Abstract
Gaucher disease (GD) is an autosomal recessive disorder caused by mutations in the glucocerebrosidase (GBA) gene, leading to a deficiency of lysosomal β-glucosidase and accumulation of glycosphingolipids in macrophages. We studied five Thai families with GD (four with GD type 1 and one with GD type 2). Using long-template PCR, PCR using specific primers for the functional gene, direct sequencing of all coding regions of GBA and restriction enzyme digestions, all 10 mutant alleles were successfully identified. The common c.1448T>C (p.L483P or L444P) mutation was identified in 60% of mutant alleles. Of the two patients homozygous for the p.L483P (L444P) mutation, one died from hepatic failure at age 16 years and the other died from sepsis at age 12 years. This p.L483P (L444P) mutation was found in four different haplotypes, suggesting that it was a recurrent mutation, not caused by a founder effect. Two novel mutations, a missense (c.1204T>C, p.Y402H), and a termination codon mutation (c.1609T>C, p.X537A) were found. Studies to determine the molecular pathomechanism of the p.X537A mutation, the first of its kind in this gene, showed that it decreased the amount of protein being expressed and the enzymatic activity, while it was still correctly localized.
Similar content being viewed by others
Introduction
Gaucher disease (GD; MIM 230800), the most prevalent lysosomal storage disorder, is caused by a deficiency of lysosomal enzyme glucocerebrosidase, or acid β-glucosidase, which normally hydrolyzes glucocerebroside to glucose and ceramide, leading to accumulation of glucocerebroside in macrophages. There are three clinical subtypes of GD, distinguished by the absence or presence and severity of neurologic complications. Type 1 (MIM 230800), or non-neuronopathic disease, does not involve the nervous system. Type 2 (MIM 230900), or acute-neuronopathic disease, is a fatal neurodegenerative disorder of infancy. Type 3 (MIM 231000), or chronic-neuronopathic disease, is a slowly progressive neurologic disease with survival into adulthood. Hepatosplenomegaly and bone lesions occur in all forms.1
The disease is an autosomal recessive disorder resulting from mutations in the glucocerebrosidase gene (GBA, MIM 606463) of ∼7.5 kb, located on chromosome 1q21 and composed of 11 exons. A highly homologous ∼5.5 kb pseudogene (GBAP, MIM 606463) that shares 96% exonic sequence homology is located 16 kb downstream from the functional gene.2
At least 291 different mutations have been identified in the GBA gene (the Human Genome Mutation Database, http://www.hgmd.cf.ac.uk/ac/index.php, February, 2013). The frequencies of specific mutated alleles vary in different populations. The most common mutation in the Ashkenazi Jewish, accounting for ∼70% of mutations is p.N409S (N370S).3 In this report, we studied the clinical, biochemical and molecular characteristics of five Thai families with GD.
Materials and methods
Subjects
Five unrelated Thai patients were diagnosed as having GD through clinical findings including hepatosplenomegaly and the presence of Gaucher cells in bone marrow aspiration. Based on the clinical findings, four unrelated patients were classified as type 1 and one as type 2. Consanguinity was denied in all families. With the exception of patient 1, who had an elder brother with similar clinical features and died at the age 18 months, others were sporadic cases. Glucocerebrosidase activity in leukocytes was determined by using a mixture of 4-methyl-umbelliferone-β-D-glucopyranoside as a substrate and fluorescence was measured with a Cecil spectrofluorometer using 450-nm emission and 365-nm excitation filters. The normal range of enzyme activity was determined in leukocytes of six normal Thais. Each patient’s major clinical features and enzymatic activity are shown in Table 1.
Genotyping
After informed consent was obtained, high-molecular weight genomic DNA of all patients except patient 1 was extracted from peripheral blood leukocytes. Long-template PCR amplifying the entire GBA gene was performed using the Elongase Enzyme Mix (Invitrogen, Carlsbad, CA, USA) with primers GBA-F1 and GBA-R11 (Table 2). DNA was denatured for 30 s at 94 °C, followed by 35 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s and elongation at 68 °C for 7 min. The 6.6-kb product amplified by long-template PCR was gel purified using the QIAquick gel extraction kit (Qiagen, Valencia, CA, USA), then treated with ExoSAP-IT (USB Corporation, Cleveland, OH, USA), and sent for direct sequencing at Macrogen Inc., Seoul, Korea. In addition, the genomic DNA of all patients including patient 1, whose high-molecular weight DNA was not available, was subjected to PCR amplification using primers designed to amplify each exon of the functional GBA gene but not the pseudogene (Table 2). PCR products were treated with ExoSAP-IT and sent for direct sequencing. Sequence analyses were performed by Sequencher 4.2. Samples with possible new variants were resequenced. The positions of mutations were compared with the GBA coding sequence (GenBank accession no. J03059.1).
