Abstract
Spinal muscular atrophy (SMA) is an autosomal recessive neuromuscular disorder characterized by progressive loss of motor neurons in the spinal cord. Approximately 95% of SMA patients have a homozygous deletion of the survival motor neuron 1 (SMN1) gene, whereas 5% harbor compound heterozygous mutations such as an SMN1 deletion allele and an intragenic mutation in the other SMN1 allele. It is difficult to detect intragenic mutations in SMN1 because of the high degree of homology shared between SMN1 and SMN2. Current methods analyze a restricted region from exon 2a to exon 7 in SMN1. We propose a new, efficient long-range polymerase chain reaction (PCR) method for detecting intragenic mutations in SMN1 (exon 1–8) and hybrid SMN genes. We analyzed 20 unrelated SMA patients using SMN copy number analysis, and the new long-range PCR method followed by sequencing. We thus confirmed a novel mutation in SMN1 exon 1 (c.5C>T) in three patients with SMA type III who also had an SMN1 deletion allele. Moreover, we confirmed three hybrid SMN gene types in eight patients. We report a novel SMN1 mutation responsible for a relatively mild SMA phenotype and three hybrid SMN gene types in patients with SMA type III.
Similar content being viewed by others
Introduction
Spinal muscular atrophy (SMA) is an autosomal recessive neuromuscular disorder characterized by degeneration of anterior horn cells in the spinal cord, leading to progressive proximal muscle weakness and atrophy.1 Disease incidence has been estimated at 1 in 6000–10 000 live births, with a carrier frequency of 1 in 40–60.2, 3 SMA is a lower motor neuron disease and is clinically classified into four phenotypes: childhood-onset types I–III and adult-onset type IV.4 SMA type I (also known as Werdnig–Hoffmann disease; OMIM 253300) is the most severe form, with onset before the age of 6 months. Unable to sit without support, patients must be ventilated to survive after the age of 2 years. SMA type II (OMIM 253550) is the intermediate form, with onset before the age of 18 months; patients with this form of SMA never gain the ability to stand and walk. SMA type III (also known as Kugelberg–Welander disease; OMIM 253400) is a mild form, with onset after the age of 18 months; patients are able to walk early in the disease course, but lose this ability as the disease progresses.5 Adult-onset SMA is referred to as SMA type IV (OMIM 271150) and manifests after the age of 20.4
SMA is caused by deletion of the survival motor neuron (SMN) gene located on chromosome 5 (5q13). SMN is present in two homologous copies, a telomeric SMN1 and a centromeric SMN2; the difference between these two genes is only five base pairs.6 Both SMN genes encode the SMN protein, which has a role in pre-messenger RNA (mRNA) splicing in the anterior horn cells in the spinal cord.7 Although transcription of SMN1 produces full-length mRNA, transcription of SMN2 yields only 15% full-length mRNA, whereas 85% of the mRNA is incomplete (lacking exon 7).4
SMN1 is the SMA-determining gene; ~95% of patients have homozygous disruptions of SMN1 owing to deletion or conversion of SMN1 to SMN2.8, 9 Homozygous deletions of SMN1 exon 7 are the result of a gene conversion of SMN1 to SMN2, yielding a hybrid SMN gene.10, 11 Approximately 5% of patients are compound heterozygotes with a deletion and an intragenic mutation in one SMN1 allele.12 SMN2 copy numbers also vary among patients and are associated with disease severity.13, 14, 15
If no SMN1 deletion is detected in a patient with suspected SMA, SMN1 copy number analysis and intragenic mutation screening should be performed.16 Real-time polymerase chain reaction (PCR) and multiplex ligation-dependent probe amplification are used to analyze SMN1 copy number. Intragenic mutation screening of SMN1 should be performed to determine whether SMN1 or SMN2 carries any intragenic mutations, because the sequences are largely homologous. Current methods include reverse-transcription PCR of mRNA or long-range PCR of genomic DNA, both of which have limitations.6, 14, 17, 18 It can be difficult to construct SMN1 complementary DNA because of the low expression level of SMN1 mRNA in peripheral blood leukocytes. Moreover, the current method does not detect intronic mutations. Although strategies have been developed to overcome some of the problems associated with this method, it remains limited to a restricted region (13.2 kb) from exon 2a to exon 7 in SMN1 (20 kb). Therefore, the current method cannot be used to analyze upstream regions such as the 5′-untranslated region and exon 1 or regions associated with the hybrid SMN gene, such as exon 7, intron 7 and exon 8.
