Abstract
Usher syndrome (USH) is an autosomal recessive disorder characterized by retinitis pigmentosa and hearing loss. USH type 1 (USH1), the second common type of USH, is frequently caused by MYO7A and CDH23 mutations, accounting for 70–80% of the cases among various ethnicities, including Caucasians, Africans and Asians. However, there have been no reports of mutation analysis for any responsible genes for USH1 in Japanese patients. This study describes the first mutation analysis of MYO7A and CDH23 in Japanese USH1 patients. Five mutations (three in MYO7A and two in CDH23) were identified in four of five unrelated patients. Of these mutations, two were novel. One of them, p.Tyr1942SerfsX23 in CDH23, was a large deletion causing the loss of 3 exons. This is the first large deletion to be found in CDH23. The incidence of the MYO7A and CDH23 mutations in the study population was 80%, which is consistent with previous findings. Therefore, mutation screening for these genes is expected to be a highly sensitive method for diagnosing USH1 among the Japanese.
Similar content being viewed by others
Introduction
Usher syndrome (USH) is an autosomal recessive disorder characterized by retinitis pigmentosa (RP) and hearing loss (HL), with or without vestibular dysfunction.1 It is the most common cause of combined deafness and blindness in industrialized countries, with a general prevalence of 3.5–6.2 per 100 000 live births.2, 3, 4, 5, 6, 7 The syndrome is clinically and genetically heterogeneous and can be classified into three clinical subtypes on the basis of the severity and progression of HL and the presence or absence of vestibular dysfunction.8, 9, 10
USH type 1 (USH1) is characterized by congenital severe-to-profound HL and vestibular dysfunction; it is the second common type after USH type 2 and accounts for 25–44% of the USH cases.7, 11 Five causative genes have been identified: myosin VIIA (HUGO gene symbol MYO7A); Usher syndrome 1C, harmonin (USH1C); cadherin-related 23 (CDH23); protocadherin-related 15 (PCDH15); and Usher syndrome 1G, Sans (USH1G).12, 13, 14, 15, 16, 17, 18 Mutations in these genes have been observed in patients with USH1 from various ethnic origins, including Caucasian, African and Asian.19 However, there have been no reports of mutation analysis for any responsible genes for USH1 in Japanese patients.
Of the five causative genes, the mutation frequency of MYO7A is the highest (39–55% of the total cases), followed by that of CDH23 (19–35% of the total cases).20, 21 These two genes account for approximately 70–80% of the USH1 cases that have been analyzed.20, 21
The aim of this study was to analyze mutations in the MYO7A and CDH23 genes in Japanese patients with USH1.
Materials and methods
Subjects and diagnosis
Five unrelated Japanese patients (C103, C224, C312, C517 and C720) from various regions of Japan were referred to Hamamatsu University School of Medicine for genetic diagnosis of USH. All patients met the following criteria for USH1: RP, congenital severe-to-profound HL and vestibular dysfunction.8 The clinical evaluation of the affected patients consisted of elicitation of the medical history, and ophthalmological and audiovestibular examinations. The medical history included the age at onset of walking, age at diagnosis of HL, nature of HL and age at diagnosis of RP.
The ophthalmological evaluation consisted of best-corrected visual acuity measurement, slit-lamp microscopy, ophthalmoscopy, Goldmann perimetry and electroretinography. Visual fields were evaluated by Goldmann perimetry of both eyes, and the isopters for the V/4e, III/4e and I/4e test targets were measured. Electroretinography was performed according to the International Society for Clinical Electrophysiology of Vision protocol.22
The auditory examination consisted of otoscopy, pure-tone audiometry (125–8000 Hz) and tympanometry. The severity of HL was classified using the pure-tone average over 500, 1000, 2000 and 4000 Hz in the better hearing ear as follows: normal hearing, <20 dB; mild HL, 21–40 dB; moderate HL, 41–70 dB; severe HL, 71–90 dB; and profound HL, >91 dB.