The p.L483P (L444P), p.Y402H and p.X537A mutations were verified by restriction enzyme digestions of the patients’ PCR products, using NciI, RsaI and Cac8I, respectively. Parents of patients with probable homozygous mutations for the p.L483P (L444P) mutation were also examined for the variants by restriction enzyme analysis. RNA from patient 5 who had the IVS6 mutation was extracted from peripheral blood leukocytes using QIAamp RNA blood mini kit (Qiagen). Reverse transcription was performed using ImProm-II reverse transcriptase (Promega, Madison, WI, USA) according to company recommendations. PCR amplification of the GBA cDNA covering the 3′-end of exon 4 through the termination codon to the 5′- end of exon 11 was performed using primers cGBA4 and cGBA-R11 designed to amplify only the functional GBA cDNA, but not the cDNA of the pseudogene (Table 2).
Haplotype analysis of the p.L483P (L444P) allele
We used PCR-RFLP to detect the p.L483P (L444P) mutation in four additional patients with GD. Three were homozygous and one heterozygous for the mutation. DNA of these four cases, patients 1, 2 and 3, and available parents were PCR-amplified with primers as shown in Table 3 for previously described microsatellites (5GC3.2, ITG6.2, D1S2777, D1S1595 D1S2721). DNA of patient 4 was not available for this haplotype analysis. Genotyping was performed by Macrogen. Data were analyzed by GeneScan software (Applied Biosystem, Carlsbad, CA, USA).
Functional analysis of the p.X537A mutation
For glucocerebrosidase activity analysis, RNA of normal controls and patient 5 was extracted from peripheral blood leukocytes with QIAamp RNA blood mini kit (Qiagen), then reverse-transcribed and amplified by PCR using primers GBA-XhoI-F and GBA-EcoRI-R (Table 2) to add the XhoI and EcoRI sites at the 5′ and 3′ ends, respectively. The amplified cDNA was cloned into the pGEM-T Easy Vector System (Promega) and subsequently into the pcDNA3.1 expression vector (Invitrogen), and sequenced. These constructs were transiently transfected into COS-7 (fibroblast) cells, using Lipofectamine 2000 (Invitrogen). After 24-hr transfection, cells were centrifuged and sonicated in dH2O. Protein concentration was determined by BCA protein assay (Micro BCA Protein Assay Kit, PIERCE, Rockford, IL, USA) and the glucocerebrosidase activity was measured by fluorimetric assay using 4-methyl-umbelliferone-β-D-glucopyranoside.
For protein expression analysis, the p.N409S (N370S) mutation, a positive control for the enzyme mislocalization to the endoplasmic reticulum (ER),4 was generated using QuikChange Site-Directed Mutagenesis Kit (Stratagene, La Jolla, CA, USA). The GBA clones were confirmed by direct sequencing. Cells transfected with the wild-type, p.X537A and p.N409S (N370S) GBA were immunoblotted to measure the level of glucocerebrosidase. Protein extracts were prepared from cell pellets harvested in lysis buffer with freshly added protease inhibitors, subjected to 10% polyacrylamide gel electrophoresis and transferred to PVDF membranes. The membranes were blotted with antibodies to glucocerebrosidase (Santa Cruz Biotechnology, Santa Cruz, CA, USA) and actin (Santa Cruz Biotechnology), a loading control.
For subcellular localization analysis, the COS-7 cells transfected with the wild-type and p.X537A GBA were analyzed by immunofluorescence staining. Cells were grown directly on Lab-Tek II chamber slides, and fixed 24–48 h after transfection with cold methanol. Cells were incubated with rabbit polyclonal immunoglobulin G antibodies to glucocerebrosidase (Santa Cruz Biotechnology), and mouse monoclonal immunoglobulin G1 antibodies to LAMP2 as a lysosomal marker (Abcam, Cambridge, UK). These cells were subsequently analyzed with Carl Zeiss LSM 700 confocal microscope (Jena, Germany).
Results
The clinical, biochemical and mutational profiles of patients are summarized in Table 1. Four patients were classified as GD type 1 and one as type 2. Among patients with type 1 GD, the onset of hepatosplenomegaly ranged from 7 months to 7 years old. All patients whose leukocytic glucocerebrosidase activities were determined had no or markedly low activities (<1.07 nmol mg−1 protein per hour) compared with 11.63±4.97 nmol mg−1 protein per hour in Thai controls.