We have developed a more efficient and broadly applicable method using long-range PCR for specific amplification of SMN1. This new method was evaluated using controls and a sample from a previously reported patient with SMA type I, who is a confirmed compound heterozygote for SMN1, with one deleted SMN1 allele and an intragenic mutation (c.275G>C, p.W92S) in the other allele.19 We identified a novel missense mutation in SMN1 exon 1 (c.5C>T), leading to an alanine-to-valine substitution at amino acid 2 (p.A2V) in three Japanese patients with SMA type III. We also identified three hybrid SMN gene types in eight Japanese patients with homozygous deletions of SMN1 exon 7.
Materials and methods
Ethics statement
This study was approved by the Ethics Committee of Tokyo Women’s Medical University and was performed with the written informed consent of all patients.
Patients
We analyzed 10 controls and 20 unrelated patients with SMA type I (n=1), type III (n=18) and type IV (n=1). All patients met the diagnostic criteria for proximal SMA established by the International Consortium for SMA.5 Some patients did not clearly fit a single category; for those patients, we assigned SMA type by giving priority to each patient’s highest function over age of onset. Our new method was evaluated in Patient 9 with SMA type I. Patient 9, as reported previously,19 was known to be compound heterozygous for SMN1, with one deleted SMN1 allele and the other allele containing an intragenic mutation (c.275G>C, p.W92S). The remaining 19 patients (patients 1–8 and 10–20) were analyzed to demonstrate and characterize the presence of homozygous or heterozygous deletions in SMN1 exon 7, intragenic mutations and hybrid SMN genes. Family members 1–1 and 1–2 were analyzed as part of our evaluation of Patient 10.
DNA extraction and SMN1 deletion test
Genomic DNA was extracted from peripheral blood leukocytes using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) and adjusted to a final concentration of 100 ng μl−1. The SMN1 exon 7 deletion was detected by PCR-restriction fragment length polymorphism.6, 20
SMN copy number analysis using the multiplex ligation-dependent probe amplification method
We used the SALSA multiplex ligation-dependent probe amplification KIT P021-A1 SMA (MRC-Holland, Amsterdam, Netherlands) to determine SMN copy numbers. This kit contains a mixture of probes specific to exon 7 of the SMN1 (NM_000344) and SMN2 genes (NM_017411); exon 8 of the SMN1 and SMN2 genes; exons 1, 4, 6 and 8 of the SMN1 and SMN2 genes; and probes for genes located near SMN (for example, the NAIP and H4F5 (SERF1) genes); other chromosomes; and reference probes. After multiplex ligation-dependent probe amplification, DNA fragments were analyzed on an ABI 3130 Genetic Analyzer (Applied Biosystems, Foster City, CA, USA) with GeneMapper software v4.1 (Applied Biosystems).
Specific amplification of SMN1 by long-range PCR
Conventional long-range PCR was performed using a specific SMN1 exon 7 reverse primer to amplify a 13.2-kb region that includes exons 2a–7 of SMN1. Our new long-range PCR (nLR-PCR) method for specific amplification of SMN1 was performed using forward primer hybridization—654 bp from the transcription initiation site and a specific SMN1 exon 8 reverse primer to amplify a 28.2-kb region that includes exons 1–8 of SMN1 (Figure 1). The reaction was performed with KOD FX Neo polymerase (TOYOBO, Osaka, Japan) by step-down cycle PCR in a 50 μl reaction volume, with 25 μl of 2 × PCR Buffer, 0.4 mM of each dNTP, 0.15 μM of each primer (SMN_FL_(ex1-654)_F and SMN_FL_ex8_R), 1 U of polymerase and 100 ng of genomic DNA (Supplementary Table 1). nLR-PCR was performed as follows: initial denaturation at 94 °C for 2 min, followed by 5 cycles of denaturation at 98 °C for 10 s, annealing and extension at 71.2 °C for 15 min, followed by 5 cycles of denaturation at 98 °C for 10 s, annealing and extension at 69.2 °C for 15 min, followed by 5 cycles of denaturation at 98 °C for 10 s, annealing and extension at 67.2 °C for 15 min, and 20 cycles of denaturation at 98 °C for 10 s, annealing and extension at 65.2 °C for 15 min and a final extension at 65.2 °C for 7 min. Expected 28.2-kb products were confirmed by 0.7% agarose gel electrophoresis. Amplified nLR-PCR products were excised, extracted with the QIAEX II Gel Extraction Kit (Qiagen) and eluted in 20 μl of elution buffer. The nLR-PCR products were quantified using the ImageJ (NIH) software.
