Abstract
Proinflammatory cytokine gene polymorphisms have been demonstrated to associate with gastric cancer risk, of which IL1B−31T/C and −511C/T changes have been well investigated due to the possibility that they may alter the IL1B transcription. The signal transduction target upon interleukin 1 beta (IL1β) stimulation, the nuclear factor of kappa B (NFκB) activation, supports cancer development, signal transduction in which is mediated by FS-7 cell-associated cell surface antigen (FAS) signaling. Based on recent papers describing the prognostic roles of the polymorphisms and the NFκB functions on cancer development, we sought to determine if Japanese gastric cancer patients were affected by the IL1B −31/−511 and FAS−670 polymorphisms. A case-control study was conducted on incident gastric adenocarcinoma patients (n=271) and age–gender frequency-matched control subjects (n=271). We observed strong linkage disequilibrium between the T allele at −511 and the C allele at −31 and between the C allele at −511 and the T allele at −31 in IL1B in both the cases and controls (R 2=0.94). Neither IL1B−31, −511 nor FAS−670 polymorphisms showed significantly different risks of gastric adenocarcinoma. Though FAS−670 polymorphisms did not show any significant difference, the proportion of subjects with IL1B−31TT (or IL1B−511CC) increased according to stage (trend P=0.019). In particular, subjects with stage IV had a two times higher probability of having either IL1B−31TT (or IL1B−511CC) genotype compared with stage I subjects. These observations suggest that IL1B−31TT and IL1B−511CC are associated with disease progression.
Similar content being viewed by others
Introduction
Chronic inflammation appears to support the formation of epithelial tumors by which a causal relationship between inflammation and cancer has long been suspected. As described in earlier studies, tumor promotion and progression appear to be maintained by the interaction between transformed cells and their close surrounding cells as innate immune cells, fibroblasts, and endothelial cells in chronic inflammation although the exact mechanism is almost unknown (Cordon-Cardo and Prives 1999; Balkwill and Mantovani 2001; Clevers 2004). Accumulated information on chronic inflammation of gastric mucosa has revealed that infection by the gram-negative bacteria Helicobacter pylori (HP) is one of the causative factors in gastric carcinogenesis (Group 2001; Uemura et al. 2001; Peek and Blaser 2002).
Another characteristic feature of gastric cancer risk appears to be mediated by polymorphisms of IL1B, one of the proinflammatory cytokines induced on inflammation. Indeed, since a first report demonstrated the positive association between higher gastric cancer risk and IL1B−31C allele in patients in the United States (El-Omar et al. 2000, 2001), epidemiological studies in Portugal (Machado et al. 2003), China (Zeng et al. 2003), the United States (El-Omar et al. 2003), and Mexico (Sicinschi et al. 2006) have demonstrated supportive evidence on either IL1B−31C or IL1B−511T that is genetically linked with IL1B−31C. Concerning biological functions of the polymorphism, a first report indicated that IL1B−31C to T change generates a TATA sequence providing a transcriptional factor binding element at −31IL1B gene (El-Omar et al. 2000) and that no increased binding of transcription factor was seen among IL1B−31C, ILB−511C, and IL1B−511T in human monocytes by lipopolysaccharide (LPS) stimulation (El-Omar et al. 2000). Through the original (El-Omar et al. 2000) and the erratum articles (El-Omar et al. 2001), IL1B−31T was finally suggested for the probable hypo interleukin 1 beta (IL1β) production allele. Indeed, this finding was supported by in vivo studies demonstrating that the IL1B−31C allele was a higher IL1β protein secretion allele than the IL1B−31T allele (Hwang et al. 2002; Hall et al. 2004). However, inconsistent epidemiological results on ILB−511C linked with IL1B−31T were also reported from Chinese (Yang et al. 2004), Italian (Palli et al. 2005), and Korean cancer patients (Chang et al. 2005), and a higher production of IL1β or transcription of the IL1B gene was also reported in IL1B−31T allele in in vivo (Chang et al. 2005; Xuan et al. 2005) and in vitro (Kimura et al. 2004) studies. Thus, the exact biological role of the nucleotide substitutions on gastric cancer risk remains unclear.
