Abstract
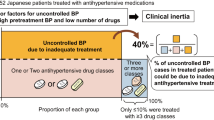
The aim of this study was to determine the clinical characteristics of patients with resistant hypertension (RH) and predictors among elderly Korean hypertensives. This prospective, multi-center, observational study evaluated 2439 elderly hypertensive patients between December 2008 and November 2011, who visited secondary hypertension clinics for high blood pressure (BP). Patients were categorized as resistant if their BP was ⩾140/90 mm Hg and if they reported using antihypertensive medications from three different drug classes, including a diuretic or drugs from ⩾4 antihypertensive drug classes, regardless of BP. Characteristics of patients with RH were compared with those of patients who were controlled with one or two antihypertensive medications after 6-month antihypertensive treatment. In comparison with 837 patients with non-RH, 404 patients with RH were more likely to be aware of their status of high BP before enrollment and have a high baseline systolic BP ⩾160 mm Hg, microalbuminuria, high body mass index (BMI) ⩾24 kg m−2 and diabetes mellitus (DM). In drug-naive patients, awareness of hypertension at baseline was the only independent predictor for RH. In elderly Korean hypertensives, BMI (⩾24 kg m−2), baseline systolic BP (⩾160 mm Hg), microalbuminuria, DM and awareness of hypertension showed an association with RH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117 (25): e510–e526.
Persell SD . Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 2011; 57 (6): 1076–1080.
Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC . Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 2011; 124 (9): 1046–1058.
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012; 125 (13): 1635–1642.
de Souza F, Muxfeldt ES, Salles GF . Prognostic factors in resistant hypertension: implications for cardiovascular risk stratification and therapeutic management. Expert Rev Cardiovasc Ther 2012; 10 (6): 735–745.
de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens 2012; 30 (6): 1211–1216.
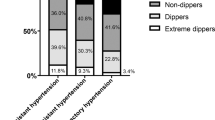
de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 2011; 57 (5): 898–902.
Anwar YA, Giacco S, McCabe EJ, Tendler BE, White WB . Evaluation of the efficacy of the Omron HEM-737 IntelliSense device for use on adults according to the recommendations of the Association for the Advancement of Medical Instrumentation. Blood Press Monit 1998; 3 (4): 261–265.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111 (5): 697–716.
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 2006; 145 (4): 247–254.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42 (6): 1206–1252.
Sarafidis PA, Bakris GL . State of hypertension management in the United States: confluence of risk factors and the prevalence of resistant hypertension. J Clin Hypertens (Greenwich) 2008; 10 (2): 130–139.
Gupta AK, Nasothimiou EG, Chang CL, Sever PS, Dahlof B, Poulter NR . Baseline predictors of resistant hypertension in the Anglo-Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high-risk. J Hypertens 2011; 29 (10): 2004–2013.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. 2007 guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007; 28 (12): 1462–1536.
Salles GF, Cardoso CR, Pereira VS, Fiszman R, Muxfeldt ES . Prognostic significance of a reduced glomerular filtration rate and interaction with microalbuminuria in resistant hypertension: a cohort study. J Hypertens 2011; 29 (10): 2014–2023.
Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES . Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis 2011; 216 (1): 199–204.
Jury DR, Mikkelsen DJ, Glen D, Dunn PJ . Assessment of Micral-Test microalbuminuria test strip in the laboratory and in diabetic outpatients. Ann Clin Biochem 1992; 29 (Pt 1): 96–100.
Spooren PF, Lekkerkerker JF, Vermes I . Micral-Test: a qualitative dipstick test for micro-albuminuria. Diabetes Res Clin Pract 1992; 18 (2): 83–87.
Bangstad HJ, Try K, Dahl-Jorgensen K, Hanssen KF . New semiquantitative dipstick test for microalbuminuria. Diabetes Care 1991; 14 (11): 1094–1097.
Redon J, Coca A, Lazaro P, Aguilar MD, Cabanas M, Gil N et al. Factors associated with therapeutic inertia in hypertension: validation of a predictive model. J Hypertens 2010; 28 (8): 1770–1777.
Acknowledgements
The HIT study was supported by Sanofi, Korea by providing web pages/server and collecting patients’ data.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Choi, SW., Kim, MK., Han, S. et al. Apparent treatment-resistant hypertension among elderly Korean hypertensives: an insight from the HIT registry. J Hum Hypertens 28, 201–205 (2014). https://doi.org/10.1038/jhh.2013.76
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2013.76
Keywords
This article is cited by
-
Resistant hypertension: consensus document from the Korean society of hypertension
Clinical Hypertension (2023)