Vestibular function was evaluated on the basis of the medical history concerning childhood motor development and the results of caloric tests. Caloric stimulation of each ear was performed with cold water (20 °C, 5 ml) and the results were classified according to the peak slow-phase velocity as follows: normal, ⩾20°/s; canal paresis, <20°/s.23 For the patient diagnosed with canal paresis, stronger stimulation with iced water (4 °C, 5 ml) was used to determine the presence of a residual response.
For all patients, parent samples were obtained for segregation analysis. A set of 135 control subjects, selected from Japanese individuals with no visual or hearing impairment, was used to assess the frequency of nucleotide sequence variations. The institutional review board of Hamamatsu University School of Medicine approved this study, and written informed consent was obtained from all subjects before enrollment.
Mutation analysis
Genomic DNA was extracted from peripheral lymphocytes by using standard procedures. In brief, the DNA samples were first screened for mutations in MYO7A, and the negative cases were screened for CDH23 mutations. All exons (MYO7A, 49 exons; CDH23, 69 exons) and their flanking sequences were amplified by PCR. The PCR products were purified with Wizard SV Gel and PCR Clean-Up System (Promega, Madison, WI, USA) or treated with Exonuclease I and Antarctic Phosphatase (New England Biolabs, Ipswich, MA, USA). Direct sequencing was performed using the BigDye Terminator version 3.1 Cycle Sequencing Kit on an ABI 3100 Autosequencer (Applied Biosystems, Foster City, CA, USA). PCR amplification of MYO7A was performed using the primers described by Kumar et al.24 with a slight modification. The PCR primers for CDH23 amplification were newly designed. Information of the nucleotide sequence and appropriate annealing condition of all primers for PCR and sequencing is available on request. Using direct sequencing or restriction enzyme-based assay, we tested the Japanese control chromosomes for all the novel mutations identified during the mutation analysis.
Reverse-transcription PCR of CDH23
Reverse-transcription PCR (RT–PCR) of CDH23 was preformed using total RNA extracted from hair roots as described previously.25 The PCR primers were newly designed: forward primer, GCTTTTGGTGCTGATCTCTGGATGC located in exon 1; reverse primer, TGGTCGCTGACAGAGAACTCCACG in exon 4. The amplification condition was as follows: denaturation at 94 °C for 2 min; 40 cycles of treatment at 98 °C for 10 s, 64 °C for 30 s and 68 °C for 1 min; and final extension at 68 °C for 5 min.
Results
Mutation analysis
Mutation analysis of MYO7A and CDH23 in the five unrelated Japanese patients revealed five probable pathogenic mutations in four patients (Tables 1 and 2; Figure 1). Of these, two mutations (p.Tyr1942SerfsX23 in CDH23 and p.Ala771Ser in MYO7A) were novel (Table 2). The former was a large deletion affecting 3 exons (Figure 2). The mutation was found in a homozygous state, which is probably accounted by consanguinity (Supplementary Figure 1). As the deletion caused the loss of 3 exons, resulted in a frameshift generating a premature stop codon at 23-codon downstream and was not identified in 64 control chromosomes, it was considered pathogenic. The other novel mutation (p.Ala771Ser in MYO7A) was considered pathogenic because it was not detected in 270 control chromosomes and Ala771 has been found to be almost conserved in various vertebrates (Table 2). Another mutation in patient C103 remained unclear. The remaining mutations (p.Arg150X and p.Arg1883Gln in MYO7A, and p.Arg2107X in CDH23) were previously reported and none of them was detected in the Japanese control chromosomes (Table 2).
(a) Schema of myosin VIIa domains with mutations identified in MYO7A. The p.Arg150X, p.Ala771Ser and p.Arg1883Gln mutations were located in the Motor domain, IQ motif and MyTH4 domain, respectively. IQ, isoleucine-glutamine motif; CC, coiled-coil domain; MyTH4, myosin tail homology 4 domain; FERM, 4.1, ezrin, radixin, moesin domain; SH3, Src homology 3 domain. (b) Schema of cadherin 23 domains with mutations identified in CDH23. The p.Tyr1942SerfsX23 mutation changed Tyr1942 located in EC18 to Ser and created a premature stop codon at 23-codon downstream. The p.Arg2107X mutation was located in EC20. EC, extracellular domain; TM, transmembrane domain.
