Abstract
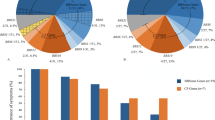
Retinitis pigmentosa (RP) is a highly heterogeneous genetic disease. The USH2A gene, which accounts for approximately 74–90% of Usher syndrome type 2 (USH2) cases, is also one of the major autosomal recessive RP (arRP) causative genes among Caucasian populations. To identify disease-causing USH2A gene mutations in Japanese RP patients, all 73 exons were screened for mutations by direct sequencing. In total, 100 unrelated Japanese RP patients with no systemic manifestations were identified, excluding families with obvious autosomal dominant inheritance. Of these 100 patients, 82 were included in this present study after 18 RP patients with very likely pathogenic EYS (eyes shut homolog) mutations were excluded. The mutation analysis of the USH2A revealed five very likely pathogenic mutations in four patients. A patient had only one very likely pathogenic mutation and the others had two of them. Caucasian frequent mutations p.C759F in arRP and p.E767fs in USH2 were not found. All the four patients exhibited typical clinical features of RP. The observed prevalence of USH2A gene mutations was approximately 4% among Japanese arRP patients, and the profile of the USH2A gene mutations differed largely between Japanese patients and previously reported Caucasian populations.
Similar content being viewed by others
Introduction
Usher syndrome (USH; Mendelian inheritance in man (MIM) 276900) is an autosomal recessive disorder characterized by retinitis pigmentosa (RP) and hearing loss, with or without vestibular dysfunction. The syndrome is clinically and genetically heterogeneous and can be clinically classified into three subtypes on the basis of severity and progression of hearing loss and the presence or absence of vestibular dysfunction.1 Specifically, USH type 2 (USH2), the most common type accounting for >50% of USH cases, is characterized by congenital mild-to-severe hearing loss and a normal vestibular response.2 The USH2A (Usher syndrome 2A) gene, which encodes usherin, accounts for approximately 80% of USH2 cases.3, 4, 5 Previous mutation analyses of the full-length USH2A coding region (exons 2–72) in Caucasian patients have revealed a frequent mutation c.2299delG (p.E767fs) in exon 13.4, 5, 6, 7, 8, 9, 10, 11, 12 In our recent analysis of the USH2A gene in Japanese USH2 patients, in which the p.E767fs mutation was not identified, we reported 19 novel mutations among 19 patients, as well as the splicing mutation c.8559-2A>G in 4 of the 19 patients, indicating that the incidence of mutations in the Japanese individuals was similar to that in Caucasian individuals, even though the mutation spectrum of the USH2A gene considerably differed between the two populations.13, 14, 15
RP (MIM 268000) is a highly heterogeneous genetic retinal degeneration characterized by night blindness and visual field constriction, which would eventually lead to severe visual impairment. The disease can be inherited via an autosomal recessive (ar), autosomal dominant (ad) or X-linked recessive mode or may occur in isolation; in fact, more than half of the cases in Japan are isolated cases.16 To date, 63 causative genes and 7 loci have been found to be associated with RP (http://www.sph.uth.tmc.edu/Retnet/; accessed 19 February 2014). The EYS (eyes shut homolog) gene encodes an ortholog of Drosophila spacemaker (spam), which is a protein essential for maintaining the photoreceptor morphology. EYS gene mutations have been detected in arRP-affected families of different ancestral origins and have been reported to account for 5–16% of arRP cases.17, 18, 19, 20, 21, 22 Mutations in the USH2A gene were also found to cause non-syndromic RP.23 Although some studies on the USH2A gene employed mostly USH patients and included a few non-syndromic RP patients,5, 24, 25 a few groups analyzed large sets of non-syndromic RP patients and reported that USH2A mutations, including the frequent mutation c.2276G>T (p.C759F), cause a substantial number of cases of non-syndromic RP in North America and Spain (7–23%).23, 26, 27, 28, 29 We previously screened all EYS gene exons in 100 unrelated Japanese RP patients and, surprisingly, found EYS gene mutations in at least 18% of the arRP patients.30 Of these 100 patients, 82 were included in the present study after 18 RP patients with very likely pathogenic (deleterious) EYS gene mutations were excluded.30 Here we report the results of our study of all USH2A exons in 82 Japanese arRP patients.
