Abstract
β-Lactams are one of the most useful classes of antibiotics against many common bacterial pathogens. One exception is Mycobacterium tuberculosis. However, with increasing incidence of multidrug-resistant tuberculosis and a need for new agents to treat it, the use of β-lactams, specifically the combination of carbapenem and clavulanate, is now being revisited. With this attention, comes the need to better understand both the mechanisms of action of β-lactams against M. tuberculosis as well as possible mechanisms of resistance, within the context of what is known about the β-lactam action in other bacteria. M. tuberculosis has two major mechanisms of intrinsic resistance: a highly active β-lactamase and a poorly permeable outer membrane. Within the cell wall, β-lactams bind several enzymes with differing peptidoglycan-synthetic and -lytic functions. The inhibition of these enzymes may lead to cell death through several mechanisms, involving disruption of the balance of synthetic and lethal activities. Currently, all known means of resistance to the β-lactams rely on diminishing the proportion of peptidoglycan-synthetic proteins bound and inhibited by β-lactams, through either exclusion or destruction of the antibiotic, or through replacement or supplementation of target enzymes. In this review, we discuss possible mechanisms for β-lactam activity in M. tuberculosis and the means by which it may acquire resistance, within the context of what is known in other bacterial species.
Similar content being viewed by others
The need for β-lactams in tuberculosis treatment
Tuberculosis causes more than a million human deaths and US$50 billion of economic damage each year.1 The disease poses a continuing threat to public health because of the emergence of multidrug-resistant, extensively drug-resistant and, recently, totally drug-resistant strains of the causative organism, Mycobacterium tuberculosis (MTB).2
Standard tuberculosis treatment for drug-sensitive disease requires the simultaneous use of four drugs: rifampin, an RNA transcription inhibitor; isoniazid, a mycolic acid biosynthesis inhibitor; ethambutol, an arabinogalactan biosynthesis inhibitor; and pyrazinamide, which inhibits the recycling of stalled ribosomes.3 The side effects of the tuberculosis treatment regimen can be severe and may discourage many patients suffering tuberculosis from completing the course of treatment. Furthermore, the 6-month duration of the treatment makes ensuring its completion difficult in impoverished areas with poor public health systems. Yet this is necessary even in the best-case scenario of a fully drug-susceptible isolate; treating drug-resistant MTB requires even more complex and toxic therapies for longer durations.
Conspicuously absent from this list of drugs are many members of the antibiotic classes commonly used to treat respiratory tract infections: β-lactams, fluoroquinolones and macrolides.4 Fluoroquinolones are used in second-line therapy and are currently in phase III clinical trials as first-line agents.5 Macrolides have efficacy against other mycobacteria, but MTB has intrinsic resistance to this class of antibiotics. Other commonly used drug classes such as aminoglycosides (for example, streptomycin6) and more recently, oxazolidinones (linezolid7) may be used for resistant MTB as well. However, β-lactams have not been clinically exploited for therapy of MTB to date.
This absence is notable, because β-lactams are among the oldest and best-validated antibiotics in medical practice, a bactericidal class of antibiotics with well-characterized pharmacokinetic and pharmacodynamic properties. They are the preferred agents in a multitude of infections, both common and serious, caused by a diverse group of bacterial pathogens, including community-acquired pneumonia,8 health-care-associated pneumonia,9 endocarditis,10 bacteremia and sepsis,11 cellulitis and other skin/soft-tissue infections including necrotizing fasciitis,12 meningitis,13 prosthetic joint infections,14 intra-abdominal infections,15 otitis media,16 Lyme disease with neurologic or cardiac involvement,17 and sexually transmitted infections such as gonorrhea and syphilis.18 Microbes have acquired resistance in nearly all of these settings through diverse mechanisms that will be explored in this review, including inactivation through β-lactamases, mutation of the target protein in the cell wall, and expulsion from the periplasmic space. However, in part because of their tremendous efficacy against susceptible organisms, strategies have been developed to overcome some of these resistance mechanisms in other clinical settings. Modification of β-lactams to evade β-lactamase activity, concurrent therapy with β-lactamase inhibitors and optimization of β-lactams to target the penicillin-binding proteins (PBPs) of specific pathogens have all increased their antimicrobial breadth, allowing their use against certain organisms possessing β-lactamases or refractory PBPs.
MTB possesses a strong, constitutive β-lactamase activity19 that renders it highly resistant to β-lactams,20 and this is thought to be one important reason why this class was not initially successful in treating MTB.21 However, β-lactamase inhibitors that have been developed for other applications have activity against the MTB β-lactamase,22 and degradation-resistant β-lactam agents such as carbapenems have some efficacy as well.23 Recently, the rise of multidrug-resistant tuberculosis has encouraged renewed interest in β-lactam/β-lactamase inhibitor combination therapy. Despite the fact that amoxicillin/clavulanate, one such combination, saw only limited success in several trials,24, 25 a recent study has shown that meropenem/clavulanate has potent activity against drug-resistant MTB. This study also showed strong activity against anaerobic models of persistent MTB infection, which are hypothesized to bear similarity to non-replicating or dormant bacteria in persistent clinical conditions. Activity in these anaerobic models may indicate a potential to shorten MTB’s unusually long duration of therapy.26 Although meropenem must be administered i.v., this finding has led to a successful animal trial27 and preliminary clinical trials of meropenem/clavulanate against MDR/XDR-TB, resulting in significant improvements in outcomes for treated patients versus controls.28, 29 Such developments are especially encouraging because the β-lactams represent a path to cell death not targeted by existing therapies, and resistance to those therapies should minimally impact β-lactam treatment. These developments offer the promise of bringing one of our most historically successful drug classes to bear on one of the world’s most prolific pathogens.