Schema of mutation p.Tyr1942SerfsX23 in the CDH23 gene. The deletion occurred between introns 43 and 46, and both boundaries had 20-nucleotide sequence string GCTAATTTTTGTATTTTTAG. Upstream and downstream strings were located between c.5821-2280 and c.5821-2261 and between c.6253+403 and c.6253+422, respectively. Although the precise breakpoints could not be determined, the deletion size was elucidated to be 5078 nucleotides. The deletion was notated as c.5821-?_6253+?del5078. The boxes with a number represent exons. The distance between exons does not indicate the actual intronic sizes. The open arrowheads indicate the primer pairs used for PCR to amplify exons 43–47.
In addition to the probable pathogenic mutations listed in Table 2, various sequence alterations were identified in MYO7A and CDH23 (Table 3; Supplementary Tables 1 and 2). These alterations were predicted to be nonpathogenic for various reasons. Some of them have been reported as polymorphism in previous reports (Supplementary Tables 1 and 2). The newly identified alteration in exon 30 of MYO7A (p.Pro1261Pro) was also found in the control chromosomes. The newly found alterations in introns, except for c.68-3C>T in CDH23 of patient C224, were distant from splicing donor or acceptor sites. The exception was not detected in any of the 270 control chromosomes but was considered benign because the RT–PCR analysis revealed that the alteration had no influence on splicing (Figure 3).
Products of reverse-transcription PCR (RT–PCR) performed using primers to amplify CDH23 complementary DNA (cDNA) between exons 1 and 4. Agarose gel electrophoresis of the RT–PCR products revealed a single band with the proper size predicted from the normal sequence, indicating that the nucleotide change (c.68-3C>T) had no effect on splicing and was presumably nonpathogenic. PCR was performed using 2 μg cDNA (total volume, 20 μl) with 40 cycles. The boxes with a number represent exons. The distance between exons does not indicate the actual intronic sizes. The open arrowheads indicate the PCR primers, and the arrow indicates the nucleotide change. M, molecular marker (100-bp ladder); C, control; P, patient.
Clinical findings
All four patients in whom at least one mutant allele was detected had been diagnosed with RP by ophthalmologists at ages 3–27 years (mean±s.d., 13.0±10.1 years; Table 1). In all the patients, the visual fields were symmetrically constricted, pigmentary degeneration was typical of RP with peripheral bone-spicule pigmentation and standard combined electroretinography was extinguished. The best-corrected visual acuity ranged from 0.7 to 0.1. Two patients (C312 and C103) reported having cataracts, but none underwent cataract surgery.
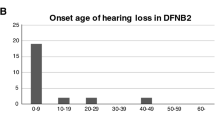
The patients were diagnosed with hearing impairment by otorhinolaryngologists at ages 2–3 years (2.3±0.5 years; Table 1). Despite using hearing aids immediately after the diagnosis, all the patients did not develop speech ability and used sign language to communicate. Tympanometry yielded normal results, consistent with the clinical findings of a normal tympanic membrane and middle ear cavity. Audiograms showed bilateral profound sensorineural HL in all the patients. None of the patients complained of progressive HL.
All the patients reported delayed walking, with starting ages ranging from 18 to 24 months (22±2.8 months; Table 1). The caloric test with cold water revealed canal paresis in all the patients, and no response was induced with the iced water. These results indicated that all the patients had congenital vestibular dysfunction.
Discussion
This is the first report on mutation analysis of MYO7A and CDH23 in Japanese patients with USH1. We found at least one mutant allele in four of the five patients in either of the genes. Although the number of patients examined was small, this frequency (80%) is similar to that among Caucasians, indicating that mutation screening for these genes is a highly sensitive method for diagnosing USH1 among the Japanese.