Materials and methods
Patients
We previously screened all EYS gene exons in 100 unrelated Japanese RP patients with no systemic manifestations, excluding families with obvious autosomal dominant inheritance.30 Among them, some pedigrees showed a pattern compatible with the recessive mode of inheritance, whereas other patients were considered as isolated cases. Excluding 18 RP patients with very likely pathogenic EYS gene mutations, 82 out of these 100 patients were employed in this study. An audiological examination, including pure-tone audiometry, was not performed before the mutation analysis; however, none of the patients had documented hearing loss. In addition, 200 unrelated and non-RP Japanese individuals were screened as controls to evaluate the frequency of mutations found in patient samples. Japanese patients with RP were examined at the Department of Ophthalmology, Hamamatsu University Hospital in Hamamatsu (by YH); the Department of Ophthalmology, Kobe City Medical Center General Hospital in Kobe (by MT); the Department of Ophthalmology, Institute of Biomedical Research and Innovation Hospital in Kobe (by MT); or the Department of Ophthalmology, Nagoya University Hospital in Nagoya (by MK and SU). These patients were from the areas of Tokyo to Osaka in Japan.
Ethics statements
This study was approved by the Institutional Review Board for Human Genetic and Genome Research at the four participating institutions (Hamamatsu University School of Medicine, RIKEN Center for Developmental Biology, Institute of Biomedical Research and Innovation Hospital and Nagoya University Graduate School of Medicine). All the procedures conformed to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants before the molecular genetic studies were performed.
Mutation analysis
Genomic DNA extracted from peripheral lymphocytes of patients using standard procedures was amplified by PCR using the primer sets described in Supplementary Table S1. The PCR and sequencing procedures used were described previously.30 A total of 73 exons, including a non-coding exon (exon 1) that covers the 5′ untranslated region, 71 coding exons (exons 2–72) and an alternatively spliced variant of exon 71,31 were analyzed in both sense and antisense directions. Alternatively spliced exon 71 encodes a 24-amino-acid peptide in the murine inner ear and is considered to be well conserved in humans, even though its presence in human transcripts has not yet been directly confirmed. The accession numbers for the two alternative splicing isoforms (long isoform,8 consisting of 72 exons, and longer isoform, consisting of 73 exons that included an alternatively spliced variant of exon 71) of USH2A genes were NM_206933 (long isoform) and ENST00000366943 (longer isoform). The latter is the Ensembl Transcript ID number in the Ensembl database, which is presented here, because the entry of the longer isoform was not found in the DDBJ/EMBL/GenBank database.
Assessment of pathogenicity
A sequence variant was considered pathogenic when it represented a nonsense mutation, a frameshift mutation, a deletion mutation affecting amino-acid sequences, a mutation in the first two bases of canonical intron splice donor or acceptor sites, a missense mutation affecting a conserved amino-acid residue, a previously described pathogenic mutation or a mutation identified in >2 unrelated patients and did not appear in 200 unrelated and non-RP Japanese control samples or a public single-nucleotide polymorphism (SNP) database (NCBI dbSNP database, http://www.ncbi.nlm.nih.gov/projects/SNP/; 1000 Genomes database, http://www.1000genomes.org/). In particular, a missense mutation was described as very likely pathogenic when it fulfilled at least two of the following criteria: (1) it was found together with a second variant, especially a nonsense mutation or frameshift mutation; (2) it was segregated with the disease phenotype within the family; and (3) the in silico analysis predicted a pathogenic effect.
In silico analysis to assess the pathogenicity of a missense or deletion mutation
We used the five following computational algorithms to evaluate the pathogenicity of missense mutations: SIFT (http://sift.jcvi.org/www/SIFT_seq_submit2.html), PolyPhen2 (http://genetics.bwh.harvard.edu/pph2/), PMut (http://mmb.pcb.ub.es/PMut/), SNAP (http://rostlab.org/services/snap/), and Align-GVGD (http://agvgd.iarc.fr/agvgd_input.php). The SIFT analysis results are given by a probability of 0–1; specifically, mutations with a probability ⩽0.05 are predicted to be deleterious (affect protein function), whereas those with a probability >0.05 are predicted to be tolerated. In this study, a mutation predicted to ‘affect protein function’ was considered as a suspected pathogenic mutation. Polyphen2 describes mutations as ‘benign’, ‘possibly damaging’ or ‘probably damaging’. In this study, both ‘possibly damaging’ and ‘probably damaging’ were classified as suspected pathogenic mutations. The results from the SNAP analysis are classified into ‘neutral’ or ‘non-neutral’. In this study, ‘non-neutral’ was considered as a suspected pathogenic mutation. The results from the PMut analysis are classified into ‘neutral’ or ‘pathological’. In this study, ‘pathological’ was considered as a suspected pathogenic mutation. The Align-GVGD analysis results are given by a grade from C0 to C65, where C0 is benign and C65 is most likely pathogenic. In this study, a grade of C65 was considered as a suspected pathogenic mutation.