Strategy for specific amplification of SMN1 by long-range PCR. SMN1 and SMN2 lie, respectively, on the telomeric and centromeric halves of an inverted duplication in chromosome region 5q13. Long-range PCR (13.2 kb) of the region including exons 2a–7 of SMN1 was reported by Clermont et al.17 The new long-range PCR (28.2 kb) encompasses the region including exons 1(-654)–8 of SMN1. We specifically amplified SMN1 using the 1-base difference in exon 8. A full color version of this figure is available at the Journal of Human Genetics online.
Intragenic mutations and hybrid SMN gene analysis by sequencing
We used 1 μl of the purified nLR-PCR product as a template to amplify each SMN1 exon by nested PCR. Supplementary Table 1 lists the sequencing PCR primers and their annealing temperatures. Amplification of exon 1 was performed with KOD FX polymerase (TOYOBO) by two-step cycle PCR in a 25 μl reaction volume, with 12.5 μl of 2 × PCR Buffer, 0.4 mM of each dNTP, 0.4 μM of each primer, 0.5 U of polymerase and 1 μl of template (Supplementary Table 1). PCR was performed under the following conditions: initial denaturation at 94 °C for 2 min, followed by 35 cycles of denaturation at 98 °C for 10 s and annealing and extension at 68 °C for 45 s. Other targets were amplified using the Ex Taq polymerase (TAKARA) by three-step cycle PCR in a 25 μl reaction volume with 2.5 μl of 10 × Ex Taq Buffer, 0.2 mM of each dNTP, 0.4 μM of each primer, 1.25 U of polymerase and 1 μl of template (Supplementary Table 1). PCR was performed under the following conditions: initial denaturation at 95 °C for 2 min, followed by 30 cycles of denaturation at 95 °C for 30 s, annealing at 60 °C for 30 s and extension at 72 °C for 45 s, followed by a final extension at 72 °C for 5 min. Each SMN1 exon product was purified with the QIAquick PCR Purification Kit (Qiagen) and sequenced on an ABI 3130 Genetic Analyzer (Applied Biosystems) using the BigDye Terminator v3.1 Cycle Sequencing Kit. Mutations reported here have been submitted to a Leiden Open Variation Database (http://www.LOVD.nl/SMN1).
Family analysis
Family members 1–1 and 1–2 were the mother and younger brother of Patient 10, respectively. Copy number and sequencing analyses were performed for all family members of Patient 10.
In silico analysis
The Polyphen-2 (http://genetics.bwh.harvard.edu/pph2/), SIFT (http://sift.jcvi.org/) and Align-GVGD (http://agvgd.iarc.fr/) classification tools were used to determine the amino-acid changes that were most likely to be responsible for the loss of protein function.21, 22 The dbSNP (http://www.ncbi.nlm.nih.gov/SNP/), 1000 Genome Project databases (http://www.1000genomes.org) and Human Genetic Variation Database (http://www.genome.med.kyoto-u.ac.jp/SnpDB/index.html) were used to determine whether the identified variants are polymorphisms.
Results
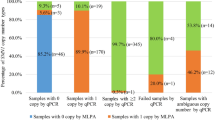
SMN1 deletion test and SMN copy number analysis
The SMN1 deletion test and SMN1 copy number analysis in 20 patients with SMA type I, SMA type III or SMA type IV revealed the absence of SMN1 exon 7 in all of these patients (Supplementary Table 2). The overall distribution of deletion types was as follows: eight patients with homozygous deletion of SMN1 exons 7 and 8 (patients 1–8); four patients with heterozygous deletion of SMN1 exons 7 and 8 (patients 9–12); and eight patients with homozygous absence of SMN1 exon 7 but not exon 8 (patients 13–20). Regarding the NAIP and H4F5 (SERF1) genes located near SMN, the overall distribution of deletion types was as follows: one patient with homozygous deletion of NAIP exon 5 (patient 1); eight patients with heterozygous deletion of NAIP exon 5 (patients 2, 6, 8, 10–12, 15 and 16); three patients with heterozygous deletion of H4F5 (SERF1 exon 1) (patients 10–12).