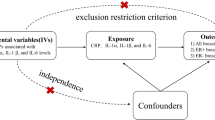
Signaling through IL1β and the receptor IL1R is generally believed the main response to the infection, and mucosal injury generates transcriptional activation through the nuclear factor kappa B (NFκB) that belongs to the reticulo-endotheliosis (Rel) family of proteins (Karin et al. 2002; Senftleben and Karin 2002; Lin and Karin 2003; Bonizzi and Karin 2004). NFκB is also a key player in anti-apoptotic function (Balkwill and Mantovani 2001; Karin et al. 2002; Lin and Karin 2003; Bonizzi and Karin 2004; Clevers 2004) in which activation correlates with gastric cancer (Sasaki et al. 2001) and colitis-associated cancer development (Greten and Karin 2004). Because the activation is needed to generate a microenvironment helping the progression of transformed cells, cancer progression appears to be promoted by the activation. The activation signaling pathway can be mediated by the dissociation between myeloid differentiation factor 88 (MyD88) and FS-7 cell-associated cell surface antigen (FAS) (CD95; Apo-1)-associated death domain protein (FADD) due to ligation and oligomerization by FAS ligand (Ma et al. 2004). FAS ligation on macrophages promotes chronic inflammation. As the FAS−670 polymorphism was demonstrated to alter the amounts of expression (Huang et al. 1997; Kanemitsu et al. 2002; Sibley et al. 2003), we hypothesized that the polymorphism might associate with the NFκB activation magnitude.
In this study, we sought to determine if Japanese patients were affected by the polymorphism of IL1B at −31 and −511 positions in a case-control study, and further, whether the risk was also altered by the FAS−670 polymorphism. We show that although these polymorphisms are not associated with gastric cancer risk, IL1B at −31 and −511 polymorphisms may be associated with disease progression while the FAS−670 polymorphism was neutral for the risk per se.
Materials and methods
Subjects
We have reported in detail elsewhere our ongoing Hospital-based Epidemiologic Research Program at Aichi Cancer Center (HERPACC) featuring a self-administered questionnaire completed by first-visit outpatients at the Aichi Cancer Center Hospital (ACCH) (Hamajima et al. 2001a, b). In this framework, more than 95% of all first-visit outpatients have participated in the questionnaire study, and approximately 60% of them agreed to provide blood samples. Before diagnosis, subjects completed a questionnaire with items including lifestyle factors. Subjects in the present study were enrolled between February 2001 and December 2003 in the framework of HERPACC. Among them, subjects diagnosed pathologically as having adenocarcinoma of the stomach were recruited as cases in this study. A total of 271 noncancer controls, patients who had visited ACCH during the same period and had never been diagnosed as having cancer, were frequency-matched for age–gender strata (age <45, 45–54, 55–65, 65–74, and 75 or older according to gender) with cancer subject cases. After providing written informed consent, study subjects donated a 7-ml sample of peripheral venous blood. Genomic DNA was extracted from the blood samples, as described previously (Ikehara et al. 1998, 2001). This study was approved by the Institutional Review Board of Aichi Cancer Center.