The potential clinical use of meropenem/clavulanate and the search for new antitubercular compounds in general raise two questions. First, what existing defenses does MTB have against small molecules? Second, what are the means by which it may acquire further resistance? This review shall consider each of these questions in turn, primarily from the perspective of the β-lactams, of which meropenem and other carbapenems are a subclass, drawing from possible mechanisms described in other bacterial species. We shall consider existing defenses including the complex architecture of the cell wall, with special emphasis on the lytic transglycosylases of MTB, and review existing mechanisms of β-lactam resistance across bacteria, with an emphasis on the diversity of possible mechanisms applicable to MTB.
The mycobacterial cell envelope
The outer membrane
Two obstacles impede β-lactams in their passage through the cell wall to their transpeptidase targets in the MTB peptidoglycan. First, they must traverse the hydrophobic, poorly permeable mycolic acid layer that constitutes a major part of the cell wall.30 Then, they must escape the hydrolytic activity of MTB’s promiscuous, highly active β-lactamase.31 The latter obstacle need not cripple the possibility of β-lactam therapy, however, because some β-lactams like meropenem are inherently poor substrates for the MTB β-lactamase. Furthermore, the β-lactamase is efficiently inhibited by clavulanate in combination therapy.31 The β-lactamase on one side of the membrane combines with membrane permeability, an additional important parameter, to determine the concentration of β-lactam within the periplasmic space and accessibility to β-lactam targets in a non-equilibrium state.32
The MTB cell wall contains an outer layer of unique mycolic acids that are C60–C90 long chain carboxylic acids covalently linked to arabinogalactan, an underlying polymer of repeating sugars.33 This arabinogalactan layer is itself covalently bound to the peptidoglycan sacculus.34 Together, then, the mycolic acids, arabinogalactan and peptidoglycan compose one giant macromolecule encasing the cell proper (Figure 1).34
The mycobacterial cell envelope consists of the cell membrane (CM), a periplasmic space (PS) and several layers of peptidoglycan (PG), which is covalently bound to branching chains of furans in arabinogalactan (AG), themselves covalently bound to long-chain mycolic acids (MA). The outer layer of the cell envelope is a heterogeneous mixture of glycolipids (GL). The bars to the left of the labels indicate degree of hydrophilicity, with dark representing hydrophobicity and light representing hydrophilicity.
Several properties of the mycolic acids make them formidable obstacles to the passage of β-lactams and other small molecules. These include their size or length, their structure and their unusual modifications or unsaturations. The mycolic acids extend around 53–64 carbons from a primary carboxylic acid head group, with the remaining carbons forming a branch extending from the carboxylic acid α-carbon.35 This carbon length is substantially longer than the average fatty acid in MTB’s inner cell membrane (Figure 1). However, recent electron microscopy studies indicate that the hydrophobic region of the outer mycolic acid layer is not substantially thicker than the cell membrane, leaving some question as to the exact conformation of mycolic acids in their cellular context.36, 37 What is certain is that they are generally perpendicular to the surface of the cell, and their boundary with the hydrophilic extracellular milieu or capsular area is mediated by a variety of accessory lipids, such as phthiocerol dimycocerosate and the sulfolipids, and glycolipids, including lipomannan and lipoarabinomannan.38, 39 Together, the mycolic acids on the inner leaflet and the free glycolipids on the outer leaflet effectively form a mycobacterial outer membrane bilayer (Figure 1).36, 37
This outer membrane forms a substantial permeability barrier to both nutrients and antibiotics. For the cephalosporin class of β-lactams, by one estimate, the dual limitations of the permeability barrier and β-lactamase activity create a 500–5000-fold concentration differential between the extracellular milieu and the periplasm, compared to a 1.5–15-fold differential across the outer membrane of Escherichia coli.40 This is true regardless of the hydrophobicity of the cephalosporin.
Beyond the hydrophobicity of the mycolic acids, their unusual length and characteristic unsaturations of the alkyl chain also contribute to the permeability barrier. The different types of unsaturation, which may vary across species, likely contribute to the higher or lower permeability of the cell walls of different mycobacteria. For instance, MTB and Mycobacterium avium-intracellulare possess a combination of cis-cyclopropanations or cis-olefins that other mycobacterial species lack; in direct biophysical comparisons, this modification raised the melting temperature of tubercular mycolic acids by 3 °C relative to the mycolic acids of an isogenic strain lacking the ability to incorporate this unsaturation.41 In a survey across mycobacterial species, the melting temperature of mycolic acid membranes also rose in proportion to the average mycolic acid length for a given species.42 The increases in mycolic acid melting temperature from cyclopropanation and elongation reflect a decrease in fluidity, which is directly related to the ability of molecules to diffuse through the membrane.42 These measurements, then, provide a biophysical basis to understand the importance of MTB’s outer membrane as a permeability barrier.
The peptidoglycan
Beyond the outer membrane, β-lactams enjoy unhindered passage through the hydrophilic arabinogalactan to the peptidoglycan target area. The properties of the peptidoglycan, such as glycan chain length and the type and density of cross-linking, do not directly affect β-lactam susceptibility, though they are the product of the peptidoglycan-synthetic machinery that is the β-lactam target. Glycan chain length and the type and density of cross-linking may reflect the relative importance of individual components of the peptidoglycan-synthetic machinery and thus determine which ones are viable antibiotic targets.
Like E. coli and Bacillus subtilis, MTB peptidoglycan is of type A1γ, which consists of long glycan chains cross-linked by interlinked peptide stems of the sequence L-Ala-γ-D-Glu-meso-Dap-D-Ala-D-Ala. (Meso-Dap is meso-diaminopimelic acid and γ-D-Glu is glutamate polymerised from its γ-carboxylic acid group; Figure 243, 44). In MTB, the glutamate often forms isoglutamine through amidation of the free α-carboxylic acid. The most common variation on this scheme in MTB is the addition of a single glycine to the ɛ-amino group on meso-Dap,44 similar to the interpeptide bridges in many Gram-positive firmicutes.45
Peptidoglycan side chains in MTB contain L-alanine, D-isoglutamate, meso-diaminopimelic acid, D-alanine and D-alanine. The chirality of each stereocenter is indicated in bold. The possible reactive carbons to an invading nucleophile are indicated with electron-pushing arrows at Positions 3 and 4. D-isoglutamate in MTB is often amidated, as depicted.
