Abstract
To investigate the frequency and type of abnormal karyotype in Japan by amniocentesis before 22 weeks of gestation. We performed a retrospective analysis of 28 983 amniotic fluid specimens in a local population collected before 22 weeks gestations for fetal karyotyping. The incidence of abnormal karyotype was 6.0%. The main indication was advanced maternal age (AMA) of 35 years and older, which represented over half of the clinical indications. Abnormal karyotype was most frequently reported among the referrals for abnormal ultrasound findings (21.8%), followed by positive maternal serum screen results (5.3%). Three-fourths of abnormal karyotype was either autosomal aneuploidy (64.0%) or sex chromosome aneuploidy (11.6%). Abnormal karyotype was detected in 2.8% of pregnant women referred for AMA. Clinically significant abnormal karyotype increased with advancing maternal age. The frequency and type of abnormal karyotype detected by amniocentesis for various indications were determined. Amniocentesis was mainly performed among the referrals for AMA, which is a characteristic distribution of indications of Japan.
Similar content being viewed by others
Introduction
In recent years the proportion of mothers ⩾35 in Japan has been increasing against a background of decreasing birth rates, according to the Ministry of Health Labor and Welfare of Japan. Based on such demographic changes, Kajii1 projected an increasing frequency of Down syndrome live births. Accordingly, the number of amniocentesis being performed in Japan has risen.2 Amniocentesis is the gold standard for prenatal diagnosis of fetal chromosome abnormalities,3 accounting for over 99% of invasive diagnostic testing in the country.2 Although first-trimester aneuploidy screening program combined with nuchal translucency measurement is not yet widely available, non-invasive prenatal testing has been introduced in Japan since April 2013.
The frequency of fetal chromosome abnormality detection depends on clinical indications.4 Prenatal testing information is essential for genetic counseling and in the decision for appropriate tests. Wellesley et al.5 reported the prevalence of chromosome abnormalities at live birth, fetal death from 20 weeks of gestation and termination of pregnancy for fetal anomaly in Europe. In Japan, however, there is no substantial data on the frequency and type of abnormal karyotype in the local population detected by amniocentesis. The frequency and distributions of chromosome abnormalities identified by amniocentesis are expected to have changed with the introduction of non-invasive prenatal testing.6 In this study, we analyzed the incidence and the type of chromosome abnormalities using amniotic fluid specimens received at a prenatal testing laboratory before the introduction of non-invasive prenatal testing in Japan.
Materials and methods
Subjects
We conducted a retrospective study of pregnant women who underwent amniocentesis for chromosome analysis. Information was derived from the results of chromosome analyses and laboratory requisition forms. In total, 30 641 amniotic fluid specimens for fetal karyotyping were received at LabCorp Japan from January 2007 to December 2012.
Subsequently, 1594 specimens were further excluded for this study; 182 had no information of gestational age while 1412 were collected after 22 weeks of gestation. According to a 1990 statement by the Ministry of Health, Labor and Welfare, artificial abortions after 22 weeks of gestation are not permitted in Japan. Therefore, pregnant women who consider the option of pregnancy termination due to fetal chromosome abnormalities usually undergo amniocentesis before 22 weeks of gestations. Of the 29 047 specimens collected before 22 weeks of gestation, 64 failed in amniotic fluid culture. Results of fetal karyotyping were obtained in 28 983 specimens (99.8%). Eventually, these 28 983 specimens were eligible for the study.
Experimental design
Referral indications and chromosome abnormalities were stratified for the 28 983 specimens. Clinical indications were classified into six groups: advanced maternal age (AMA), abnormal ultrasound findings, family history of chromosome abnormality, positive result of maternal serum screening (MSS) test, parental anxiety and others. Clinical information provided in the test requisition forms was used in classifying the specimens into these six groups. AMA was defined as ⩾35 years of age at the expected date of delivery. The age of the women at the expected date of delivery and cytogenetic results were analyzed based on the date of birth provided in the test requisition form. Abnormal karyotype was classified into the following groups: autosomal aneuploidy, sex chromosome aneuploidy, balanced structural rearrangement, unbalanced structural rearrangement, mosaicism and others. Frequently reported chromosome abnormalities were classified as a subgroup.