Specific SMN1 analysis by long-range PCR
Eight control subjects (controls 1–8) had two SMN1 copies and eight patients (patients 1–8) had SMN1 deletions. Products, 28.2-kb in size, were confirmed for all controls, whereas the bands were faint in the patients (Figure 2a). Band intensity for the controls was four times higher than that for the patients (patients 1 and 2 or patients 3–8 versus controls 6–8; P<0.05; Figure 2b). Controls 1 and 2 had the SMN2 deletion and, therefore, their samples produced the highest-intensity bands (controls 1 and 2 versus controls 6–8; P<0.05). SMN1 intron 6, exon 7 and intron 7 were amplified from the nLR-PCR products by nested PCR using SMN-ex7-F and R primers and sequenced to verify SMN1 specificity (Figure 2c).
Evaluation of new method. SMN1-specific amplifications from exon 1(-654) to exon 8 (28.2 kb) are shown. (a) Controls 1–8 yielded 28.2-kb amplicons, whereas there were few signs of amplification in patients 1–8. Copy numbers of SMN1 and SMN2 exon 8 determined by MLPA are shown at the bottom of each line. M, molecular weight marker (TAKARA 2.5-kb DNA Ladder). (b) Quantification of nLR-PCR products. Average intensities of samples with the same SMN2 exon 8 copy number are presented. P-value: Student’s t-test. *Patients 1 and 2 versus controls 6–8; P=0.001, **Patients 3–8 versus controls 6–8; P=0.000, ***controls 1 and 2 versus controls 6–8; P=0.002. (c) SMN1 specificity was confirmed by the presence of intron 6, exon 7 and intron 7 sequences. A full color version of this figure is available at the Journal of Human Genetics online.
Direct sequencing for patient 9, who had a known intragenic mutation (c.275G>C), revealed an abnormal heteroduplex signal (blue: Cytosine, black: Guanine) in exon 3 of SMN1 and SMN2 (Figure 3). Only SMN1 regions were isolated by nLR-PCR; SMN1 exon 3 was amplified by nested PCR from nLR-PCR products; sequencing revealed increased cytosine and decreased guanine signal intensity (Figure 3). These findings suggested that the cytosine was derived from SMN1 and that the mutation was present in SMN1 exon 3. SMN1 intron 6, exon 7 and intron 7 were also sequenced from nLR-PCR products to verify SMN1 specificity (data not shown).
Detection of an intragenic mutation in a patient with type I SMA. Patient 9 was compound heterozygous for SMN1, with one deleted SMN1 allele and an intragenic mutation (c.275G>C, p.W92S) in the other allele.19 This patient had three SMN2 copies. (Left) Direct sequencing of SMN1 and SMN2; (Right) Sequencing of SMN1 exon 3 isolated by the new long-range PCR technique is shown.
Novel intragenic mutations and family analysis
We screened all exons of SMN for novel intragenic mutations by direct sequencing of genomic DNA. Patient 10, with SMA type III, produced an abnormal heteroduplex signal (blue: Cytosine, red: Thymine) in exon 1 of SMN1 and SMN2 (Figure 4a), indicating an intragenic mutation in exon 1 of SMN1 or SMN2. To determine which gene carried the mutation, SMN1 nLR-PCR products were sequenced. A single signal (red: Thymine) was detected in SMN1 exon 1, indicating that the mutation was present in SMN1 exon 1 (Figure 4a). This C-to-T mutation at position 5 (c.5C>T) causes an alanine-to-valine substitution at amino acid 2 (p.A2V). This mutation was also identified in patients 11 and 12 (Table 1).
Identification of an intragenic mutation in SMN1. (a) Patient 10 had one copy each of SMN1 and SMN2. (Left) Direct sequencing for SMN1 and SMN2 results are shown; (Right) direct sequencing of SMN1 (right) exon 1 isolated by the new long-range PCR technique. The sequence revealed a c.5C>T mutation (red signal), leading to an alanine-to-valine substitution (p.A2V). (b) Patient 10 family analysis. The mutation in patient 10 (II–1) was absent from I–2 and II–2.