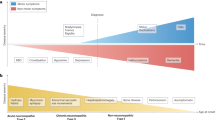
We successfully identified all 10 mutant alleles with either long-template PCR or PCR using specific primers for the functional GBA gene (Table 2). Both methods gave the same results. Four patients had the p.L483P (L444P) mutation. Patients 1 and 4 were compound heterozygotes (Figure 1a lower panel, lanes 5 and 6, respectively). Patients 2 and 3 were homozygotes (Figure 1a lower panel, lanes 4 and 3, respectively). The parents of patients 2 and 3 denied consanguinity, and were all heterozygous for the c.1448T>C (p.L483P) mutation. Patient 2 died from hepatic failure at age 16 years. Patient 3 had thrombocytopenia requiring splenectomy at age 4, fracture of her right femoral neck at age 9 and died from sepsis at age 12. This p.L483P (L444P) mutation was found in four different haplotypes (Table 4).
Mutation analysis of the common p.L483P (L444P) mutation (column a) and the novel mutations, p.Y402H (column b) and p.X537A (column c). Upper and middle panels, electropherograms of the wild-type and heterozygous mutant alleles, respectively. Lower panel, restriction enzyme digestion analysis. M is a 100-bp marker. The arrow heads indicate the 500-bp bands. In column a, the p.L483P (L444P) mutation creates an NciI restriction site. Therefore, the 638-bp PCR products of the mutant allele of individuals homozygous (lanes 3 and 4) and heterozygous (lanes 1, 2, 5, and 6) for the mutation were digested into 536-bp and 102-bp (not shown) products. In column b, the p.Y402H mutation in patient 4 (lane 2) eliminates the RsaI site, leaving the 580-bp product intact. The 580-bp product was digested into 430 and 150-bp (not shown) products of the other allele. In column c, the p.X537A mutation in patient 5 (lane 1) creates a Cac8I site. Therefore, the 840-bp product of the mutant allele was digested into 667 and 173-bp (not shown) products. A full color version of this figure is available at the Journal of Human Genetics journal online.
Two novel mutations were identified. A novel non-synonymous variant, c.1204T>C (p.Y402H), in exon 8 was found in patient 4 (Figure 1b middle panel and lower panel) and a novel termination codon mutation, c.1609T>C (p.X537A) (Figure 1c middle panel and lower panel), was found in patient 5. The boy was heterozygous for a splice site mutation, IVS6-1G>C. Sequencing of his cDNA revealed only the sequence of the p.X537A allele with no detectable level of the IVS6-1G>C transcript (Figure 1c lower panel). Expression of the p.X537A mutant and the wild-type clones in COS-7 cells demonstrated that the mutation reduced the residual glucocerebrosidase enzyme activity with respect to controls (Figure 2) and reduced the protein expression level (Figure 3), but did not significantly change the protein subcellular localization in mammalian cells (Figure 4).
Glucocerebrosidase (GBA) activity analysis of the p.X537A mutant. Enzyme activity was measured on extracts of cells transfected with the empty pcDNA3.1 vector (empty vector), wild-type GBA (wild-type), p.N409S mutant (p.N409S) and p.X537A mutant (p.X537A). Enzyme activity from cells transfected with the wild-type GBA was used as a baseline.
Glucocerebrosidase (GBA) expression analysis of p.X537A by western blotting. Top panel: Empty vector, wild-type (WT), p.N409S, p.X537A=cells transfected with the empty pcDNA3.1 vector, wild-type GBA, p.N409S mutant and p.X537A mutant, respectively. Arrow=a non-specific band. Lower panel: glyceraldehyde 3-phosphate dehydrogenase (GAPDH) loading control.
Subcellular localization analysis of p.X537A mutant by immunofluorescence confocal microscopy. (a, b)=wild-type glucocerebrosidase (GBA), (c, d)=p.X537A mutant, E=p.N409S. Green=GBA, red=LAMP2 (a lysosomal marker), blue=nuclei counterstained with 4′,6-diamidino-2-phenylindole. A full color version of this figure is available at the Journal of Human Genetics journal online.
Discussion
The presence of a highly homologous pseudogene sequence and several types of mutations including large recombinant alleles or deletions has made mutation analysis of GBA challenging.5 Using solely conventional PCR and single-strand conformation polymorphism (SSCP) or PCR-based mutation-detection techniques to screen for specific mutations might result in a significant number of unidentified mutant alleles.6 Therefore, in this study, direct mutation detection was performed by sequencing the entire coding region in all patients either by long-template PCR or PCR using specific primers for the functional gene. With these methods, all ten mutant alleles were identified in our five patients (see Table 1).