The combinatorial diversity formed by the cross-linking of these side chains greatly exceeds the variations in the side chains themselves, mediated by a collection of transpeptidases. Previously, models assumed that these penicillin-binding transpeptidases carried out most or all of this cross-linking,46 and that these transpeptidases were the high MW (HMW) PBPs. Each HMW PBP contains a transpeptidase domain, which catalyzes the displacement of the peptide bond to the terminal D-Ala of a receiving pentapeptide side chain with the amino group from an invading peptide side chain (Figure 2). This amino group is always contributed by the amino acid at the Position 3 (Figure 2); in MTB, this is the ɛ-amino group of meso-Dap, but in other species, it may be the side chain amino group of lysine or ornithine instead.47
As with glycan chain length, the degree of peptide cross-linking modulates the properties of the peptidoglycan macromolecule. More cross-linking results in a finer mesh encircling the cell. The greater number of cross-links per unit area also means that individual cross-links may be less stressed, because each cross-link bears less of the turgor pressure of the cell contents. The diversity of PBP paralogs in most bacterial species suggests transcriptional or translational mechanisms may play a role in controlling the amount of cross-linking that occurs, but other mechanisms exist as well. For example, carboxypeptidases can remove the terminal D-Ala from a side chain, preventing it from accepting a cross-link from a neighboring peptide strand. Endopeptidases also can hydrolyze existing peptide cross-links, most often at Position 4 (Figure 2), but endopeptidases have been described that cleave at nearly every position.48 In contrast to Position 4 endopeptidases, which are generally non-essential, the endopeptidase cleaving at Position 2 in MTB is essential.49
Beyond the degree of cross-linking, the nature of the cross-link also appears to have a major impact on bacterial physiology. Although the invading amine group is always a side chain from Position 3, the receiving carboxylic acid can be at Position 4 or Position 3 (Figure 2). The former cross-link, termed a 4→3 cross-link, predominates in E. coli.43 The D,D stereochemistry of the invading and receiving amino acid chiral centers matches the stereochemistry of the D-Ala-D-Ala bond they replace; these bonds are the natural substrates of PBPs.50 In contrast, the 3→3 cross-link, which is formed by an invading amine group from Position 3 forming a covalent bond with the α-carboxylic acid of Position 3 meso-Dap, predominates in Mycobacterium abscessus51 and stationary phase MTB.44 The L,D stereochemistry of the disrupted link between meso-Dap and D-Ala has given the enzymes catalyzing the formation of 3→3 cross-links the name of L,D-transpeptidases. The investigation of 3→3 cross-links is relatively new, but it is clear that they play a major role in determining β-lactam susceptibility.52
This unusual cross-linking is just one of several properties, then, that contribute to the complexity of the mycobacterial cell envelope as a β-lactam obstacle. It combines with the low permeability of the mycolic acid layer and the mycobacterial β-lactamase to present an array of difficulties that β-lactam chemotherapy must overcome.
The β-lactam mechanism of action
The molecular targets of the β-lactams
The β-lactams were the first antibiotics discovered, and have to date been among the most successful, both in use and diversity, having spawned hundreds of semi-synthetic derivatives.53 Exposure to β-lactams may induce several different effects. The observable outcomes range from bacteriostasis and morphological alterations to rapid bacteriolysis.54 Although effects vary for particular species,55 antibiotics54 and exposure conditions,56 all known effects result from the inhibition of peptidoglycan-modifying peptidases outside of the cell membrane. These peptidases are the (D,D-) PBPs and the L,D-transpeptidases.57
The most important effects of exposure to β-lactams are cell death and bacteriolysis. Current models hold that cell death arises only from the inhibition of peptidoglycan-synthesizing HMW PBPs and L,D-transpeptidases,58 and not the low MW endo- and carboxypeptidase PBPs, which hydrolyze peptidoglycan (Table 1). Although the phenotypic alterations arising from deletion of the low MW PBPs indicate that they may be responsible for some of the morphological effects of β-lactam treatment, they are not usually essential for viability.59
For the two most diverse classes of β-lactams, the penicillins and cephalosporins, bacteriolysis and cell death probably occur through inhibition of the HMW PBPs alone and not the L,D-transpeptidases.54, 57 Although cephalosporin binding to the L,D-transpeptidases can occur,60 the failure to identify these proteins in most early assays for β-lactam binding proteins suggests the phenomenon is not common.
The third major class of β-lactams, the carbapenems, also display high affinity for certain Class A HMW PBPs,61 and so it had been assumed that the carbapenems target these PBPs too.62 Recently, however, the finding that carbapenems form adducts with the L,D-transpeptidases that form 3→3 cross-links in MTB,63 and that they potently kill organisms rich in these cross-links,26 has raised the possibility that these enzymes may in fact be an additional or alternate molecular target for the carbapenems.58
Whatever the relevant protein targets are in the cell, the β-lactams mimic the natural D-Ala-D-Ala substrate of the PBPs and inhibit them by forming a slowly hydrolyzing adduct at the active site. The hypothesis that carbapenems may target the L,D-transpeptidases has force because a distinctive feature of the carbapenems versus other β-lactams is the opposite chirality of the α-carbon, which mirrors the fourth position of the peptide substrate (Figure 3).62, 64 The chirality difference between other β-lactams and carbapenems thus corresponds to the difference between D,D- and L,D-transpeptidation.