The secondary structure of usherin was predicted by PSIPRED v3.3 on the PSIPRED server (http://bioinf.cs.ucl.ac.uk/psipred/).
Clinical evaluation
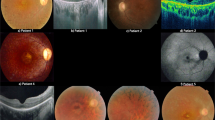
The doctors were asked to obtain as much detail as possible about the family history of patients in whom we identified very likely pathogenic mutations (RP7H, RP10H, RP15H and RP66K) and possible pathogenic mutations (RP82K and RP85N). The complete history and medical records of these four patients were reviewed. In addition, patients were also clinically evaluated by standard procedures, including spectral-domain optical coherence tomography (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany or Cirrus OCT; Carl Zeiss Meditec, Inc., Dublin, CA, USA). Electroretinograms were also performed in some cases. Audiological examination, including pure-tone audiometry, was performed for patients (RP7H, RP10H and RP15H) who consented to the study.
Results
Mutation analysis
Our mutation analysis of the USH2A gene in 82 unrelated Japanese patients revealed 5 very likely pathogenic mutations among 4 patients. A patient had only one very likely pathogenic mutation and the others had two of them (Tables 1 and 2). These very likely pathogenic mutations consisted of a deletion mutation, two splicing mutations and two missense mutations. In addition, we identified two possible pathogenic mutations in two individual patients (Tables 1 and 2).
Families with very likely pathogenic mutations
Among the four patients carrying very likely pathogenic mutations, RP7H, RP10H and RP15H each had two pathogenic mutations. In RP7H and RP15H, the two mutated alleles were considered to be located on different chromosomes (Figures 1a and c).
Pedigree and clinical examination data of patients with mutations in the USH2A gene. (a–c) Pedigrees of patients RP7H (a), RP10H (b) and RP15H (c). The genotypes are presented for p.E1199del, p.G229R, p.G2752R, p.R926C and c.8559-2A>G. The genotype of each evaluated individual is indicated below the symbol: square boxes and circles denote male and female individuals, respectively; black symbols indicate affected individuals; and slashed symbols indicate deceased individuals. The probands are indicated with arrows. NA, unavailable DNA samples. For example, c.8559-2A>G/c.8559-2A>G, homozygous mutation carriers; p.G229R/+, heterozygous carriers; +/+, individuals carrying two wild-type alleles; p.E1199del/p.G229R, individuals who were compound heterozygous for both mutations. p.G229R;p.R926C could not be segregated (See Table 1 footnote). (d–f) Right visual fields of patients RP7H (d), RP10H (e) and RP15H (f). The constriction of visual fields was found to be symmetric. The concentric constriction started in their twenties or thirties, and no effective residual visual field was observed after their fifties. (g–i) Audiograms of patients RP7H (g), RP10H (h) and RP15H (i). Circles and crosses indicate hearing thresholds of the right and left ears, respectively.
Patient RP7H was born in the Hamamatsu area and was considered as an isolated case (Figure 1a). In RP7H, the proband (II-2) was compound heterozygous for the novel missense mutation c.685G>C (p.G229R) and the novel deletion mutation c.3595_3597delGAA (p.E1199del) (Figure 1a). p.G229R was also identified in patient RP10H, who was unrelated to RP7H (Tables 1 and 2). The amino-acid residue at G229 of human USH2A was compared with those encoded by the orthologous genes of some vertebrates (bovine, dog, rat, mouse, chicken and zebrafish) and was found to be highly conserved across species (Table 2). p.G229R was predicted to be pathogenic by four different computational prediction programs (SIFT, Polyphen2, SNAP and Align-GVGD). On the other hand, p.E1199del is a 3-base pair (bp) in-frame deletion that results in the loss of the amino-acid residue E1199 in the second fibronectin type 3 domain (Figure 2). E1199 was also compared with the equivalent residue in other species’ orthologous genes and was highly conserved among mammals and chicken (Table 2). p.E1199del was analyzed by the PSIPRED program to determine its effect on the secondary structure of usherin. The predicted effect was the shortening of the beta-sheet stretch from seven contiguous amino acids (QPCVSYE-1199) to five (QPCVS-1197), which suggests that the mutation affected the normal protein structure and was pathogenic. Interestingly, we also found another missense mutation c.8254G>A (p.G2752R), which we previously found in USH2 patient C212 as one of thee candidates for probable pathogenic mutations, but we could not determine the pathogenicity because of difficulty in the segregation analysis.13 However, in this study, p.G2752R was assigned to the group of possible non-pathogenic sequence alterations (Supplementary Table S2), because it has been described in the dbSNP database (rs201863550) and the 1000 Genomes database. As shown in Figure 1a, the mutations were found to co-segregate with the disease phenotype as follows. The unaffected father (I-1) and mother (I-2) were heterozygous for p.E1199del and p.G229R, respectively, whereas the unaffected brother (II-1) carried the wild-type alleles. In addition, p.G2752R was identified in cis to p.E1199del in the unaffected father, indicating that these two mutations were genetically linked in this family.