Of the five mutations identified in this study, three mutations (p.Arg150X and p.Arg1883Gln in MYO7A, and p.Arg2107X in CDH23) were previously identified in European-Caucasians.12, 21, 26 All of these mutations occurred by transition (C/G → T/A) at CpG sites and were considered to be recurrent, which meets the fact that they are not specific to a particular ethnic group. This finding is consistent with a result of an analysis by Baux et al.,27 who reported that a high proportion of MYO7A and CDH23 mutations are represented by single base-pair substitutions and that 51.5 and 48.5% of them in MYO7A and CDH23, respectively, involve a CpG dinucleotide. Interestingly, neither of the two novel mutations found in the present study is of the transition type.
Mutation p.Tyr1942SerfsX23 (in CDH23) was found by PCR using a specially designed primer pair far distant from each other. After failing to amplify each of exons 44–46 in patient C517, we hypothesized the homozygous deletion of a long genomic region including at least exons 44–46. We successfully obtained an amplified product using a primer pair, one (forward) in intron 42 and the other (reverse) in intron 47 (Figure 2). Sequence analysis showed that the amplified DNA contains intact exon 43, truncated intron 43, truncated intron 46 and intact exon 47, indicating a deletion from introns 43 to 46. The boundary between truncated introns 43 and 46 had 20-nucleotide sequence string GCTAATTTTTGTATTTTTAG. Interestingly, the same 20-nucleotide sequences exist in normal introns 43 and 46, and lie within AluSx repetitive sequences. It is speculated that the deletion occurred with Alu-mediated recombination. We could not determine the precise breakpoints in both introns because of the exact sequence identity around possible breakpoints, but the deletion size was elucidated to be 5078 nucleotides regardless of the position of break. We notated the deletion as c.5821-?_6253+?del5078 according to a nomenclature guideline recommended by the Human Genome Variation Society (http://www.hgvs.org/mutnomen/).28
The deleted sequence in p.Tyr1942SerfsX23 included exons 44, 45 and 46 (103, 126 and 204 nucleotides long, respectively) and the total deletion size in mRNA was 433 nucleotides. Therefore, the mutation was presumed to create a premature stop codon at 23-codon downstream in exon 47 by a frameshift. This is the first large deletion to be found in CDH23. We could detect the mutation because of the loss of the same exons in both alleles by consanguinity. However, a large deletion of this type in only one allele cannot be easily detected by PCR because of the existence of the normal allele. In addition, we found a mutation p.Arg2107X in CDH23 of patient C720. Both of these mutations are of a truncated type (nonsense, deletion/insertion with frameshift, or splicing). This finding is consistent with the previously reported genotype/phenotype relationship for CDH23: at least one of the two mutations is of a truncated type in USH1 cases, and both mutations are of a missense type in nonsyndromic HL cases.29
In conclusion, the mutation analysis of MYO7A and CDH23 led to the identification of five mutations in four patients. This frequency (80%) indicates that mutation screening for these genes is a highly sensitive method for diagnosing USH1 among the Japanese. One novel mutation, p.Tyr1942SerfsX23 of CDH23, was a large deletion causing the loss of 3 exons: the homozygosity resulting from consanguinity probably led to the relatively easy identification. It is possible that similar exonal deletions latently exist in a compound heterozygous state in some USH1 cases in which only one mutation has been found.
References
Yan, D. & Liu, X. Z. Genetics and pathological mechanisms of Usher syndrome. J. Hum. Genet. 55, 327–335 (2010).
Nuutila, A. Dystrophia retinae pigmentosa––dysacusis syndrome (DRD): a study of the Usher or Hallgren syndrome. J. Genet. Hum. 18, 57–88 (1970).
Boughman, J. A., Vernon, M. & Shaver, K. A. Usher syndrome: definition and estimate of prevalence from two high-risk populations. J. Chronic Dis. 36, 595–603 (1983).