Data analysis
Data used for analysis contained no identifiable personal information so as to protect individuals’ privacy. The data were analyzed using SAS version 9.3 and SAS JMP 10 (SAS Institute Inc., Cary, NC, USA). χ2-tests were used to test differences and association between the groups. Fisher’s exact test was used to test the significance for unbalanced structure rearrangements that have frequency counts <5.
Results
Distribution of clinical indications and frequency of abnormal karyotype
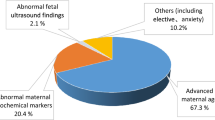
The most frequent referral (Table 1) indication was AMA, accounting for over half of the referral indications (54.7%). This was followed by positive result of MSS and abnormal ultrasound findings. The incidence of abnormal karyotype was 6.0% for all specimens. However, it varied by indications; 21.8% for abnormal ultrasound findings, 5.3% for positive result for MSS and 2.8% for AMA.
Proportion of abnormal karyotype
The indication of AMA accounted (Table 2) for over half of the indications. Of the detected abnormal karyotypes in all specimens, two-thirds of abnormal karyotype was autosomal aneuploidy including trisomy 21, trisomy 18 and trisomy 13 in order of descending frequency. Approximately 10% of abnormal karyotype was sex chromosome aneuploidy with 45,X accounting for over half of this group. The five categories of abnormal karyotype have different proportion of AMA and non-AMA indications and are independent of each other (P<0.0001). Three of the five categories, autosomal aneuploidy (P=0.0464), sex chromosome aneuploidy (P<0.001) and unbalanced structural rearrangement (P=0.0054), have significant association between AMA proportion and different incidence rates of specific karyotype within their categories. Specifically, AMA has lower proportion of trisomy 21, 18, 13 and other trisomies, higher proportion of 47,XXY, 47,XXX, 47,XYY and marker chromosome and lower proportion of additional material on the chromosome, unbalanced translocation and deletion.
Frequency of abnormal karyotype based on clinical indications
Autosomal aneuploidy was most (Table 3) frequently identified when the indication was abnormal ultrasound findings, followed by positive result of MSS and AMA. For these indications, the incidence of trisomy 21 was 10.1%, 3.0% and 1.1%, respectively, while the incidence of sex chromosome aneuploidy was 2.8%, 0.4% and 0.4%, respectively. Among the specimens with indication of abnormal ultrasound findings, 45,X was the most frequent sex chromosome aneuploidy.
Maternal age-specific rates for abnormal karyotype among referrals for AMA
Maternal age-specific rates for (Table 4) abnormal karyotype excluding balanced structural rearrangements were increased from 1.1% at 35 years to 8.0% at ⩾47 years. However, there was a variation in this trend with each additional year of age. Advancing maternal age was correlated with the frequency of clinically significant abnormal karyotype every 3 years, increasing from 1.3% (35–37 years) to 4.7% (⩾44 years). For sex chromosome aneuploidy, the frequency was increased from 0.3% (35–37 years) to 0.9% (⩾44 years), while the frequency of autosomal aneuploidy was more significantly increased from 0.7% (35–37 years) and 3.5% (⩾44 years).
Discussion
We presented an analysis of chromosome abnormalities identified by amniocentesis before 22 weeks of gestation. Our study represents the largest series of fetal karyotyping of amniotic fluid specimens in Japan.
AMA as a main clinical indication
In terms of clinical indications of amniocentesis for fetal karyotyping, the main indication was AMA. In contrast, in countries whereby prenatal screening policy is adopted, the proportion of AMA indication was smaller.7, 8, 9, 10 This is due to most developed countries having national guidelines that recommend fetal aneuploidy screening prior to invasive testing.11 In Japan, however, fetal aneuploidy screening such as MSS and first-trimester screening are not routinely offered to pregnant women.