Genotyping
Genotypes of IL1B−31T/C were determined by polymerase chain reaction with confronting two-pair primers (PCR-CTPP) (Hamajima et al. 2001a, b). PCR-CTPP was performed in 25 μl of PCR mixture containing 25 pmol each of four primers (IL1B−31 F1: 5′-ACTTCTGCTTTTGAAAGCC-3′; IL1B−31 R5: 5′-TCAGCTGTTAGATAAGCAGTATC-3′; IL1B−31 F4: 5′-AATGTGGACATCAACTGCA-3′; IL1B−31 R2: 5′-CTCCCTCGCTGTTTTTATA-3′), 200 μM dNTPs, 1.0 mM MgCl2, 50 mM KCl2, 10 mM Tris–HCl (pH 8.5), and 0.5 U AmpliTaq Gold polymerase (PE Applied Biosystems, NJ, USA) under 35 thermal cycling conditions consisting of 1 min at 94°C for denaturing, 1 min at 54°C for annealing, and 1 min at 72°C for extension. PCR product was resolved in 2.0% agarose gels containing ethidium bromide. The genotype was determined under ultraviolet (UV) illumination, with a C allele fragment length of 345 bp and T allele of 266 bp. Genotypes of IL1B−511C/T were determined by PCR-based restriction fragment length polymorphism (PCR-RFLP) using specific primer pairs (IL1B−511 F1: 5′-GCATTGATCTGGTTCATCCATG-3′; IL1B−511 R: 5′-GTTCATGGAAGGGCAAGGAG-3′). The reaction was performed in 200 μM dNTPs, 1.0 mM MgCl2, 50 mM KCl2, 10 mM Tris–HCl (pH 8.5), and 0.5 U AmpliTaq Gold polymerase (PE Applied Biosystems) under 35 thermal cycling conditions of 90 s at 95°C for denaturing, 90 s at 56°C for annealing, and 1 min at 72°C for extension. AvaI restriction enzyme-digested product was resolved in 2.0% agarose gels containing ethidium bromide. The genotype was determined under UV illumination, with a T allele fragment length of 530 bp and C allele fragments of 190 and 340 bp that were digested by AvaI. FAS−670 was determined by PCR-RFLP using specific primer pairs (Fas F: 5′-CTACCTAAGAGCTATCTACCGTTC-3′; Fas R: 5′-GGCTGTCCATGTTGTGGCTGC-3′) (Kanemitsu et al. 2002). The reaction was performed in 200 μM dNTPs, 1.0 mM MgCl2, 50 mM KCl2, 10 mM Tris–HCl (pH 8.5), and 0.5 U AmpliTaq Gold polymerase (PE Applied Biosystems) under 35 thermal cycling conditions of 30 s at 95°C for denaturing, 1 min at 58°C for annealing, and 1 min at 72°C for extension. MvaI restriction enzyme-digested product was resolved in 2.0% agarose gels containing ethidium bromide. The genotype was determined under UV illumination, with a G allele fragment length of 188 bp and A allele of 232 bp.
Statistical analysis
A chi-squared test and exact test were applied to test distribution difference, as well as Hardy–Weinberg disequilibrium when appropriate. The continuous values were tested with Wilcoxon’s signed rank test or t test according to variable distribution. An unconditional logistic regression model was applied to calculate age–gender-adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for IL1B−31, IL1B−511, and FAS−670 genotypes. An ordinal logistic regression was applied to evaluate the impact of genotypes on clinical stage (I, II, III and IV). We defined P value less than 0.05 as statistically significant. In each multivariate model, age was treated as a continuous variable and gender was treated as indicator variable. All analyses were conducted with STATA ver.8 (STATA Corp., College Station, TX, USA).
Results
Subject characteristics are summarized in Table 1. There was no statistically significant difference between patients and controls in terms of age and gender, indicating that the age–gender strata matching was adequate. Although not statistically significant, ever smokers were relatively dominant among cases rather than controls. Distributions of clinical stages on 271 gastric cancers were as follows: 154 for stage I (56.8%), 20 for II (7.4%), 29 for III (10.7%), and 68 for IV (25.1%).
Initial experiments were performed to determine polymorphisms of IL1B−31, IL1B−511, and FAS−670 in subjects using the PCR technique, and genotype distributions are presented in Table 2. IL1B−31C/C was inversely associated with IL1B−511T/T. Allele frequencies for FAS−670G and IL1B−31C were 51.1% and 44.8% in cases and 49.8% and 45.4% in control subjects. No significant deviations in control subjects were seen in observed genotype frequencies of FAS−670 G to A, IL1B−31C to T, and IL1B−511T to C polymorphisms, inferring the expected results from the Hardy–Weinberg equilibrium (P=0.22, 0.54, and 0.26, respectively). As expected, a tight linkage disequilibrium was observed between IL1B−31C to T and IL1B−511T to C polymorphisms. Coefficients for linkage disequilibrium were D′ 0.97 and R 2 0.94.