Molecular pathways to cell death
Although a range of HMW PBPs and L,D-transpeptidases have been identified as binding targets, the means by which the inhibition of these targets leads to the observed effects of β-lactam exposure is less clear. In fact, the precise mechanism by which β-lactams kill bacteria is an enduring mystery.57, 65, 66, 67 The functional diversification of PBPs complicates efforts to solve the mystery, as has the multiplicity of PBP paralogs in the typical bacterial genome and the variable death mechanisms, requirements and phenotypes observed in different bacterial species. Although all of these paralogs can be easily identified in MTB bioinformatically, their genetic study is only just beginning, and so we shall draw upon the body of work on more tractable organisms to describe how the inhibition of the molecular targets of β-lactams may lead to killing.
In E. coli, the phenotypic effects of exposure to several β-lactams have received the most comprehensive study. Some β-lactams, such as cephalexin, specifically inhibit PBP3 leading to filamentation. Others, such as mecillinam, specifically inhibit PBP2, the function of which is less clear, inducing the formation of ovoid cells. β-Lactams such as benzylpenicillin specifically inhibit the collective PBP1, leading to rapid lysis.54 The collective PBP1 comprises all of the E. coli Class A PBPs, including PBP1a, PBP1b and PBP1c, which were not separable in initial observations of the E. coli PBP complement.
The bacteriolytic effect of PBP1 inhibition is consistent with a number of data indicating that the Class A HMW PBPs are collectively essential in many species. This has been genetically demonstrated in E. coli68 and B. subtilis.69 In Corynebacterium glutamicum, a close relative of MTB with a one-to-one corresponding set of PBPs, the deletion of the full complement of Class A HMW PBPs leads to severe morphological defects.70 Why precisely these phenotypes should arise is not clear; both the glycosyltransferase and transpeptidase activities of the Class A HMW PBPs are biochemically redundant with monofunctional glycosyltransferases and Class B PBPs that are expressed in the bacterium, respectively. One hypothesis is that some Class A HMW PBPs may serve an essential scaffolding function, which cannot be fulfilled by alternative peptidoglycan-synthesizing enzymes,71 though whether β-lactam binding would disrupt such a function bears further investigation.
The effects of PBP3 inhibition are also consistent across species. PBP3, also called FtsI, has a more distinct and well-defined spatiotemporal role than other PBPs, as a catalyst of cross-linking during septal peptidoglycan synthesis. It is recognizable across species and essential for septation and viability in E. coli, B. subtilis and C. glutamicum.72, 73, 74, 75 The filamentation phenotype upon exposure to cephalexin is therefore consistent with this known function.
The most extreme of these effects of PBP inhibition, cell death, is perforce the one of most interest, but it is also the most complicated. Several models have been proposed over the years, most of them following directly from effects on the cell wall, but others including transcriptional effects and wholesale macromolecular damage. Although little is known about how these models apply to MTB, it is likely β-lactams use some subset of the death pathways present in other bacteria.
Killing by autolysis
When β-lactams were first discovered, the simplest model for killing was that cell death at bactericidal concentrations ultimately arises from the inhibition of the well-conserved and essential functions of either FtsI or the collective Class A HMW PBPs.54 The inhibition of either of these cross-linking functions could result in a cell wall with weakened mechanical stability, which would ultimately succumb to the turgor pressure within the cell, rupturing violently.76, 77 Although inhibition of cross-linking and concomitant loss of mechanical stability certainly occur upon β-lactam exposure, findings from many laboratories have since shown that the links between these effects and ultimate cell death are potentially much more complicated than initially thought.
One of the first observations to hint at the underlying complexity of the effects of β-lactams on viability occurred in Streptococcus pneumoniae. S. pneumoniae has an autolytic system that causes it to undergo massive loss of viability upon reaching stationary phase.78 Inhibition of LytA, a peptidoglycan amidase that functions as an autolysin in stationary phase, by the substitution of ethanolamine for choline in the cell wall conferred tolerance to penicillin.79 Genetic inactivation of amidases in E. coli80 and endopeptidases in B. subtilis81 confirmed that such autolysins are widely required for β-lactam-mediated bacteriolysis. All of these proposed autolysins are in fact peptidoglycan-modifying enzymes with functions presumed to be related to the reshaping and division of the peptidoglycan sacculus during growth.48 Notably, in all of these species, β-lactam tolerance is not complete; bacteriostatic, but not bacteriolytic, effects still occur, and in some cases there is still a gradual loss of viability in the presence of β-lactams.78, 81, 82 These observations imply that either additional autolysins or another pathway of cell death must exist.
The requirement for autolysins has led to the balanced growth model of killing by β-lactams.83 In this model, the proper maintenance of peptidoglycan requires a balance of synthetic activities, primarily from PBPs, and lytic activities from autolytic peptidoglycan hydrolases, such as the amidase LytA. Inhibition of synthetic HMW PBPs by β-lactams tips the balance in favor of the lytic activities, and the cell wall gradually degrades until it is too weak to withstand the turgor pressure of the cell, resulting in release of cytoplasmic contents and death.83 MTB has many peptidoglycan hydrolytic activities that have not yet been fully characterized but that could be involved in balanced growth; further, only a few have been evaluated for their roles in antibiotic resistance.84, 85
Killing by induced autolysis
This model of death by autolysis has endured to the present as a partial explanation of β-lactam killing.86 The most significant refinement to this model has been the realization that autolysins are tightly regulated and dependent on cellular signals to enact β-lactam-mediated bacteriolysis.83 This refinement arose from the observation that in E. coli, B. subtilis, S. pneumoniae, S. aureus and Enterococcus faecium, manipulation of culture conditions could uncouple PBP inhibition and bacteriolysis in time: incubation of bacteria with β-lactams at acidic pH did not lead to lysis, but subsequent transfer of the same bacteria to neutral pH without β-lactams did lead to lysis.87, 88 This experiment demonstrates that neutral pH conditions either themselves activate autolysins or stimulate some signal that does so.