Higher incidence of abnormal karyotype detected by amniocentesis
We detected chromosome abnormalities in 6.0% of the specimens, which was higher than reported in previous studies in other countries (between 2.7–3.1%),8, 12, 13, 14 although the frequency of abnormal karyotype in the specimens with indication of AMA was 2.8%, which was similar to that in other studies (between 2.1–3.4%).8, 12, 13, 15 The contributing factor of high frequency of chromosome abnormality is likely to be the larger proportion of referrals for abnormal ultrasound findings (14.1%) compared with previous studies.8, 12, 13 These findings suggest that amniocentesis for fetal karyotyping in our study population was performed for pregnant women with more significant abnormal ultrasound findings.
Frequency and types of chromosome abnormalities detected by amniocentesis
We found that 75.6% of abnormal karyotype detected by amniocentesis before 22 weeks of gestation was composed of either autosomal aneuploidy (64.0%) or sex chromosomal aneuploidy (11.6%). When we excluded balanced structural rearrangement (12.9% of all abnormal karyotype), the proportion of autosomal aneuploidy and sex chromosome aneuploidy was 73.5% and 13.3%, respectively. These findings were similar to the report by Wellesley et al.5 on the results of population-based congenital anomaly registers in Europe, which showed the frequency of autosomal and sex chromosome aneuploidy to be 71.1% and 12.1%, respectively. In our study, the frequency of trisomy 18 and sex chromosome trisomies was 19.9%(=303/1524) and 6.6%(=100/1524), respectively, both higher than those reported by Wellesley et al.5 These findings were most likely attributed that our study assessed fetal abnormal karyotype before 22 gestational weeks which included unborn cases.
Frequency and types of chromosome abnormalities in AMA by maternal age
In this study, maternal age-specific rates for abnormal karyotype ascertained in the Japanese population receiving amniocentesis because of AMA were documented. We confirmed the age dependency of abnormal karyotype including clinically significant abnormal karyotype such as autosomal and sex chromosomal aneuploidies. The frequency of these abnormal karyotypes was similar to the data of a European collaborative of 52 965 amniocenteses performed on women aged ⩾35 compiled prior to the routine use of fetal aneuploidy screening.16 Maternal age-specific rates for abnormal karyotype revealed in this study could assist Japanese pregnant women in understanding the risk of fetal chromosome abnormalities and their decision for prenatal testing.
Limitations of the study
The information available was dependent on what was revealed in the laboratory requisition forms at the time of testing. Nonetheless, our study presented the largest series of amniocentesis cases in Japan, accounting for about a third of all specimens in the country.17
Conclusion
We reported on the frequency and the type of chromosome abnormalities diagnosed in utero before 22 weeks of gestation among the local population. The findings may provide valuable information for prenatal genetic counseling followed the decision in electing appropriate testing options.
References
Kajii, T. Predicted prevalence of Down syndrome live births in Japan, 1970–2006. Am. J. Med. Genet. A 146A, 1387–1388 (2008).
Sasaki, A., Sawai, H., Masuzaki, H., Hirahara, F. & Sago, H. Low prevalence of genetic prenatal diagnosis in Japan. Prenat. Diagn. 31, 1007–1009 (2011).
Sago, H. Prenatal Diagnosis of Chromosome abnormalities through Amniocentesis. J. Mamm. Ova Res. 21, 18–21 (2004).
Shaffer, L. G., Rosenfeld, J. A., Dabell, M. P., Coppinger, J., Bandholz, A. M., Ellison, J. W. et al. Detection rates of clinically significant genomic alterations by microarray analysis for specific anomalies detected by ultrasound. Prenat. Diagn. 32, 986–995 (2012).
Wellesley, D., Dolk, H., Boyd, P. A., Greenlees, R., Haeusler, M., Nelen, V. et al. Rare chromosome abnormalities, prevalence and prenatal diagnosis rates from population-based congenital anomaly registers in Europe. Eur. J. Hum. Genet. 6, 521–526 (2012).
Chetty, S., Garabedian, M. J. & Norton, M. E. Uptake of noninvasive prenatal testing (NIPT) in women following positive aneuploidy screening. Prenat. Diagn. 33, 542–546 (2013).