To detect a possible association between polymorphisms and gastric cancer risks, we compared allele frequencies among IL1B−31C/T, IL1B−511T/C, and FAS−670 G/A genotypes among case patients and control subjects (Table 2). We did not find any significant difference between cases and controls in terms of genotype distributions. To evaluate the risk for gastric cancer according to genotypes, an unconditional logistic regression model analysis adjusted for age and gender was performed. Results demonstrated that both IL1B−31C/T and IL1B−511T/C polymorphisms were neutral in terms of the risk of gastric carcinogenesis in our study. No increasing OR was seen in FAS−670 G to A polymorphisms on gastric cancer risk.
Since some studies pointed out a smoking habit mildly associated with increased gastric cancer risks, we evaluated the possibility of whether or not a higher individual smoking status may have caused an increasing risk by the polymorphism in the Japanese population. Regarding the FAS−670 polymorphism, smokers harboring the G allele showed a statistically significant increased risk of gastric cancer (OR=1.70, 95% CI 1.04–2.79) whereas no such effect was observed in never smokers (OR=0.74, 95% CI 0.37–1.50) compared with patients with FAS−670 A allele homozygote in ever-smoker patients. However, we could not find any effect modification due to smoking habit for IL1B−31 and IL1B−511 polymorphisms. These results suggest that persons with the FAS−670 G allele exhibited a higher transcriptional activity on the FAS gene showing susceptibility to gastric cancer in terms of their smoking habit and that the IL1B−31C allele linking with IL1B−511T did not cause an increase in the risk of gastric adenocarcinoma in the Japanese population.
To determine why the positive association between IL1B−31C allele and gastric cancer risk was not seen in Japanese populations despite its presence in Caucasians, we further explored the association between the tumor, node, metastases (TNM) stage of gastric cancer and IL1B and FAS genotypes. Of 271 gastric cancer cases, 56.8% (154 cases) were in stage I while 43.2% (117 cases) were classified in stages II–IV. Frequencies for homozygous alleles, IL1B−31T, IL1B−511C, and FAS−670G were 24.7, 24.0, and 24.0% among stage I and 36.8, 34.5, and 24.7% among stages II–IV, respectively, demonstrating an accumulation of the IL1B−31TT and IL1B−511CC genotype in stages II–IV. As shown in Table 3, the proportion of subjects with both IL1B−31TT and IL1B−511CC increased according to stage (trend P=0.019, trend P=0.040). In particular, subjects with stage IV showed a two times higher probability of having the IL1B−31TT genotype compared with stage I subjects. However, this trend was not observed for the FAS polymorphism. This might suggest that the IL1B−31C/T polymorphism, linking with IL1B−511T/C, has a specific impact on the progression of gastric cancer.
Discussion
Through this case-control study, we found evidence that the progression of gastric adenocarcinoma is enhanced by the presence of the IL1B−31T allele that is strongly linked with IL1B−511C. Although it remains to be elucidated whether cancer tissues of subjects with IL1B−31T express IL1β rather than those of subjects with IL1B−31C, the present results demonstrated a causal relationship between advanced gastric adenocarcinoma and the IL1B−31T allele.