For firmicutes, an elegant model exists wherein the local acidity of cell wall regions controls hydrolase activity.89 Several factors in turn modulate this local acidity, including the buffering capacity and pH of the extracellular milieu, the proton motive force, and the D-alanylation of cell wall teichoic acids. The balance of these forces can cause fine-tuned local variations across the cell wall.89 This model is more problematic for proteobacteria such as E. coli, which lack teichoic acids and the thick peptidoglycan of firmicutes, which are critical features of the model.89 MTB lacks teichoic acids but possesses other negatively charged peptidoglycan-associated sugar polymers that could play a similar role.
Killing by holins
The balanced growth model does not explain cell death that occurs without bacteriolysis, which occurs in some streptococci.90, 91 In these systems, loss of colony-forming ability and protein and RNA synthesis occur without any detectable change in OD. In the initial report of this phenomenon, an uncharacterized mutation reduced this cell death by four orders of magnitude.91
The identity of this mutation did not become clear until years later, when other researchers found a mutation in the cidAB operon of S. aureus, which corresponds to the mutant streptococcus allele, that confers a similar amount of β-lactam resistance. It is also homologous to some holin proteins, which are small, amphiphilic helical proteins that tend to disrupt the membrane. Its deletion lowered the extracellular peptidoglycan hydrolase activity of Staphylococcus aureus mutants.92
Holins were first described in phage biology. During phage infection, peptidoglycan hydrolases remain intracellular, where they cannot act, until the appropriate point in the infection cycle. At the appropriate point, the balance of holins and antiholins changes to permeabilize the cell membrane; the released hydrolases digest the peptidoglycan, and the packaged phage can diffuse freely through the permeabilized membrane and digested peptidoglycan to infect other cells.93
Notably, although endogenous holins are hypothesized to perform the same biophysical function in S. aureus—permeabilization of the cell membrane—during β-lactam-induced death as phage-encoded holins do during phage escape, the method of killing to which endogenous holins contribute is non-lytic, indicating that it does not require the release of peptidoglycan hydrolases. Instead, cell death may occur simply as a result of the collapse of the cell membrane permeability barrier, followed by loss of the proton motive force and dissipation of the cellular machinery.89, 92 Consistent with this model, the antiholin regulator of cidAB, lrgAB, is activated in response to decreases in the proton motive force, allowing it to prevent inappropriate killing by cidAB-mediated permeabilization.94
Homologs of cidAB occur in E. coli and many Gram-positive bacteria, but there are no obvious homologs in MTB or other actinomycetes. This is not surprising, because the prevailing explanation for the existence of cidAB is that it has a role in biofilm development;89 the holins facilitate the release of DNA from dying staphylococci, which increases biofilm integrity.95 The exploration of biofilm roles in MTB pathogenesis is debated, but biofilms do not play a role in the classical model of granulomatous infection.96 Although MTB lacks obvious cidAB homologs, the possibility that some holin may contribute to β-lactam-mediated cell death cannot be excluded, because the holins are merely small, amphiphilic helical proteins, and proteins meeting this description are abundant in MTB’s genome.84
Killing by oxidative damage
Another proposal that is currently being debated is that killing by β-lactams (and other bactericidal antibiotics) may occur through the disregulation of the tricarboxylic acid cycle and the Fenton reaction, leading to an increase in cellular hydroxyl radicals.97 Although recent work has begun to elucidate the pathways by which hydroxyl radicals may lead to cell death,98 other work has shown that bactericidal antibiotics retain potency under conditions where hydroxyl radicals cannot be efficiently generated, indicating that the hydroxyl radical pathway may not be the only or even the major pathway to cell death for some antibiotic classes.99, 100 In MTB, hydroxyl radicals do seem to play a role in cellular death, at least under conditions of bacterial persistence.101
The very existence of tricarboxylic acid cycle disregulation under exposure to β-lactams reinforces a crucial point: the existence of pathways to cell death requires the sensing of either the β-lactams or the effect they have on their molecular targets.
Cellular sensing of β-lactams
The induced autolysis pathway, the holin:antiholin pathway and the oxidative damage pathway to bacterial cell death all require some means by which the cell can sense the state of its peptidoglycan, or sense the presence of β-lactams directly. Without signal transduction, the active processes in these pathways would never be initiated.
There are several possible mechanisms the MTB cell could use to monitor the state of its peptidoglycan-synthetic machinery. One mechanism is through a sensor protein. Methicillin-resistant S. aureus uses such a mechanism, via the BlaR1 protein, to monitor β-lactam concentrations so that it can avoid unnecessary expression of its supplementary, highly β-lactam-resistant PBP, PBP2a. PBP2a is the principal effector of methicillin resistance in methicillin-resistant S. aureus infection. BlaR1 consists of an extracellular sensor domain, resembling a transpeptidase domain, connected by a transmembrane helix to an internal peptidase response domain. In response to treatment with methicillin, BlaR1 upregulates the expression of PBP2a.102 MTB has a close homolog of BlaR1. This gene, Rv1845c, is thought to respond to β-lactams; however, it has only a BlaR1-like response domain, with no sensor domain.103 MTB nonetheless possesses many candidate domains that may bind to β-lactams that could serve as the sensor domain, including a number of β-lactamases and uncharacterized transpeptidases not thought to contribute directly to β-lactamase activity. It also possesses two genes that encode the PBP-associated serine and threonine kinase-associated domain, a specialized domain that may bind peptidoglycan-like substrates and play a role in sensing.104 It is possible that any of these proteins may interact with Rv1845c or another transmembrane regulator to convey direct information about the presence of β-lactams.