Copy number and sequencing analyses were performed for relatives (family members 1–1 and 1–2) of patient 10 (II–1; Figure 4b). The mother (family member 1–1; I–2) carried one SMN1 copy and two SMN2 copies; the brother (family member 1–2; II–2) carried two SMN1 copies and two SMN2 copies. The intragenic mutation in patient 10 (II–1) was absent in both of the family members tested (I–2 and II–2).
In silico analysis
The c.5C>T mutation was not observed in 100 normal Japanese control samples. This mutation has not been documented in dbSNP, the 1000 Genome Project database or the Human Genetic Variation Database. Functional significance was evaluated by referring to Polyphen-2, SIFT and Align-GVGD. The mutation was assumed to lead to a hazardous change in protein function because all three programs returned evaluations of ‘DAMAGING (PolyPhen-2 score: 0.939, SIFT score: 0.01)’ and ‘Class C65.’ Thus, in SMA type III patients 10–12, the disease was attributed to a compound heterozygous mutation, including one SMN1 allele deletion and a c.5C>T mutation in the other SMN1 allele.
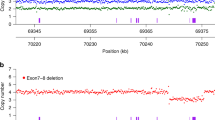
Hybrid SMN gene analysis by long-range PCR and sequencing
Patients 13–20, carrying a homozygous absence of SMN1 exon 7 but not exon 8, were assessed for the presence of the hybrid SMN gene by nLR-PCR amplification of a region that includes exons 1–8 of SMN1 and by sequencing of intron 6, exon 7 and intron 7 (Table 2). We identified three hybrid SMN gene types (Table 2 and Figure 5). The sequences of hybrid SMN intron 6, exon 7, intron 7 and exon 8 were as follows: patient 13, aTagG; patients 14 and 16–20, aTggG; and patient 15, gTaaG.
Schematic illustration of the three hybrid SMN gene types. Dotted line frames indicate SMN2 sequences and show the SMN1-to-SMN2 gene conversion. The type A hybrid was most common. The sequences of intron 6, exon 7 and intron 7 were of SMN2 origin, whereas that of exon 8 was of SMN1 origin. Type B was a complex form. The sequences of intron 6, exon 7 and intron 7 (only one base) were of SMN2 origin, whereas those of intron 7 (the other base) and exon 8 were of SMN1 origin. Type C had the fewest changes: the exon 8 sequence was of SMN2 origin, whereas intron 6, intron 7 and exon 8 were of SMN1 origin. A full color version of this figure is available at the Journal of Human Genetics online.
Discussion
We developed an efficient and broadly applicable LR-PCR method to detect intragenic mutations in SMN1 (Figure 1). Without the need for complementary DNA cloning, this new method makes it possible to analyze all exons and introns of SMN1, the 5′- and 3′-untranslated regions, the promoter region, small or large insertions and deletions and hybrid SMN genes. Differences between controls and patients were clear (P<0.05), and the specificity was verified (Figure 2b). The absence of SMN2, which inhibits SMN1-specific PCR, yielded an increase in nLR-PCR products (controls 1 and 2). Even when there are more copies of SMN2 than of SMN1, specific SMN1 regions can be amplified using our nLR-PCR method (Figure 3).
We identified a novel mutation in exon 1 of SMN1, c.5C>T, in three unrelated patients (patients 10–12) with SMA type III (Table 1). With the currently available methods, it was difficult to isolate only SMN1 mRNA from the peripheral blood leukocytes of patient 11 (data not shown). We attribute this to low SMN1 mRNA expression in these cells. Although family members of patient 10 (II–1) were shown by sequencing analysis to have the c.5C>T mutation, the intragenic mutation in patient 10 (II–1) was absent in both her mother (I–2) and her brother (II–2; Figure 4b). Patient 10 (II–1) had inherited the allele deletion from her mother, whereas the intragenic mutation had either been inherited from her father or occurred de novo.