Grondahl, J. Estimation of prognosis and prevalence of retinitis pigmentosa and Usher syndrome in Norway. Clin. Genet. 31, 255–264 (1987).
Hope, C. I., Bundey, S., Proops, D. & Fielder, A. R. Usher syndrome in the city of Birmingham: prevalence and clinical classification. Br. J. Ophthalmol. 81, 46–53 (1997).
Rosenberg, T., Haim, M., Hauch, A- M. & Parving, A. The prevalence of Usher syndrome and other retinal dystrophy-hearing impairment associations. Clin. Genet. 51, 314–321 (1997).
Spandau, U. H. & Rohrschneider, K. Prevalence and geographical distribution of Usher syndrome in Germany. Graefes Arch. Clin. Exp. Ophthalmol. 240, 495–498 (2002).
Kimberling, W. J. & Möller, C. Clinical and molecular genetics of Usher syndrome. J. Am. Acad. Audiol. 6, 63–72 (1995).
Tsilou, E. T., Rubin, B. I., Caruso, R. C., Reed, G. F., Pikus, A., Hejtmancik, J. F. et al. Usher syndrome clinical types I and II: could ocular symptoms and signs differentiate between the two types? Acta Ophthalmol. Scand. 80, 196–201 (2002).
Pennings, R. J. E., Huygen, P. L. M., Orten, D. J., Wagenaar, M., van Aarem, A., Kremer, H. et al. Evaluation of visual impairment in Usher syndrome 1b and Usher syndrome 2a. Acta Ophthalmol. Scand. 82, 131–139 (2004).
Grøndahl, J. & Mjøen, S. Usher syndrome in four Norwegian countries. Clin. Genet. 30, 14–28 (1986).
Weil, D., Blanchard, S., Kaplan, J., Guilford, P., Gibson, F., Walsh, J. et al. Defective myosin VIIA gene responsible for Usher syndrome type 1B. Nature 374, 60–61 (1995).
Bitner-Glindzicz, M., Lindley, K. J., Rutland, P., Blaydon, D., Smith, V. V., Milla, P. J. et al. A recessive contiguous gene deletion causing infantile hyperinsulinism, enteropathy and deafness identifies the Usher syndrome 1C gene. Nat. Genet. 26, 56–60 (2000).
Verpy, E., Leibovici, M., Zwaenepoel, I., Liu, X. Z., Gal, A., Salem, N. et al. A defect in harmonin, a PDZ domain-containing protein expressed in the inner sensory hair cells, underlies Usher syndrome type 1C. Nat. Genet. 26, 51–55 (2000).
Bolz, H., von Brederlow, B., Ramirez, A., Bryda, E. C., Kutsche, K., Nothwang, H. G. et al. Mutation of CDH23, encoding a new member of the cadherin gene family, causes Usher syndrome type 1D. Nat. Genet. 27, 108–112 (2001).
Ahmed, Z. M., Riazuddin, S., Bernstein, S. L., Ahmed, Z., Khan, S., Griffith, A. J. et al. Mutations of the protocadherin gene PCDH23 cause Usher syndrome type 1F. Am. J. Hum. Genet. 69, 25–34 (2001).
Alagramam, K. N., Yuan, H., Kuehn, M. H., Murcia, C. L., Wayne, S., Srisailpathy, C. et al. Mutations in the novel protocadherin PCDH15 cause Usher syndrome type 1F. Hum. Mol. Genet. 10, 1709–1718 (2001).
Weil, D., El-Amraoui, A., Masmoudi, S., Mustapha, M., Kikkawa, Y., Laine, S. et al. Usher syndrome type IG (USH1G) is caused by mutations in the gene encoding SANS, a protein that associates with the USH1C protein, harmonin. Hum. Mol. Genet. 12, 463–471 (2003).
Ahmed, Z. M., Riazuddin, S., Riazuddin, S. & Wilcox, E. R. The molecular genetics of Usher syndrome. Clin. Genet. 63, 431–444 (2003).