The first implication of this study is that the presence of the IL1B−31T allele has a higher risk for advanced gastric cancer in the Japanese population. The overall results did not demonstrate accumulation of any alleles in Japanese gastric cancer patients while we found an increased frequency of IL1B−31TT but not for IL1B−31CC in patients with advanced gastric cancer defined as greater than stage II. This was corroborated by the fact that IL1B−31TT was strongly linked with IL1B−511CC that was inversely increased in advanced gastric cancer patients. Therefore, the IL1B−31T allele is associated with the risk of cancer progression and may be considered to be a higher IL1β productive allele. In support of this possibility, the in vivo (Chang et al. 2005; Xuan et al. 2005) and in vitro (Kimura et al. 2004) experiments of earlier studies were consistent with higher production of IL1β by IL1B−31T allele. On the other hand, IL1B polymorphisms were not significantly different between the control and stage IV gastric cancer. Moreover, P value of CC versus CT and TT between control and stage I was lowest (P=0.08). This is not consistent with the result that these polymorphisms associated with gastric cancer progression. It is reasonable to consider the result was due to the bias of patient. And further, the higher transcriptional activity on IL1B−31C than IL1B−31T reportedly corresponded to a higher risk of gastric cancer in Portugal (Machado et al. 2003), China (Zeng et al. 2003), the United States (El-Omar et al. 2003), and Mexico (Sicinschi et al. 2006), and no mention was made as to any associations between TMN stages and the genotypes. This controversial issue should be addressed in further biochemical and epidemiological studies on IL1B polymorphisms.
The second implication of this study is that FAS−670A/G polymorphism does not interact with the risk of either incidence or development of gastric adenocarcinoma. A-to-G substitution at FAS−670 altered FAS transcriptional activity by the disruption of STAT1 binding sequence, the polymorphism of which was earlier pointed out to be associated with the risk of esophageal squamous cell carcinoma (Sun et al. 2004) and acute myeloid leukemia (Sibley et al. 2003). However, the results of our case-control study did not support this hypothesis, presumably because not all gastric tumors express FAS as reported (positive cases up to 30% of gastric cancer) (Vollmers et al. 1997; Osaki et al. 2001). Based on previous epidemiological studies of the polymorphism, the positive and negative correlation between the polymorphism and a risk of cervical squamous cell carcinoma has been disregarded (Lai et al. 2003; Engelmark et al. 2004). Immunohistochemical analysis using pathological specimens would help to provide a biological explanation to resolve this discrepancy.
Among the potential methodological limitations of the present study, one issue is admittedly the selection of the base population for controls. We recruited noncancer patients at the ACCH for this purpose because it is reasonable to assume our cases arose within this population base. A notable characteristic of our control population is its similarity to the general population in terms of exposure of interest, in this case smoking and drinking (Inoue et al. 1997). Similarity in genotype distribution for the IL1B−31C/T polymorphism between our controls and the general population has also been reported (Yoshimura et al. 2003). No previous report in terms of the FAS polymorphism is another limitation. The medical background of controls is still another potential source of bias; however, our previous study focusing on women demonstrated a limited impact. More than 66% of noncancer outpatients at ACCH do not have any specific medical condition. The remaining 34% have specific diseases, such as benign tumors and/or nonneoplastic polyps (13.1%), mastitis (7.5%), digestive disease (4.1%), or benign gynecological disease (4.1%) (Hamajima et al. 1995). As for men, the circumstances are similar although not reported. This situation is very different from that in other developed countries where people visit local general clinics first and are then referred to hospitals that function as secondary and/or specific facilities for further medical treatment. We conclude, therefore, that it is feasible to use noncancer outpatients at ACCH as referents in HERPACC-type epidemiological studies. In addition, the present study was free of questionnaire response information bias because all data were collected prior to diagnoses. Our case-control study has a statistical power of more than 90% under the assumption that the proportion of subjects with IL1B or FAS genotype of interest is 25–30% and OR for those genotypes is 2.0. Therefore, there is no conclusive risk of an association between IL1B/FAS polymorphisms and gastric cancer. However, the association between IL1B and stage should be carefully interpreted because the analysis was made in an exploratory fashion.
Yet another potential limitation was not being able to examine HP infection status. HP infection is known to induce chronic inflammation and IL1β expression to activate NFκB that can promote cancer cell growth and survive. Given high cytokine production by HP infection, it is tempting to speculate that the infection enhances growth of gastric adenocarcinoma by NFκB activation through IL1R. An alternative hypothesis is that virulent factors from HP continue to transcriptionally activate NFκB in transformed cells. Further investigation of the functional consequences of HP infection will be needed to define its exact role in cancer development though some gastric cancers arise long after infection has disappeared because of unfavorable conditions for HP in the precancerous changes. Nevertheless, high IL1β production by HP infection remains of particular interest in the context of gastric cancer because it is the main cause of chronic gastritis.