The c.5C>T mutation was evaluated as a hazardous change based on in silico analysis results. The c.5C>T mutation was not registered in dbSNP, the 1000 Genome Project database or the Human Genetic Variation Database and might be a Japanese-specific variant. Consistent with these results, one patient with SMA type II and two with SMA type III with c.5C>G (p.A2G, dbSNP: rs75030631) mutations were reported previously.23 These patients had only one SMN2 copy and presented with similar mild symptoms. There are also reports of SMA associated with the c.5C>G mutation. Although SMN knockout mice with low SMN2 copy numbers have severe SMA, phenotype rescue could be achieved in a transgene SMN A2G missense mutant.24 Although SMN knockout is lethal in mouse embryos,25 SMN(A2G) SMA mice exhibit the onset of motor neuron loss, resulting in mild SMA. The SMN A2G mutation inhibits self-association and affects SMN binding, probably by disrupting the formation of SMN oligomers. Because the effect of p.A2G is mild, it is associated with a later age of onset and relatively mild symptoms. The p.A2V variation is likely similar to p.A2G in its phenotypic effect.
Phenotypic effects might differ among intragenic mutation positions. For example, despite patient 9, with W92S(c.275G>C) and SMN1 deletion, having three copies of SMN2, the relatively severe SMA type I phenotype was evident.19 This mutation was located in exon 3, corresponding to the Tudor domain, an essential region for interaction of SMN with fundamental components of multiple nuclear RNA-protein complexes. This mutation impaired the interaction of SMN with various proteins. Therefore, mutations of this type may have a critical impact on SMN function.
Furthermore, the positions of intragenic mutations seemed to have more profound effects on phenotype than the size of the deletion in one allele. Although patients 10–12 had a large deletion including NAIP and H4F5 in one allele (Supplementary Table 2), their phenotype was mild. On the other hand, although patient 9 had a small deletion including only SMN1, the SMA phenotype was severe.
We identified three hybrid SMN gene types in eight patients. Our method enables the direct isolation and sequencing of the entire hybrid SMN gene. We identified large (Type A), complex (Type B) and small conversions (Type C; Figure 5). SMA in patients 13–17 was associated with a deletion in SMN1 exon 7 combined with an SMN1-to-SMN2 conversion. SMA in patients 17–20 was associated with a homozygous SMN1-to-SMN2 conversion. Cusco et al.26 reported milder symptoms in patients with a homozygous conversion than in those with a combination of deletion and conversion. An association between disease severity and conversion has been described27 but other reports suggest no such association.28 Increased copy numbers of hybrid SMN genes and SMN2 have also been reported to be associated with disease severity.26 In this study, similar to a report by Cusco et al.,26 symptoms were found to be milder in patients 18–20, who carry a homozygous conversion. Patient 15 had late onset of disease compared with patients 13, 14, 16 and 17, and could walk, thereby showing disease severity similar to that of patients 18–20. We speculate that milder symptoms might correspond to small conversion regions, like Type C.
Patients with a missense mutation or hybrid SMN gene, identified in this study, showed relatively mild SMA symptoms. As to possible mechanisms underlying such mild symptoms, Prior et al.29 reported that the c.859G>C substitution in the SMN2 gene is a positive modifier of the SMA phenotype. Although we tested for the c.859G>C change in the SMN2 gene, neither the missense mutation nor the hybrid SMN gene (patients 9–20) carried this change.
Our method for detecting intragenic mutations of SMN1 by nLR-PCR (28.2 kb) is more efficient and has broader applications than the currently available methods. In three patients for whom current methods yielded no results, we identified a c.5C>T mutation in SMN1 exon 1. In eight patients with a hybrid SMN gene, we identified three hybrid types. This new method allows analysis of previously undetectable regions, including all introns and exons of SMN1 and all SMN genes. Furthermore, we identified three distinct hybrids.
References
Crawford, T. O. & Pardo, C. A. The neurobiology of childhood spinal muscular atrophy. Neurobiol. Dis. 3, 97–110 (1996).
Ogino, S. & Wilson, R. B. Genetic testing and risk assessment for spinal muscular atrophy (SMA). Hum. Genet. 111, 477–500 (2002).
Prior, T. W., Snyder, P. J., Rink, B. D., Pearl, D. K., Pyatt, R. E., Mihal, D. C. et al. Newborn and carrier screening for spinal muscular atrophy. Am. J. Med. Genet. A 152A, 1608–1616 (2010).
Kolb, S. J. & Kissel, J. T. Spinal muscular atrophy: a timely review. Arch. Neurol. 68, 979–984 (2011).