Patient 1 was compound heterozygous for p.L483P/p.N227K (L444P/N188K). The N188K mutation is a rare mutation previously found in patients with type 2 GD.7 Sequencing electropherogram of patients 2 and 3 showed only the c.1448T>C (p.L483P) mutation, which could be homozygous or hemizygous. Therefore, the genotypes of their parents were studied and revealed that all were heterozygous for the p.L483P (L444P) mutation, suggesting that patients 2 and 3 were homozygous for the mutation. p.L483P (L444P) is the most common mutant allele in the Thai patients with GD studied, accounting for 60% of mutant alleles. Notably, because conventional PCR method could not distinguish the isolate p.L483P (L444P) mutation and the p.L483P (L444P) as a part of a recombinant allele carrying additional pseudogene sequence alterations, further evaluation by other techniques such as direct sequencing to establish the presence or absence of a complex allele should be considered.8, 9 The p.L483P (L444P) mutation occurs with significant frequencies in various populations, including 41% of mutant alleles in the Japanese,6 and 2.84% in the Jewish.10 At the age of death at 16 years in patient 2 and 12 years in patient 3, both patients with homozygous p.L483P (L444P) did not show primary neurological manifestations, and, therefore, were categorized as type 1. A previously reported Thai patient with homozygous for the p.L483P (L444P) mutation was described to have a ‘Norbottnian-like’ phenotype, with mild neurological involvement.11 However, 15 of 19 Caucasian patients homozygous for the p.L483P (L444P) had neuronopathic GD.12 In addition, 9 of 12 Japanese patients with this genotype who were originally diagnosed with non-neuronopathic GD, developed neurological signs/symptoms during follow-up.13 Patient 2 died from cirrhosis and hepatic failure. Owing to no other identifiable causes of cirrhosis, this could be a complication of GD. There are several previous reports of GD patients dying from cirrhosis.14, 15 This p.L483P (L444P) mutation was found in four different haplotypes, suggesting that it was a recurrent mutation, not caused by a founder effect.
Two novel mutations including a missense (c.1204T>C, p.Y402H) and a mutation in the termination codon (c.1609T>C, p.X537A) were identified. A splice site mutation previously reported in a Thai patient with type 3 GD,11 the IVS6-1G>C change, was compound heterozygous with the c.1609T>C (p.X537A) in patient 5. Sequencing of his cDNA showed no skipping around IVS6 and only the C at position 1609 (Figure 1c lower panel), suggesting that it contained only the sequence of the p.X537A allele. It is probable that the IVS6-1G>C is pathogenic due to the absence of its mRNA, which is most likely from a splicing defect, leading to a premature stop codon and degradation of its mRNA via a nonsense mediated mRNA decay.16 The c.1609T>C (p.X537A) mutation is the first identified termination codon mutation in the GBA gene and expected to result in the addition of 15 more amino acids before coming to a new stop. Functional studies have suggested that the mutation decreases the amount of protein being expressed and the enzymatic activity, while it is still correctly localized. Termination codon mutations have been observed in many disorders, including Wiskott–Aldrich syndrome.17
In conclusion, we report five Thai patients with GD. A common mutation, p.L483P (L444P), accounting for 60% of mutant alleles, and two novel mutations, c.1204T>C (p.Y402H) and c.1609T>C (p.X537A), were identified. Phenotypes of the two patients homozygous for p.L483P (L444P) were severe; both died in their teens. Long-term follow-up is necessary in determining the disease severity associated with the novel mutations.
Accession codes
References
Grabowski, G. A. Recent clinical progress in Gaucher disease. Curr. Opin. Pediatr. 17, 519–524 (2005).
Horowitz, M., Wilder, S., Horowitz, Z., Reiner, O., Gelbart, T. & Beutler, E. The human glucocerebrosidase gene and pseudogene: structure and evolution. Genomics 4, 87–96 (1989).
Diaz, G. A., Gelb, B. D., Risch, N., Nygaard, T. G., Frisch, A., Cohen, I. J. et al. Gaucher disease: the origins of the Ashkenazi Jewish N370S and 84GG acid beta-glucosidase mutations. Am. J. Hum. Genet. 66, 1821–1832 (2000).
Schmitz, M., Alfalah, M., Aerts, J. M., Naim, H. Y. & Zimmer, K. P. Impaired trafficking of mutants of lysosomal glucocerebrosidase in Gaucher’s disease. Int. J. Biochem. Cell Biol. 37, 2310–2320 (2005).