Roux, A- F., Faugère, V., Le Guèdard, S., Pallares-Ruiz, N., Vielle, A., Chambert, S. et al. Survey of the frequency of USH1 gene mutations in a cohort of Usher patients shows the importance of cadherin 23 and protocadherin 15 genes and establishes a detection rate of above 90%. J. Med. Genet. 43, 763–768 (2006).
Ouyang, X. M., Yan, D., Du, L. L., Hejtmancik, J. F., Jacobson, S. G., Nance, W. E. et al. Characterization of Usher syndrome type I gene mutations in an Usher syndrome patient population. Hum. Genet. 116, 292–299 (2005).
Marmor, M. F., Holder, G. E., Seeliger, M. W. & Yamamoto, S. Standard for clinical electroretinography (2004 update). Doc. Ophthalmol. 108, 107–114 (2004).
Nakanishi, H., Ohtsubo, M., Iwasaki, S., Hotta, Y., Mizuta, K., Mineta, H. et al. Identification of 11 novel mutations in USH2A among Japanese patients with Usher syndrome type 2. Clin. Genet. 76, 383–391 (2009).
Kumar, A., Babu, M., Kimberling, W. J. & Venkatesh, C. P. Genetic analysis of a four generation Indian family with Usher syndrome: a novel insertion mutation in MYO7A. Mol. Vis. 10, 910–916 (2004).
Nakanishi, H., Ohtsubo, M., Iwasaki, S., Hotta, Y., Mizuta, K., Mineta, H. et al. Hair roots as an mRNA source for mutation analysis of Usher-syndrome causing genes. J. Hum. Genet. 55, 701–703 (2010).
Bork, J. M., Peters, L. M., Riazuddin, S., Bernstein, S. L., Ahmed, Z. M., Ness, S. L. et al. Usher syndrome 1D and nonsyndromic autosomal recessive deafness DFNB12 are caused by allelic mutations of the novel cadherin-like CDH23. Am. J. Hum. Genet. 68, 26–37 (2001).
Baux, D., Faugère, V., Larrieu, L., Le Guèdard-Mèreuze, S., Hamroun, D., Bèroud, C. et al. UMD-USHbases: a comprehensive set of databases to record and analyse pathogenic mutations and unclassified variants in severe Usher syndrome causing genes. Hum. Mutat. 29, E76–E87 (2008).
den Dunnen, J. T. & Antonarakis, S. E. Mutation nomenclature extensions and suggestions to describe complex mutations: a discussion. Hum. Mutat. 15, 7–12 (2000).
Astuto, L. M., Bork, J. M., Weston, M. D., Askew, J. W., Fields, R. R., Orten, D. J. et al. CDH23 mutation and phenotype heterogeneity: a profile of 107 diverse families with Usher syndrome and nonsyndromic deafness. Am. J. Hum. Genet. 71, 262–275 (2002).
Acknowledgements
We thank all the subjects who participated in the study. This work was supported by research grants from the Ministry of Health, Labour and Welfare (Acute Profound Deafness Research Committee) and the Ministry of Education, Culture, Sports, Science and Technology (Young Scientists Grant B-22791589) in Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Nakanishi, H., Ohtsubo, M., Iwasaki, S. et al. Mutation analysis of the MYO7A and CDH23 genes in Japanese patients with Usher syndrome type 1. J Hum Genet 55, 796–800 (2010). https://doi.org/10.1038/jhg.2010.115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2010.115
Keywords
This article is cited by
-
Comprehensive genetic testing improves the clinical diagnosis and medical management of pediatric patients with isolated hearing loss
BMC Medical Genomics (2022)
-
New splice site mutations in MYO7A causing Usher syndrome type 1: a study on a Chinese consanguineous family
International Ophthalmology (2022)
-
Novel USH2A mutations in Japanese Usher syndrome type 2 patients: marked differences in the mutation spectrum between the Japanese and other populations
Journal of Human Genetics (2011)