In conclusion, this study showed that there was no association between IL1B−31 and FAS polymorphisms and the risk of gastric cancer among the Japanese population. The observed trend in which IL1B−31 TT genotype was more prevalent with the advanced stage of stomach cancer, although of interest, needs further clarification.
Abbreviations
- NFκB:
-
Nuclear factor of kappa B
- HP:
-
Helicobacter pylori
- PCR-CTPP:
-
Polymerase chain reaction with confronting two-pair primers
- HERPACC:
-
The Hospital-based Epidemiologic Research Program at Aichi Cancer Center
References
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Bonizzi G, Karin M (2004) The two NF-kappaB activation pathways and their role in innate and adaptive immunity. Trends Immunol 25:280–288
Chang YW, Jang JY, Kim NH, Lee JW, Lee HJ, Jung WW, Dong SH, Kim HJ, Kim BH, Lee JI, Chang R (2005) Interleukin-1B (IL-1B) polymorphisms and gastric mucosal levels of IL-1beta cytokine in Korean patients with gastric cancer. Int J Cancer 114:465–471
Clevers H (2004) At the crossroads of inflammation and cancer. Cell 118:671–674
Cordon-Cardo C, Prives C (1999) At the crossroads of inflammation and tumorigenesis. J Exp Med 190:1367–1370
El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, Herrera J, Lissowska J, Yuan CC, Rothman N, Lanyon G, Martin M, Fraumeni JF, Jr. Rabkin CS (2000) Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature 404:398–402
El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, Herrera J, Lissowska J, Yuan CC, Rothman N, Lanyon G, Martin M, Fraumeni JF, Jr. Rabkin CS (2001) The role of interleukin-1 polymorphisms in the pathogenesis of gastric cancer. Nature 412:499
El-Omar EM, Rabkin CS, Gammon MD, Vaughan TL, Risch HA, Schoenberg JB, Stanford JL, Mayne ST, Goedert J, Blot WJ, Fraumeni JF, Jr. Chow WH (2003) Increased risk of noncardia gastric cancer associated with proinflammatory cytokine gene polymorphisms. Gastroenterology 124:1193–1201
Engelmark MT, Renkema KY, Gyllensten UB (2004) No evidence of the involvement of the Fas−670 promoter polymorphism in cervical cancer in situ. Int J Cancer 112:1084–1085
Greten FR, Karin M (2004) The IKK/NF-kappaB activation pathway—a target for prevention and treatment of cancer. Cancer Lett 206:193–199
Group HC (2001) Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut 49:347–353
Hall SK, Perregaux DG, Gabel CA, Woodworth T, Durham LK, Huizinga TW, Breedveld FC, Seymour AB (2004) Correlation of polymorphic variation in the promoter region of the interleukin-1 beta gene with secretion of interleukin-1 beta protein. Arthritis Rheum 50:1976–1983
Hamajima N, Hirose K, Inoue M, Takezaki T, Kuroishi T, Tajima K (1995) Age-specific risk factors of breast cancer estimated by a case-control study in Japan. J Epidemiol 5:99–105
Hamajima N, Matsuo K, Saito T, Hirose K, Inoue M, Takezaki T, Kuroishi T, Tajima K (2001a) Gene–environment interactions and polymorphism studies of cancer risk in the hospital-based epidemiologic research program at Aichi Cancer Center II (HERPACC-II). Asian Pac J Cancer Prev 2:99–107
Hamajima N, Matsuo K, Saito T, Tajima K, Okuma K, Yamao K, Tominaga S (2001b) Interleukin 1 polymorphisms, lifestyle factors, and Helicobacter pylori infection. Jpn J Cancer Res 92:383–389