Tayebi, N., Stubblefield, B. K., Park, J. K., Orvisky, E., Walker, J. M., LaMarca, M. E. et al. Reciprocal and nonreciprocal recombination at the glucocerebrosidase gene region: implications for complexity in Gaucher disease. Am. J. Hum. Genet. 72, 519–534 (2003).
Eto, Y. & Ida, H. Clinical and molecular characteristics of Japanese Gaucher disease. Neurochem. Res. 24, 207–211 (1999).
Stone, D. L., Tayebi, N., Orvisky, E., Stubblefield, B., Madike, V. & Sidransky, E. Glucocerebrosidase gene mutations in patients with type 2 Gaucher disease. Hum. Mutat. 15, 181–188 (2000).
Koprivica, V., Stone, D. L., Park, J. K., Callahan, M., Frisch, A., Cohen, I. J. et al. Analysis and classification of 304 mutant alleles in patients with type 1 and type 3 Gaucher disease. Am. J. Hum. Genet. 66, 1777–1786 (2000).
Tayebi, N., Stern, H., Dymarskaia, I., Herman, J. & Sidransky, E. 55-base pair deletion in certain patients with Gaucher disease complicates screening for common Gaucher alleles. Am. J. Med. Genet. 66, 316–319 (1996).
Grabowski, G. A. Gaucher disease: gene frequencies and genotype/phenotype correlations. Genet. Test. 1, 5–12 (1997).
Suwannarat, P., Keeratichamroen, S., Wattanasirichaigoon, D., Ngiwsara, L., Cairns, J. R., Svasti, J. et al. Molecular characterization of type 3 (neuronopathic) Gaucher disease in Thai patients. Blood Cells Mol. Dis. 39, 348–352 (2007).
Sidransky, E., Tsuji, S., Martin, B. M., Stubblefield, B. & Ginns, E. I. DNA mutation analysis of Gaucher patients. Am. J. Med. Genet. 42, 331–336 (1992).
Ida, H., Rennert, O. M., Iwasawa, K., Kobayashi, M. & Eto, Y. Clinical and genetic studies of Japanese homozygotes for the Gaucher disease L444P mutation. Hum. Genet. 105, 120–126 (1999).
Ida, H., Rennert, O. M., Ito, T., Maekawa, K. & Eto, Y. Clinical and genetic studies of five fatal cases of Japanese Gaucher disease type 1. Acta. Paediatr. Jpn. 38, 233–236 (1996).
Perel, Y., Bioulac-Sage, P., Chateil, J. F., Trillaud, H., Carles, J., Lamireau, T. et al. Gaucher’s disease and fatal hepatic fibrosis despite prolonged enzyme replacement therapy. Pediatrics 109, 1170–1173 (2002).
Conti, E. & Izaurralde, E. Nonsense-mediated mRNA decay: molecular insights and mechanistic variations across species. Curr. Opin. Cell. Biol. 17, 316–325 (2005).
Chatchatee, P., Srichomthong, C., Chewatavorn, A. & Shotelersuk, V. A novel termination codon mutation of the WAS gene in a Thai family with Wiskott-Aldrich syndrome. Int. J. Mol. Med. 12, 939–941 (2003).
Acknowledgements
We would like to thank Dr Darintr Sosothikul for referring patients to us and Dr Nipan Israsena for technical advices. This study was supported by Ratchadaphiseksomphot Endowment Fund, Faculty of Medicine, Chulalongkorn University, the Thailand Research Fund, and The Integrated Innovation Academic Center, Chulalongkorn University Centenary Academic Development Project (CU56-HR05), and the Higher Education Research Promotion and National Research University Project of Thailand, Office of the Higher Education Commission (HR1163A). Duangrurdee Wattanasirichaigoon is a recipient of Research Career Development Awards from the Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Tammachote, R., Tongkobpetch, S., Srichomthong, C. et al. A common and two novel GBA mutations in Thai patients with Gaucher disease. J Hum Genet 58, 594–599 (2013). https://doi.org/10.1038/jhg.2013.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2013.60
Keywords
This article is cited by
-
Gaucher disease: clinical phenotypes and refining GBA mutational spectrum in Thai patients
Orphanet Journal of Rare Diseases (2021)
-
Clinical phenotype features and genetic etiologies of 38 children with progressive myoclonic epilepsy
Acta Epileptologica (2020)
-
Gaucher disease: single gene molecular characterization of one-hundred Indian patients reveals novel variants and the most prevalent mutation
BMC Medical Genetics (2019)
-
Novel mutations in the glucocerebrosidase gene of Indian patients with Gaucher disease
Journal of Human Genetics (2014)