Lichtenbelt, K. D., Alizadeh, B. Z., Scheffer, P. G., Stoutenbeek, P., Schielen, P. C., Page-Christiaens, L. C. et al. Trends in the utilization of invasive prenatal diagnosis in the Netherlands during 2000–2009. Prenat Diagn. 31, 765–772 (2011).
Mademont-Soler, I., Morales, C., Clusellas, N., Soler, A. & Sánchez, A. Group of Cytogenetics from Hospital Clínic de Barcelona. Prenatal cytogenetic diagnosis in Spain: analysis and evaluation of the results obtained from amniotic fluid samples during the last decade. Eur. J. Obstet. Gynecol. Reprod. Biol. 157, 156–160 (2011).
Nakata, N., Wang, Y. & Bhatt, S. Trends in prenatal screening and diagnostic testing among women referred for advanced maternal age. Prenat. Diagn. 30, 198–206 (2010).
Wray, A. M., Ghidini, A., Alvis, C., Hodor, J., Landy, H. J. & Poggi, S. H. The impact of first-trimester screening on AMA patients' uptake of invasive testing. Prenat. Diagn. 25, 350–353 (2005).
Benn, P., Borell, A., Chiu, R., Cuckle, H., Dugoff, L., Faas, B. et al. Position statement from the Aneuploidy Screening Committee on behalf of the Board of the International Society for Prenatal Diagnosis. Prenat. Diagn. 33, 622–629 (2013).
Chang, Y. W., Chang, C. M., Sung, P. L., Yang, M. J., Li, W. H., Li, H. Y. et al. An overview of a 30-year experience with amniocentesis in a single tertiary medical center in Taiwan. Taiwan J. Obstet. Gynecol. 51, 206–211 (2012).
Han, S. H., An, J. W., Jeong, G. Y., Yoon, H. R., Lee, A., Yang, Y. H. et al. Clinical and cytogenetic findings on 31,615 mid-trimester amniocenteses. Korean J. Lab. Med. 28, 378–385 (2008).
Karaoguz, M. Y., Bal, F., Yakut, T., Ercelen, N. O., Ergun, M. A., Gokcen, A. B. et al. Cytogenetic results of amniocentesis materials: incidence of abnormal karyotypes in the Turkish collaborative study. J. Genet. Couns. 17, 219–230 (2006).
Forabosco, A., Percesepe, A. & Santucci, S. Incidence of non-age-dependent chromosome abnormalities: a population-based study on 88965 amniocenteses. Eur. J. Hum. Genet. 17, 897–903 (2009).
Ferguson-Smith, M. A. & Yates, J. R. Maternal age specific rates for chromosome aberrations and factors influencing them: report of a collaborative european study on 52965 amniocenteses. Prenat. Diagn. 4, 5–44 (1984).
Nishiyama, M., Sawai, H. & Kosugi, S. The current state of genetic counseling before and after amniocentesis for fetal karyotyping in Japan: a survey of obstetric hospital clients of a prenatal testing laboratory. J. Genet. Couns. 22, 795–804 (2013).
Acknowledgements
We would like to thank Dr Julian Tang of the Department of Education for Clinical Research, the National Center for Child Health and Development for proofreading, editing and writing a part of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
M Nishiyama is a former employee of LabCorp Japan. J Yan is a current employee of Laboratory Corporation of America Holdings. The remaining authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Nishiyama, M., Yan, J., Yotsumoto, J. et al. Chromosome abnormalities diagnosed in utero: a Japanese study of 28 983 amniotic fluid specimens collected before 22 weeks gestations. J Hum Genet 60, 133–137 (2015). https://doi.org/10.1038/jhg.2014.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.116
This article is cited by
-
Prevalence of common aneuploidy in twin pregnancies
Journal of Human Genetics (2022)
-
The correlation between maternal age and fetal sex chromosome aneuploidies: a 8-year single institution experience in China
Molecular Cytogenetics (2021)
-
Pregnant women’s opinions toward prenatal pretest genetic counseling in Japan
Journal of Human Genetics (2021)
-
Nationwide survey for current clinical status of amniocentesis and maternal serum marker test in Japan
Journal of Human Genetics (2016)