Schematic distribution of the USH2A mutations identified in this study. Upper, usherin domains encoded by USH2A; lower, USH2A cDNA with exon boundaries. Novel very likely pathogenic mutations, novel possible pathogenic mutations and previously described mutations are shown in bold, normal and italic fonts, respectively. Identified mutations were widely distributed throughout almost the entire USH2A gene without any clear hot spot.
Patient RP10H was born in the Hamamatsu area and was considered to be an isolated case (Figure 1b). RP10H was heterozygous for two missense mutations, c.685G>C (p.G229R) and c.2776C>T (p.R926C). p.G229R, also found in RP7H, was classified as very likely pathogenic as described above. Similarly, the novel missense mutation p.R926C was predicted to be pathogenic by four different computational prediction programs (SIFT, Polyphen2, SNAP and Align-GVGD) (Table 2). Like G229, the R926 residue was also found to be highly conserved across species (Table 2). No segregation analysis could be performed in this patient owing to difficulties in collecting samples from the patient’s family. Although both these two missense mutations were considered pathogenic, we were not able to confirm whether they were located on different chromosomes (Figure 1b, Table 1).
Patient RP15H carried the homozygous c.8559-2A>G mutation; RP15H was an isolated case and his parents were second cousins from the Hamamatsu area; that is, he was the product of a consanguineous marriage (Figure 1c). The proband (II-1) was homozygous for the splicing mutation c.8559-2A>G. No segregation analysis was performed, because both parents were deceased. Although the mutation has been previously reported as disease causing in four Japanese and one Chinese USH2 patients,13, 15, 32 all of these five patients were heterozygous for c.8559-2A>G. To the best of our knowledge, this study is the first to report of a patient homozygous for the c.8559-2A>G mutation.
Patient RP66K was born in Kobe and was considered as an isolated case. In RP66K, we found the splicing mutation, c468-14G>A, which has been previously reported as disease causing in a French USH2 patient and shown to create a new AG (acceptor consensus) sequence, resulting in abnormal splicing.33
None of these five very likely pathogenic mutations was found among the Japanese controls or in a public SNP database (Table 2).
Families with novel possible pathogenic mutations
Here we report two novel missense mutations in two different patients (RP82K and RP85N), none of which was identified in 400 Japanese control alleles or a public SNP database. Patients RP82K and RP85N were born in the Kansai and Hiroshima areas, respectively, and were considered as isolated cases. RP82K and RP85N each had one novel missense mutation (p.V2386F and p.S4748F, respectively; Tables 1 and 2). The amino-acid residues of USH2A affected by the two novel missense mutations (V2386 and S4748) are not evolutionally conserved compared with those encoded by the orthologous genes of some vertebrate species (Table 2). For pathogenicity, the in silico analysis with at least two of the five different computational programs described these two mutations as pathogenic but did not exclude the possibility that these mutations were non-pathogenic (Table 2). Nevertheless, these two mutations were assigned to the group of possible pathogenic mutations, and further analyses are necessary to determine the precise nature of these mutations.
Summary of the possible non-pathogenic sequence alterations in the USH2A gene identified in this study
Overall, 78 possible sequence alterations were identified among 82 patients, and 7 of them have never been reported (Supplementary Table S2). These alterations did not fulfill the assessment of pathogenicity in this study (See Materials and methods); therefore, they were assigned to the group of possible non-pathogenic sequence alterations (Supplementary Table S2).
Clinical findings
The age of the four patients with one or two deleterious mutations ranged from 19 to 52 years at the time of diagnosis and from 37 to 60 years at the time of initial examination for this study. In addition, all the four patients had night blindness. The constriction of visual fields was found to be symmetric. The concentric constriction started in their twenties or thirties, and no effective residual visual field was observed after their fifties (Figures 1d–f). In all cases, the fundus displayed changes typical of RP, including attenuated retinal vessels and bone spicule deposits over 360° of the fundus, all of which were increased in density with age. Spectral-domain OCT images also showed a marked reduction in retinal thickness resulting from the loss of photoreceptor layers. The photoreceptor inner segment/outer segment junction was either completely absent or was only detectable at the fovea of four subjects. The electroretinographic responses were consistent with severe generalized rod-cone dysfunction. On the other hand, none of these four patients had difficulties in daily conversation. Although the hearing tests for RP7H and RP10H yielded normal results (Figures 1g and h), the test for RP15H showed moderate hearing loss, suggesting USH2 (Figure 1i).