Huang QR, Morris D, Manolios N (1997) Identification and characterization of polymorphisms in the promoter region of the human Apo-1/Fas (CD95) gene. Mol Immunol 34:577–582
Hwang IR, Kodama T, Kikuchi S, Sakai K, Peterson LE, Graham DY, Yamaoka Y (2002) Effect of interleukin 1 polymorphisms on gastric mucosal interleukin 1beta production in Helicobacter pylori infection. Gastroenterology 123:1793–1803
Ikehara Y, Nishihara S, Kudo T, Hiraga T, Morozumi K, Hattori T, Narimatsu H (1998) The aberrant expression of Lewis a antigen in intestinal metaplastic cells of gastric mucosa is caused by augmentation of Lewis enzyme expression. Glycoconj J 15:799–807
Ikehara Y, Nishihara S, Yasutomi H, Kitamura T, Matsuo K, Shimizu N, Inada K, Kodera Y, Yamamura Y, Narimatsu H, Hamajima N, Tatematsu M (2001) Polymorphisms of two fucosyltransferase genes (Lewis and Secretor genes) involving type I Lewis antigens are associated with the presence of anti-Helicobacter pylori IgG antibody. Cancer Epidemiol Biomarkers Prev 10:971–977
Inoue M, Tajima K, Hirose K, Hamajima N, Takezaki T, Kuroishi T, Tominaga S (1997) Epidemiological features of first-visit outpatients in Japan: comparison with general population and variation by sex, age, and season. J Clin Epidemiol 50:69–77
Kanemitsu S, Ihara K, Saifddin A, Otsuka T, Takeuchi T, Nagayama J, Kuwano M, Hara T (2002) A functional polymorphism in fas (CD95/APO-1) gene promoter associated with systemic lupus erythematosus. J Rheumatol 29:1183–1188
Karin M, Cao Y, Greten FR, Li ZW (2002) NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer 2:301–310
Kimura R, Nishioka T, Soemantri A, Ishida T (2004) Cis-acting effect of the IL1B C−31T polymorphism on IL-1 beta mRNA expression. Genes Immun 5:572–575
Lai HC, Sytwu HK, Sun CA, Yu MH, Yu CP, Liu HS, Chang CC, Chu TY (2003) Single nucleotide polymorphism at Fas promoter is associated with cervical carcinogenesis. Int J Cancer 103:221–225
Lin A, Karin M (2003) NF-kappaB in cancer: a marked target. Semin Cancer Biol 13:107–114
Ma Y, Liu H, Tu-Rapp H, Thiesen HJ, Ibrahim SM, Cole SM, Pope RM (2004) Fas ligation on macrophages enhances IL-1R1-Toll-like receptor 4 signaling and promotes chronic inflammation. Nat Immunol 5:380–387
Machado JC, Figueiredo C, Canedo P, Pharoah P, Carvalho R, Nabais S, Castro Alves C, Campos ML, Van Doorn LJ, Caldas C, Seruca R, Carneiro F, Sobrinho-Simoes M (2003) A proinflammatory genetic profile increases the risk for chronic atrophic gastritis and gastric carcinoma. Gastroenterology 125:364–371
Osaki M, Kase S, Kodani I, Watanabe M, Adachi H, Ito H (2001) Expression of Fas and Fas ligand in human gastric adenomas and intestinal-type carcinomas: correlation with proliferation and apoptosis. Gastric Cancer 4:198–205
Palli D, Saieva C, Luzzi I, Masala G, Topa S, Sera F, Gemma S, Zanna I, D’Errico M, Zini E, Guidotti S, Valeri A, Fabbrucci P, Moretti R, Testai E, del Giudice G, Ottini L, Matullo G, Dogliotti E, Gomez-Miguel MJ (2005) Interleukin-1 gene polymorphisms and gastric cancer risk in a high-risk Italian population. Am J Gastroenterol 100:1941–1948
Peek RM Jr Blaser MJ (2002) Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer 2:28–37
Sasaki N, Morisaki T, Hashizume K, Yao T, Tsuneyoshi M, Noshiro H, Nakamura K, Yamanaka T, Uchiyama A, Tanaka M, Katano M (2001) Nuclear factor-kappaB p65 (RelA) transcription factor is constitutively activated in human gastric carcinoma tissue. Clin Cancer Res 7:4136–4142