Zerres, K. & Davies, K. E. 59th ENMC International Workshop: Spinal Muscular Atrophies: recent progress and revised diagnostic criteria 17-19 April 1998, Soestduinen, The Netherlands. Neuromuscul. Disord. 9, 272–278 (1999).
Lefebvre, S., Burglen, L., Reboullet, S., Clermont, O., Burlet, P., Viollet, L. et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell 80, 155–165 (1995).
Pellizzoni, L., Charroux, B. & Dreyfuss, G. SMN mutants of spinal muscular atrophy patients are defective in binding to snRNP proteins. Proc. Natl Acad. Sci. USA 96, 11167–11172 (1999).
Burghes, A. H. When is a deletion not a deletion? When it is converted. Am. J. Hum. Genet. 61, 9–15 (1997).
Wirth, B. An update of the mutation spectrum of the survival motor neuron gene (SMN1 in autosomal recessive spinal muscular atrophy (SMA). Hum. Mutat. 15, 228–237 (2000).
Hahnen, E., Forkert, R., Marke, C., Rudnik-Schoneborn, S., Schonling, J., Zerres, K. et al. Molecular analysis of candidate genes on chromosome 5q13 in autosomal recessive spinal muscular atrophy: evidence of homozygous deletions of the SMN gene in unaffected individuals. Hum. Mol. Genet. 4, 1927–1933 (1995).
van der Steege, G., Grootscholten, P. M., Cobben, J. M., Zappata, S., Scheffer, H., den Dunnen, J. T. et al. Apparent gene conversions involving the SMN gene in the region of the spinal muscular atrophy locus on chromosome 5. Am. J. Hum. Genet. 59, 834–838 (1996).
Alias, L., Bernal, S., Fuentes-Prior, P., Barcelo, M. J., Also, E., Martinez-Hernandez, R. et al. Mutation update of spinal muscular atrophy in Spain: molecular characterization of 745 unrelated patients and identification of four novel mutations in the SMN1 gene. Hum. Genet. 125, 29–39 (2009).
Feldkotter, M., Schwarzer, V., Wirth, R., Wienker, T. F. & Wirth, B. Quantitative analyses of SMN1 and SMN2 based on real-time lightCycler PCR: fast and highly reliable carrier testing and prediction of severity of spinal muscular atrophy. Am. J. Hum. Genet. 70, 358–368 (2002).
Harada, Y., Sutomo, R., Sadewa, A. H., Akutsu, T., Takeshima, Y., Wada, H. et al. Correlation between SMN2 copy number and clinical phenotype of spinal muscular atrophy: three SMN2 copies fail to rescue some patients from the disease severity. J. Neurol. 249, 1211–1219 (2002).
Cusco, I., Barcelo, M. J., Rojas-Garcia, R., Illa, I., Gamez, J., Cervera, C. et al. SMN2 copy number predicts acute or chronic spinal muscular atrophy but does not account for intrafamilial variability in siblings. J. Neurol. 253, 21–25 (2006).
Lunn, M. R. & Wang, C. H. Spinal muscular atrophy. Lancet 371, 2120–2133 (2008).
Clermont, O., Burlet, P., Benit, P., Chanterau, D., Saugier-Veber, P., Munnich, A. et al. Molecular analysis of SMA patients without homozygous SMN1 deletions using a new strategy for identification of SMN1 subtle mutations. Hum. Mutat. 24, 417–427 (2004).
Zapletalova, E., Hedvicakova, P., Kozak, L., Vondracek, P., Gaillyova, R., Marikova, T. et al. Analysis of point mutations in the SMN1 gene in SMA patients bearing a single SMN1 copy. Neuromuscul. Disord. 17, 476–481 (2007).
Kotani, T., Sutomo, R., Sasongko, T. H., Sadewa, A. H., Gunadi, Minato, T., Fujii, E. et al. A novel mutation at the N-terminal of SMN Tudor domain inhibits its interaction with target proteins. J. Neurol. 254, 624–630 (2007).
van der Steege, G., Grootscholten, P. M., van der Vlies, P., Draaijers, T. G., Osinga, J., Cobben, J. M. et al. PCR-based DNA test to confirm clinical diagnosis of autosomal recessive spinal muscular atrophy. Lancet 345, 985–986 (1995).
Adzhubei, I. A., Schmidt, S., Peshkin, L., Ramensky, V. E., Gerasimova, A., Bork, P. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Ng, P. C. & Henikoff, S. SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res. 31, 3812–3814 (2003).