The age of the two patients with one possible mutation (RP82K and RP85N) was 40–46 years at the time of diagnosis and 50–66 years at the time of the initial examination for this study. Both patients had night blindness. The ocular findings including visual field, fundus, OCT and electroretinogram were compatible with the ocular findings in four patients with one or two deleterious mutations. Audiological examination, including pure-tone audiometry, was not performed, because the patients did not consent to the study.
Discussion
This study is the first to analyze mutations in the USH2A gene among Japanese arRP patients with no systemic manifestations. In total, we detected 85 USH2A sequence alterations, of which 12 were novel. Among these 85 sequence alterations, 5 were classified as very likely pathogenic mutations (1 deletion, 2 splicing and 2 missense mutations), 2 were possibly pathogenic mutations (2 missense mutations) and 78 were possible non-pathogenic sequence alterations (Tables 1 and 2, and Supplementary Table S2). Among the 7 very likely and possible pathogenic mutations, a deletion and 4 missense mutations were novel, whereas the other 2 splicing mutations have been reported as disease causing in USH2 patients.13, 15, 32, 33 Similar to our previous study of Japanese USH2 patients, our current study did not detect the most prevalent mutations, p.E767fs and p.C759F, which account for approximately 23–39% and 1–14% of mutated alleles, respectively, in Caucasian individuals.7, 8, 9, 10, 11 These results indicate that the profile of USH2A gene mutations differs largely between Japanese patients and previously reported Caucasian populations.4, 5, 6, 7, 8, 9, 10, 11, 12, 23, 24, 26, 27, 28, 29
We previously screened all EYS gene exons in 100 unrelated Japanese arRP patients with no systemic manifestations, with the exclusion of families showing obvious autosomal dominant inheritance, and, as a result, detected EYS gene mutations in 18–26% of the patients.30 Excluding 18 RP patients with very likely pathogenic EYS gene mutations, 82 of these 100 patients were employed in this study. Among them, we found at least one very likely pathogenic or possible pathogenic USH2A gene mutation in six cases, of which three had two mutations and three had one mutation (Tables 1 and 2). Previous studies reported that 23 out of the 96 USH2 patients carried heterozygous USH2A gene mutations,5 implying that this finding could be due to relatively large heterozygous deletions or deep intronic mutations.34 In this study, because the direct sequences of PCR-amplified samples were used, we were not able to detect large deletions, insertions or rearrangements. In addition, because audiograms were not obtained from all patients with USH2A gene mutations, some of them may be USH2 patients without documented hearing loss. Therefore our results can only provide an estimate of the prevalence of USH2A mutations among Japanese arRP patients without documented systemic manifestations, including hearing loss. Considering only one or two deleterious mutations, the minimum observed prevalence of distinct USH2A gene mutations is 4% (4/100). If the patients with one heterogeneous possible pathogenic mutation are included in the estimation, the prevalence increases to 6% (6/100). A few previous studies on USH2A mutations employed large sets of non-syndromic RP patients, which accounted for 7–23% of arRP patients.23, 26, 27, 28, 29 A possible reason for why the estimated prevalence in our study was lower than that of previous reports may be the fact that the Japanese population does not carry the p.E767fs or p.C759F mutation.
A previous report employing Japanese USH2 patients detected the c.8559-2A>G mutation in 4 out of the 19 cases, suggesting a possible frequent USH2A gene mutation among the Japanese population.13, 15 Here we identified that RP15H was homozygous for the c.8559-2A>G mutation, supporting the possibility of a frequent USH2A gene mutation among the Japanese population. To the best of our knowledge, this study is the first to report a patient homozygous for the c.8559-2A>G mutation. Although RP15H did not have documented hearing loss or communication problems, the hearing test demonstrated that the patient had moderate sensorineural hearing loss. A detailed medical interview revealed that the patient, a 61-year-old male, noticed a slight difficulty in hearing but considered it as age-appropriate. Elderly subjects, especially those aged >60 years, are affected by age-related hearing deterioration that makes it difficult to distinguish hearing loss from age-appropriate hearing. Therefore, auditory examination, including pure-tone audiometry, may be recommended for accurate evaluation of auditory function in elderly subjects. However, in our opinion, we could determine the presence or absence of hearing loss and select RP patients without auditory examination, because most of the subjects included in this study were middle-aged or younger.