Another mechanism through which MTB may sense the presence of β-lactams is indirectly, by monitoring the state of its peptidoglycan. One way to do this would be through a peptidoglycan recycling pathway, by which various peptidoglycan fragments are transported directly to the cytosol. In E. coli, this pathway provides information through the proportion of tri-, tetra- and pentapeptides imported by AmpD, a disaccharide-peptide transporter. An increased ratio of pentapeptides to tripeptides indicates a lack of PBP activity, implying the presence of β-lactams and leading to expression of the AmpC β-lactamase.105 Although MTB does not possess clear homologs to the proteins of the Amp pathway, it and other Gram-positive bacteria have evidence of a peptidoglycan recycling system. Investigation of the Gram-positive system has elucidated several components that could be involved in peptidoglycan digestion, recovery and sensing, including the β-N-acetylglucosaminidase NagZ in B. subtilis,106 with MTB possessing a NagZ ortholog.84
Finally, bacteria may possess additional ways of sensing β-lactams by somehow directly monitoring the activity or inhibition of their β-lactam-sensitive transpeptidases. In C. glutamicum, which is closely related to MTB, depletion of FtsI (a Class B HMW PBP), but not its inhibition by cephalexin, results in overexpression of the structural protein DivIVA.75 The overexpression of this protein implies that cephalexin-bound FtsI activates some signaling pathway distinct from the one activated by absence of FtsI activity, which does not lead to DivIVA overexpression. As FtsI activity is absent in both cases, there should be no difference that can be detected from the state of the peptidoglycan itself. C. glutamicum, which falls in the same actinomycete family as MTB, may possess a sensor molecule like BlaR1 or may have some entirely novel way of monitoring FtsI activity.105
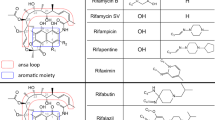
Potential defenses: β-lactam resistance across bacteria and its implications for mycobacteria
Given the uncertainty surrounding the precise series of steps by which exposure to β-lactams leads to bacterial cell death, it would be remarkable if there existed a complete catalog of the mechanisms by which bacteria might acquire resistance to the β-lactams. Nonetheless, two broad classes of resistance mechanisms have occurred over and over again. The first broad class contains those mechanisms that decrease the effective concentration of β-lactams at the general site of action, the periplasm or cell wall zone. This class comprises changes in outer membrane permeability, changes in β-lactamase activity and changes in efflux pump activity. The second broad class of β-lactam resistance mechanisms is the modification of the PBP profile of the cell in such a way that sufficient transpeptidase activity remains to permit survival even in the presence of the β-lactam. This may occur through target site modification in which an individual PBP acquires a mutation altering its affinity for the β-lactams, or through acquisition or activation of previously unused PBPs with low β-lactam affinity (Figure 4).
Overview of β-lactam resistance mechanisms. A simplified mycobacterial cell wall is depicted from the outer membrane (OM) through the peptidoglycan (PG) to the cell membrane (CM). In the bottom panel, the same cell wall is depicted after having utilized the full complement of resistance mechanisms discussed here: [1] alterations in permeability of the outer membrane; [2] increase in efflux pump expression; [3] increase in β-lactamase expression; [4] target site modification of the constitutive PBP [5] and expression of a new, β-lactam-refractory PBP.
Permeability
Changes in β-lactam cell entry could occur through alteration in their ability to diffuse through the hydrophobic bilayer itself or through alterations in the population of porins within the outer membrane.107 In Pseudomonas aeruginosa, which like MTB has a combination of permeability and efflux defenses,108 β-lactam diffusion through porins is a much more important means of access to the periplasm than direct diffusion across the lipid bilayer. This was inferred from the fact that increasing β-lactam hydrophobicity leads to decreasing β-lactam effectiveness, implying that the increased bilayer diffusion gained through increased hydrophobicity does not compensate for loss of mobility through porins. Supporting this line of argument, although both alterations in porin content109 and outer membrane composition110 correlate with acquisition of β-lactam resistance, the main explanation for differences in intrinsic resistance across genetic variants of P. aeruginosa is through the populations of porins that are permitted in the outer membrane.107, 110 Clinically significant drug resistance may arise from the accumulation of mutations modulating intrinsic resistance.111
Although the MTB cell wall is in some ways more similar to that of Gram-positive bacteria, MTB is similar to Gram-negative organisms in that it possesses a well-defined outer membrane with porins for nutrient diffusion. Also like Gram-negative bacteria, diffusion of β-lactams into MTB probably occurs through hydrophilic pathways rather than across its lipid bilayer.40 As few model Gram-positive organisms possess similar outer membranes to MTB, and against these few, β-lactams are generally ineffective, little literature exists on the possibility of MTB modifying its porin or outer membrane characteristics to resist β-lactam diffusion through its hydrophilic entry points. Nevertheless, expression of a porin from a closely related organism, Mycobacterium smegmatis, in the MTB model Mycobacterium bovis BCG, increased growth rate and sensitivity to several antibiotics, implying that low hydrophilic diffusion is a limiting factor in growth.112, 113 Thus, alterations in porins that result in increased β-lactam resistance are likely to also deleteriously affect growth.
Some research has identified loss of function mutations in sulfolipid biogenesis genes that appear to confer β-lactam resistance in MTB. Sulfolipids are components of the outer membrane. This work, however, only showed genetic association, and did not identify changes in the sulfolipid population or show a causal link between gene loss and resistance;114 nonetheless, the possibility exists that diffusion across the lipidic components of the outer membrane does play an unappreciated role in β-lactam access to the periplasm. The great complexity of the MTB outer membrane, discussed above, implies considerable evolutionary flexibility in the precise degree of membrane permeability possessed by the organism.