Parsons, D. W., McAndrew, P. E., Iannaccone, S. T., Mendell, J. R., Burghes, A. H., & Prior, T. W. Intragenic telSMN mutations: frequency, distribution, evidence of a founder effect, and modification of the spinal muscular atrophy phenotype by cenSMN copy number. Am. J. Hum. Genet. 63, 1712–1723 (1998).
Monani, U. R., Pastore, M. T., Gavrilina, T. O., Jablonka, S., Le, T. T., Andreassi, C. et al. A transgene carrying an A2G missense mutation in the SMN gene modulates phenotypic severity in mice with severe (type I) spinal muscular atrophy. J. Cell. Biol. 160, 41–52 (2003).
Schrank, B., Gotz, R., Gunnersen, J. M., Ure, J. M., Toyka, K. V., Smith, A. G. et al. Inactivation of the survival motor neuron gene, a candidate gene for human spinal muscular atrophy, leads to massive cell death in early mouse embryos. Proc. Natl Acad. Sci. USA 94, 9920–9925 (1997).
Cusco, I., Barcelo, M. J., del Rio, E., Martin, Y., Hernandez-Chico, C., Bussaglia, E. et al. Characterisation of SMN hybrid genes in Spanish SMA patients: de novo, homozygous and compound heterozygous cases. Hum. Genet. 108, 222–229 (2001).
DiDonato, C. J., Ingraham, S. E., Mendell, J. R., Prior, T. W., Lenard, S., Moxley, R. T. 3rd et al. Deletion and conversion in spinal muscular atrophy patients: is there a relationship to severity? Ann. Neurol. 41, 230–237 (1997).
Hahnen, E., Schonling, J., Rudnik-Schoneborn, S., Zerres, K. & Wirth, B. Hybrid survival motor neuron genes in patients with autosomal recessive spinal muscular atrophy: new insights into molecular mechanisms responsible for the disease. Am. J. Hum. Genet. 59, 1057–1065 (1996).
Prior, T. W., Krainer, A. R., Hua, Y., Swoboda, K. J., Snyder, P. C., Bridgeman, S. J. et al. A positive modifier of spinal muscular atrophy in the SMN2 gene. Am. J. Hum. Genet. 85, 408–413 (2009).
Yamamoto, T., Sato, H., Lai, P. S., Nurputra, D. K., Harahap, N. I., Morikawa, S. et al. Intragenic mutations in SMN1 may contribute more significantly to clinical severity than SMN2 copy numbers in some spinal muscular atrophy (SMA) patients. Brain Dev. 36, 914–920 (2014).
Acknowledgements
We are grateful to the patients who agreed to participate in this study. We thank Drs T Yamamoto, S Morikawa, S Sawai, H Nakajima, T Oshita and T Kurashige for their valuable contributions to this study. This work was supported by Grants-in-Aid from the Research Committee of Spinal Muscular Atrophy, the Ministry of Health, Labour and Welfare of Japan (to KS). This work was also supported by the Global COE program, Multidisciplinary Education and Research Center for Regenerative Medicine (MERCREM) from the Ministry of Education, Culture, Sports Science, and Technology (MEXT), Japan (to YK and KS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Kubo, Y., Nishio, H. & Saito, K. A new method for SMN1 and hybrid SMN gene analysis in spinal muscular atrophy using long-range PCR followed by sequencing. J Hum Genet 60, 233–239 (2015). https://doi.org/10.1038/jhg.2015.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2015.16
This article is cited by
-
Optimized MLPA workflow for spinal muscular atrophy diagnosis: identification of a novel variant, NC_000005.10:g.(70919941_70927324)del in isolated exon 1 of SMN1 gene through long-range PCR
BMC Neurology (2024)
-
Detection of SMN1 to SMN2 gene conversion events and partial SMN1 gene deletions using array digital PCR
neurogenetics (2021)
-
Target resequencing of neuromuscular disease-related genes using next-generation sequencing for patients with undiagnosed early-onset neuromuscular disorders
Journal of Human Genetics (2016)
-
Validation of a high resolution NGS method for detecting spinal muscular atrophy carriers among phase 3 participants in the 1000 Genomes Project
BMC Medical Genetics (2015)