In RP85N, we also found another missense mutation, c.2802T>G (p.C934W), which was previously reported as disease causing in a Chinese RP patient without hearing loss, although it has also been identified in two Chinese individuals among 100 normal Chinese controls.25 p.C934W was also listed in the dbSNP database (rs201527662) and the 1000 Genomes database and was detected in 1 of the 400 control alleles in this study. Therefore we evaluated p.C934W as a possible non-pathogenic sequence alteration in this study (Supplementary Table S2).
In our previous report, we were unable to assign three sequence alterations (p.C691T, p.G2752R and p.T3747R) identified in patient C212 or determine which one of them was pathogenic.13 In this study, we found that RP7H was heterozygous for p.G2752R, which was absent from 400 control alleles. However, because p.G2752R was described in the public SNP database (rs201863550) and was found to be genetically linked to the 3-bp in-frame deletion mutation p.E1199del in the patient’s family (Figure 1a), it was assigned to the group of possible non-pathogenic sequence alterations. We speculate that patient C212 may be compound heterozygous for p.C691T and p.T3747R.
Studies have reported the phenotype of non-syndromic RP caused by USH2A gene mutations among the Caucasian.35 The patients in this present study shared a relatively uniform phenotype, characterized by a symptom-free interval in the first and second decades of life, followed by a rapid decline in visual functions due to concentric constriction. The four patients with one or two deleterious mutations did not have any documented hearing loss or pronunciation problems. Although the hearing test results for RP7H and RP10H were normal (Figures 1g and h), the results for RP15H showed moderate hearing loss, indicating USH2 (Figure 1i). These findings suggest that RP without documented hearing loss occasionally includes moderate type of USH2.
In conclusion, the profile of USH2A gene mutations in arRP patients with no systemic manifestations differs largely between Japanese and Caucasian. Considering only one or two deleterious mutations, the observed prevalence of distinct USH2A gene mutations among Japanese arRP patients with no systemic manifestations was 4% (4/100). Based on these data, if both EYS and USH2A genes are analyzed among Japanese arRP patients with no systemic manifestations, gene defects could be detected in 22–32% of the patients in total (18–26% and 4–6%, respectively). We believe that screening for these two genes is effective for genetic testing and counseling of RP patients in Japan.
References
Yan, D. & Liu, X. Z. Genetics and pathological mechanisms of Usher syndrome. J. Hum. Genet. 55, 327–335 (2010).
Rosenberg, T., Haim, M., Hauch, A. M. & Parving, A. The prevalence of Usher syndrome and other retinal dystrophy-hearing impairment associations. Clin. Genet. 51, 314–321 (1997).
Eudy, J. D., Weston, M. D., Yao, S., Hoover, D. M., Rehm, H. L., Ma-Edmonds, M. et al. Mutation of a gene encoding a protein with extracellular matrix motifs in Usher syndrome type IIa. Science 280, 1753–1757 (1998).
Weston, M. D., Eudy, J. D., Fujita, S., Yao, S., Usami, S., Cremers, C. et al. Genomic structure and identification of novel mutations in usherin, the gene responsible for Usher syndrome type IIa. Am. J. Hum. Genet. 66, 1199–1210 (2000).
Le Quesne Stabej, P., Saihan, Z., Rangesh, N., Steele-Stallard, H. B., Ambrose, J., Coffey, A. et al. Comprehensive sequence analysis of nine Usher syndrome genes in the UK National Collaborative Usher Study. J. Med. Genet. 49, 27–36 (2012).
Dreyer, B., Tranebjaerg, L., Brox, V., Rosenberg, T., Möller, C., Beneyto, M. et al. A common ancestral origin of the frequent and widespread 2299delG USH2A mutation. Am. J. Hum. Genet. 69, 228–234 (2001).
Bernal, S., Medà, C., Solans, T., Ayuso, C., Garcia-Sandoval, B., Valverde, D. et al. Clinical and genetic studies in Spanish patients with Usher syndrome type II: description of new mutations and evidence for a lack of genotype–phenotype correlation. Clin. Genet. 68, 204–214 (2005).
Aller, E., Jaijo, T., Beneyto, M., Nájera, C., Oltra, S., Ayuso, C. et al. Identification of 14 novel mutations in the long isoform of USH2A in Spanish patients with Usher syndrome type II. J. Med. Genet. 43, e55 (2006).