β-lactamase activity
The second method of altering effective β-lactam concentration is through enhancement or alteration of the β-lactamase profile. The development of β-lactamase inhibitors such as clavulanate or sulbactam that are co-administered with β-lactams, or the development β-lactams such as the carbapenems, which are resistant to most conventional β-lactamases, has largely, though not wholly, served to circumvent this resistance mechanism. However, MTB possesses a strong, promiscuous β-lactamase, BlaC,115 which is unusual in its ability to hydrolyze the carbapenem family, thus necessitating carbapenem administration with β-lactamase inhibitors.31 Beyond BlaC, MTB also possesses numerous apparent β-lactamase paralogs84 with undefined activity or regulation; not all are necessarily β-lactamases. The blaC gene itself is under control of at least two stress-responsive transcription factors.103 Together, these factors suggest a broad potential for MTB to alter its existing β-lactamase transcription levels and substrate specificities through spontaneous mutation. MTB has not yet realized this potential in the clinic; a broad survey of clinical strains found little variation in the β-lactamase activities present.116 This is perhaps unsurprising, because MTB has not experienced direct selective pressure from β-lactams during the chemotherapeutic era. Indeed, the presence of these β-lactamase paralogs present a possible reservoir from which resistance may emerge if β-lactam therapy is used against MTB in the future. It is an open question whether these additional β-lactamases too are inhibited by co-administration of β-lactamase inhibitors like clavulanate.117 Only BlaC has been extensively characterized.31
Current β-lactamase inhibitors are poorly effective against the metallo-β-lactamases, one of the most important resistance determinants for the carbapenems.118 However, MTB does not have nor is MTB likely to acquire one of these genes, because it has very low potential for horizontal gene transfer.119, 120
Multidrug efflux pumps
The third method of altering effective β-lactam concentration is through multidrug efflux pumps. Multidrug efflux pumps are a widespread mechanism of antibiotic resistance. In the case of MTB and other organisms possessing an outer membrane, all of the multidrug efflux pump families require adaptor proteins to facilitate transport from the cytoplasm or periplasm across the outer membrane. Although MTB does not possess homologs to the known adaptor proteins, it does possess numerous multidrug efflux pumps.114 One of these, Rv0194, exports β-lactams, and its loss confers β-lactam sensitivity.114 Therefore, it seems probable that adaptor proteins compatible with the unique mycobacterial cell envelope exist in the genome, but have not been discovered by standard bioinformatic approaches.
Target site modification
The second broad class of mechanisms of β-lactam resistance is modifications of the transpeptidase activity that allow it to evade β-lactam binding. The most prominent method for doing this is through target site modification, which can make a PBP more refractory to a given β-lactam. Target site modification may work through two methods. First, point mutations in the target site may alter the deacylation rate, allowing the PBP to eject the suicide substrate and regain its functionality on a shorter timescale. Such mutations confer modest resistance in S. pneumoniae.121 Second, point mutations can alter the affinity of the β-lactam for the particular PBP, thus favoring peptidoglycan substrate over β-lactam binding.57 Although target site modification often occurs through genetic exchange and the formation of mosaic alleles differing by as much as 15% from the original parent alleles,122 target site modification in MTB would occur through individual point mutations rather than genetic exchange, because of its low potential for horizontal gene transfer. Such mutations have been identified and described, conferring modest resistance to β-lactams in a phenotypically dominant manner.57, 123
Alteration of the penicillin-binding protein profile
Instead of altering an existing transpeptidase through target site modification, the cell can alternatively acquire or express a new PBP with low β-lactam affinity. The most prominent example of this sort of resistance is PBP2a in S. aureus. PBP2a has very low affinity for many β-lactams,124 but is sufficient to carry on transpeptidation when all other PBP transpeptidase functions are inhibited.125 PBP2a is induced by a β-lactam-sensing system,102 and its expression does not alter the remainder of the PBP profile of the cell,126 which is intuitively consistent with its dominant mode of action.123
S. aureus acquired PBP2a from a mobile genetic element;127 the possibilities for MTB acquiring PBP2a or a similar resistance mechanism are therefore limited by MTB’s low potential for horizontal gene transfer. Nonetheless, the fact that PBP2a is repressed under normal conditions illustrates an important point: MTB may not express its entire complement of PBPs under normal conditions, but upon the introduction of stress such as β-lactam exposure, it may upregulate expression of alternative PBPs with lower affinity for β-lactams. Some have hypothesized that ponA2, a Class A HMW PBP, may have special sterically obstructive elements that render it refractory to β-lactam binding and thus inhibition.50 Experimentally, the PBP PonA2 appears to have low affinity for some β-lactams,128 and our laboratory has noted that PonA2 seems to be poorly expressed at the protein level under standard growth conditions (unpublished data). Perhaps this is because it is not part of the housekeeping peptidoglycan biosynthesis machinery under such conditions. PonA2 is therefore a speculative example of the potential for a PBP2a-like resistance mechanism in MTB.
A relatively unexplored mechanism of resistance that fits broadly into alteration of the PBP profile is the replacement of normal cross-linking functions with L,D-transpeptidation in E. faecium. Inhibited by β-lactams, PBP cross-linking stops, whereas L,D-transpeptidation continues, resulting in a viable bacterium, albeit with an altered cell wall. In order for this alternative transpeptidation to occur in E. faecium, a β-lactam-insensitive D,D-carboxypeptidase is required to convert the usual pentapeptide substrate to a tetrapeptide, which is the substrate preference of the E. faecium transpeptidase.52, 129 Although MTB does not possess any orthologs of the E. faecium carboxypeptidase that prepares the substrate,84 it does possess several L,D-transpeptidases that could theoretically accept the usual pentapeptide substrates; thus, it is conceivable that MTB could acquire β-lactam resistance (with the exception of carbapenems that also inhibit L,D-transpeptidases) by using an alternative L,D-transpeptidation strategy to cross-link its cell wall. Crucially, evidence that L,D-transpeptidase activity may contribute to intrinsic resistance has been provided by a recent study showing that MTB lacking an L,D-transpeptidase is hypersensitized to amoxicillin.130 Nonetheless, it seems unlikely that any resistance provided by L,D-transpeptidase could be effective against carbapenems, because these bind both the L,D-transpeptidases and the D,D-carboxypeptidases in MTB that may hydrolyze pentapeptides prior to L,D-transpeptidation.131
Notably, this β-lactam resistance mechanism in E. faecium is distinctive from all other proposed resistance mechanisms in that it relies on loss of PBP function, and loss of dependence on this function, rather than gain or preservation of function in the face of increasingly harsh exposures to β-lactams.129 As there are many more ways for mutation to cause loss of function than gain of function, this mechanism of β-lactam resistance may be a long-term possibility for MTB.