Senftleben U, Karin M (2002) The IKK/NF-kappa B pathway. Crit Care Med 30:S18–S26
Sibley K, Rollinson S, Allan JM, Smith AG, Law GR, Roddam PL, Skibola CF, Smith MT, Morgan GJ (2003) Functional FAS promoter polymorphisms are associated with increased risk of acute myeloid leukemia. Cancer Res 63:4327–4330
Sicinschi LA, Lopez-Carrillo L, Camargo MC, Correa P, Sierra RA, Henry RR, Chen J, Zabaleta J, Piazuelo MB, Schneider BG (2006) Gastric cancer risk in a Mexican population: role of Helicobacter pylori CagA positive infection and polymorphisms in interleukin-1 and -10 genes. Int J Cancer 118:649–657
Sun T, Miao X, Zhang X, Tan W, Xiong P, Lin D (2004) Polymorphisms of death pathway genes FAS and FASL in esophageal squamous-cell carcinoma. J Natl Cancer Inst 96:1030–1036
Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, Taniyama K, Sasaki N, Schlemper RJ (2001) Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 345:784–789
Vollmers HP, Dammrich J, Hensel F, Ribbert H, Meyer-Bahlburg A, Ufken-Gaul T, von Korff M, Muller-Hermelink HK (1997) Differential expression of apoptosis receptors on diffuse and intestinal type stomach carcinoma. Cancer 79:433–440
Xuan J, Deguchi R, Watanabe S, Ozawa H, Urano T, Ogawa Y, Fukuda R, Kijima H, Koga Y, Takagi A (2005) Relationship between IL-1beta gene polymorphism and gastric mucosal IL-1beta levels in patients with Helicobacter pylori infection. J Gastroenterol 40:796–801
Yang J, Hu Z, Xu Y, Shen J, Niu J, Hu X, Guo J, Wei Q, Wang X, Shen H (2004) Interleukin-1B gene promoter variants are associated with an increased risk of gastric cancer in a Chinese population. Cancer Lett 215:191–198
Yoshimura K, Hanaoka T, Ohnami S, Kohno T, Liu Y, Yoshida T, Sakamoto H, Tsugane S (2003) Allele frequencies of single nucleotide polymorphisms (SNPs) in 40 candidate genes for gene-environment studies on cancer: data from population-based Japanese random samples. J Hum Genet 48:654–658
Zeng ZR, Hu PJ, Hu S, Pang RP, Chen MH, Ng M, Sung JJ (2003) Association of interleukin 1B gene polymorphism and gastric cancers in high and low prevalence regions in China. Gut 52:1684–1689
Acknowledgments
This work was supported in part by Grants-in-Aid for Scientific Research on Priority Area (10311440 to Y I and 12218242 K T) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikehara, S.K., Ikehara, Y., Matsuo, K. et al. A polymorphism of C-to-T substitution at −31 IL1B is associated with the risk of advanced gastric adenocarcinoma in a Japanese population. J Hum Genet 51, 927–933 (2006). https://doi.org/10.1007/s10038-006-0040-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-006-0040-2
Keywords
This article is cited by
-
Effects of the interleukin-1β-511 C/T gene polymorphism on the risk of gastric cancer in the context of the relationship between race and H. pylori infection: a meta-analysis of 20,000 subjects
Molecular Biology Reports (2015)
-
Significant association among the Fas -670 A/G (rs1800682) polymorphism and esophageal cancer, hepatocellular carcinoma, and prostate cancer susceptibility: a meta-analysis
Tumor Biology (2014)
-
Associations of three common polymorphisms in CD95 and CD95L promoter regions with gastric cancer risk
Tumor Biology (2013)