Baux, D., Larrieu, L., Blanchet, C., Hamel, C., Ben Salah, S., Vielle, A. et al. Molecular and in silico analyses of the full-length isoform of usherin identify new pathogenic alleles in Usher type II patients. Hum. Mutat. 28, 781–789 (2007).
Dreyer, B., Brox, V., Tranebjaerg, L., Rosenberg, T., Sadeghi, A. M., Möller, C. et al. Spectrum of USH2A mutations in Scandinavian patients with Usher syndrome type II. Hum. Mutat. 29, 451 (2008).
Yan, D., Ouyang, X., Patterson, D. M., Du, L. L., Jacobson, S. G. & Liu, X. Z. Mutation analysis in the long isoform of USH2A in American patients with Usher syndrome type II. J. Hum. Genet. 54, 732–738 (2009).
Aller, E., Larrieu, L., Jaijo, T., Baux, D., Espinós, C., González-Candelas, F. et al. The USH2A c.2299delG mutation: dating its common origin in a Southern European population. Eur. J. Hum. Genet. 18, 788–793 (2010).
Nakanishi, H., Ohtsubo, M., Iwasaki, S., Hotta, Y., Mizuta, K., Mineta, H. et al. Identification of 11 novel mutations in USH2A among Japanese patients with Usher syndrome type 2. Clin. Genet. 76, 383–391 (2009).
Nakanishi, H., Ohtsubo, M., Iwasaki, S., Hotta, Y., Mizuta, K., Mineta, H. et al. Hair roots as an mRNA source for mutation analysis of Usher syndrome-causing genes. J. Hum. Genet. 55, 701–703 (2010).
Nakanishi, H., Ohtsubo, M., Iwasaki, S., Hotta, Y., Usami, S., Mizuta, K. et al. Novel USH2A mutations in Japanese Usher syndrome type 2 patients: marked differences in the mutation spectrum between the Japanese and other populations. J. Hum. Genet. 56, 484–490 (2011).
Hayakawa, M., Fujiki, K., Kanai, A., Matsumura, M., Honda, Y., Sakaue, H. et al. Multicenter genetic study of retinitis pigmentosa in Japan: I. Genetic heterogeneity in typical retinitis pigmentosa. Jpn J. Ophthalmol. 41, 1–6 (1997).
Abd El-Aziz, M. M., Barragán, I., O'Driscoll, C. A., Goodstadt, L., Prigmore, E., Borrego, S. et al. EYS, encoding an ortholog of Drosophila spacemaker, is mutated in autosomal recessive retinitis pigmentosa. Nat. Genet. 40, 1285–1287 (2008).
Collin, R. W., Littink, K. W., Klevering, B. J., van den Born, L. I., Koenekoop, R. K., Zonneveld, M. N. et al. Identification of a 2 Mb human ortholog of Drosophila eyes shut/spacemaker that is mutated in patients with retinitis pigmentosa. Am. J. Hum. Genet. 83, 594–603 (2008).
Abd El-Aziz, M. M., O'Driscoll, C. A., Kaye, R. S., Barragán, I., El-Ashry, M. F., Borrego, S. et al. Identification of novel mutations in the ortholog of Drosophila eyes shut gene (EYS) causing autosomal recessive retinitis pigmentosa. Invest. Ophthalmol. Vis. Sci. 51, 4266–4272 (2010).
Audo, I., Sahel, J. A., Mohand-Saïd, S., Lancelot, M. E., Antonio, A., Moskova-Doumanova, V. et al. EYS is a major gene for rod-cone dystrophies in France. Hum. Mutat. 31, E1406–E1435 (2010).
Barragán, I., Borrego, S., Pieras, J. I., González-del Pozo, M., Santoyo, J., Ayuso, C. et al. Mutation spectrum of EYS in Spanish patients with autosomal recessive retinitis pigmentosa. Hum. Mutat. 31, E1772–E1800 (2010).
Littink, K. W., van den Born, L. I., Koenekoop, R. K., Collin, R. W., Zonneveld, M. N., Blokland, E. A. et al. Mutations in the EYS gene account for approximately 5% of autosomal recessive retinitis pigmentosa and cause a fairly homogeneous phenotype. Ophthalmology 117, 2026–2033 (2010).
Rivolta, C., Sweklo, E. A., Berson, E. L. & Dryja, T. P. Missense mutation in the USH2A gene: association with recessive retinitis pigmentosa without hearing loss. Am. J. Hum. Genet. 66, 1975–1978 (2000).
Aller, E., Nájera, C., Millán, J. M., Oltra, J. S., Pérez-Garrigues, H., Vilela, C. et al. Genetic analysis of 2299delG and C759F mutations (USH2A) in patients with visual and/or auditory impairments. Eur. J. Hum. Genet. 12, 407–410 (2004).
Xu, W., Dai, H., Lu, T., Zhang, X., Dong, B. & Li, Y. Seven novel mutations in the long isoform of the USH2A gene in Chinese families with non-syndromic retinitis pigmentosa and Usher syndrome Type II. Mol. Vis. 17, 1537–1552 (2011).
Bernal, S., Ayuso, C., Antiñolo, G., Gimenez, A., Borrego, S., Trujillo, M. J. et al. Mutations in USH2A in Spanish patients with autosomal recessive retinitis pigmentosa: high prevalence and phenotypic variation. J. Med. Genet. 40, e8 (2003).
Seyedahmadi, B. J., Rivolta, C., Keene, J. A., Berson, E. L. & Dryja, T. P. Comprehensive screening of the USH2A gene in Usher syndrome type II and non-syndromic recessive retinitis pigmentosa. Exp. Eye Res. 79, 167–173 (2004).
McGee, T. L., Seyedahmadi, B. J., Sweeney, M. O., Dryja, T. P. & Berson, E. L. Novel mutations in the long isoform of the USH2A gene in patients with Usher syndrome type II or non-syndromic retinitis pigmentosa. J. Med. Genet. 47, 499–506 (2010).
Ávila-Fernández, A., Cantalapiedra, D., Aller, E., Vallespín, E., Aguirre-Lambán, J., Blanco-Kelly, F. et al. Mutation analysis of 272 Spanish families affected by autosomal recessive retinitis pigmentosa using a genotyping microarray. Mol. Vis. 16, 2550–2558 (2010).
Hosono, K., Ishigami, C., Takahashi, M., Park, D. H., Hirami, Y., Nakanishi, H. et al. Two novel mutations in the EYS gene are possible major causes of autosomal recessive retinitis pigmentosa in the Japanese population. PLoS ONE 7, e31036 (2012).
Adato, A., Lefèvre, G., Delprat, B., Michel, V., Michalski, N., Chardenoux, S. et al. Usherin, the defective protein in Usher syndrome type IIA, is likely to be a component of interstereocilia ankle links in the inner ear sensory cells. Hum. Mol. Genet. 14, 3921–3932 (2005).
Dai, H., Zhang, X., Zhao, X., Deng, T., Dong, B., Wang, J. et al. Identification of five novel mutations in the long isoform of the USH2A gene in Chinese families with Usher syndrome type II. Mol. Vis. 14, 2067–2075 (2008).
Le Guédard-Méreuze, S., Vaché, C., Baux, D., Faugère, V., Larrieu, L., Abadie, C. et al. Ex vivo splicing assays of mutations at noncanonical positions of splice sites in USHER genes. Hum. Mutat. 31, 347–355 (2010).
Steele-Stallard, H. B., Le Quesne Stabej, P., Lenassi, E., Luxon, L. M., Claustres, M., Roux, A. F. et al. Screening for duplications, deletions and a common intronic mutation detects 35% of second mutations in patients with USH2A monoallelic mutations on Sanger sequencing. Orphanet. J. Rare Dis. 8, 122 (2013).
Sandberg, M. A., Rosner, B., Weigel-DiFranco, C., McGee, T. L., Dryja, T. P. & Berson, E. L. Disease course in patients with autosomal recessive retinitis pigmentosa due to the USH2A gene. Invest. Ophthalmol. Vis. Sci. 49, 5532–5539 (2008).
Acknowledgements
We thank the patients who participated in the study. This study was supported by research grants from the Ministry of Health, Labour and Welfare (Research on Measures for Intractable Diseases) and from Japan Society for the Promotion of Science (Grant-in-Aid for Scientific Research (C) 23592561 and Grant-in Aid for Young Scientists (B) 23791975).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Zhao, Y., Hosono, K., Suto, K. et al. The first USH2A mutation analysis of Japanese autosomal recessive retinitis pigmentosa patients: a totally different mutation profile with the lack of frequent mutations found in Caucasian patients. J Hum Genet 59, 521–528 (2014). https://doi.org/10.1038/jhg.2014.65
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.65
This article is cited by
-
USH2A gene variants cause Keratoconus and Usher syndrome phenotypes in Pakistani families
BMC Ophthalmology (2021)
-
Development of a molecular diagnostic test for Retinitis Pigmentosa in the Japanese population
Japanese Journal of Ophthalmology (2018)