Conclusion
MTB presents many challenges to β-lactam treatment. Some, like the degree of outer membrane impermeability it possesses, are less common among bacterial species, whereas others, like its strong β-lactamase, are familiar. The depth of the clinical problem posed by MTB, particularly strains that have acquired resistance to most or all first-line clinical agents, and the power of β-lactams against other infectious diseases urges a reconsideration by the preclinical community of the problem of how to potentiate this class of antibiotics in treatment. Unlike most common bacterial pathogens, as MTB has little chance of acquisition of foreign resistance elements as a means to dramatically increase its resistance to β-lactams, understanding the mechanisms of resistance that are accessible through mutation of its own genome will be paramount to any successful deployment and subsequent preservation of β-lactams against tuberculosis. Much has been learned about the mechanisms of β-lactam-mediated killing and β-lactam resistance over the years in many different bacterial species. Future investigations specifically focused on understanding these mechanisms in MTB will clarify and assist the effort to revisit their application to tuberculosis.
References
Laxminarayan, R. et al. Economic benefit of tuberculosis control. World Bank Policy Research Working Paper 4295, 44 (2007).
Udwadia, Z. F., Amale, R. A., Ajbani, K. K. & Rodrigues, C. Totally drug-resistant tuberculosis in India. Clin. Infect. Dis. 54, 579–581 (2012).
Shi, W. et al. Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. Science 333, 1630–1632 (2011).
Kiffer, C. R. & Pignatari, A. C. Pharmacodynamic evaluation of commonly prescribed oral antibiotics against respiratory bacterial pathogens. BMC. Infect. Dis. 11, 286 (2011).
Grosset, J. H., Singer, T. G. & Bishai, W. R. New drugs for the treatment of tuberculosis: hope and reality. Int. J. Tuberc. Lung. Dis. 16, 105–1014 (2012).
Streptomycin treatment of pulmonary tuberculosis. Br. Med. J. 2, 769–782 (1948).
Lee, M. et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N. Engl. J. Med. 367, 1508–1518 (2012).
Mandell, L. A. et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 44 (Suppl 2), S27–S72 (2007).
American Thoracic Society Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care. Med. 171, 388–416 (2005).
Baddour, L. M. et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111, e394–e434 (2005).
Dellinger, R. P. et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit. Care. Med. 41, 580–637 (2013).
Stevens, D. L. et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin. Infect. Dis. 41, 1373–1406 (2005).
Tunkel, A. R. et al. Practice guidelines for the management of bacterial meningitis. Clin. Infect. Dis. 39, 1267–1284 (2004).
Osmon, D. R. et al. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the infectious diseases society of America. Clin. Infect. Dis. 56, 1–10 (2013).
Solomkin, J. S. et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 50, 133–164 (2010).
Lieberthal, A. S. et al. The diagnosis and management of acute otitis media. Pediatrics 131, e964–e999 (2013).
Wormser, G. P. et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 43, 1089–1134 (2006).
Workowski, K. A. & Berman, S. Sexually transmitted diseases treatment guidelines, 2010. MMWR. Recomm. Rep. 59, 1–110 (2010).
Kasik, J. E. The nature of the mycobacterial penicillinase. Am. Rev. Respir. Dis. 91, 117–119 (1965).
Flores, A. R., Parsons, L. M. & Pavelka, M. S. Jr. Genetic analysis of the β-lactamases of Mycobacterium tuberculosis and Mycobacterium smegmatis and susceptibility to β-lactam antibiotics. Microbiology 151, 521–532 (2005).
Finch, R. Beta-lactam antibiotics and mycobacteria. J. Antimicrob. Chemother. 18, 6–8 (1986).
Chaves, J. et al. Can penicillins and other beta-lactam antibiotics be used to treat tuberculosis? Antimicrob. Agents Chemother. 39, 2620–2624 (1995).
Chaves, J., Turner, J., Schwarz, H., Kawamura, M. & Hopewell, P. C. Imipenem for treatment of tuberculosis in mice and humans. Antimicrob. Agents Chemother. 49, 2816–2821 (2005).
Chambers, H. F., Kogacoz, T., Sipit, T., Turner, J. & Hopewell, P. C. Activity of amoxicillin/clavulanate in patients with tuberculosis. Clin. Infect. Dis. 26, 874–877 (1998).
Donald, P. R. Early bactericidal activity of amoxicillin in combination with clavulanic acid in patients with sputum smear-positive pulmonary tuberculosis. Scand. J. Infect. Dis. 33, 466–469 (2001).
Hugonnet, J.-E., Tremblay, L. W., Boshoff, H. I., Barry, R. C. E. & Blanchard, J. S. Meropenem-clavulanate is effective against extensively drug-resistant Mycobacterium tuberculosis. Science 323, 1215–1218 (2009).
England, K. et al. Meropenem-clavulanic acid shows activity against Mycobacterium tuberculosis in vivo. Antimicrob. Agents Chemother. 56, 3384–3387 (2012).
Payen, M. C. et al. Clinical use of the meropenem-clavulanate combination for extensively drug-resistant tuberculosis [case study]. Int. J. Tuberc. Lung Dis. 16, 558–560 (2012).
De Lorenzo, S. et al. Efficacy and safety of meropenem-clavulanate added to linezolid-containing regimens in the treatment of MDR-/XDR-TB. Eur. Respir. J. 41, 1386–1392 (2013).
Brennan, P. J. & Nikaido, H. The envelope of mycobacteria. Annu. Rev. Biochem. 64, 29–63 (1995).
Hugonnet, J.-E. & Blanchard, J. S. Irreversible inhibition of the Mycobacterium tuberculosis beta-lactamase by clavulanate. Biochemistry 46, 11998–12004 (2007).
Zimmermann, W. & Rosselet, A. Function of the outer membrane of Escherichia coli as a permeability barrier to beta-lactam antibiotics. Antimicrob. Agents Chemother. 12, 368–372 (1977).
Azuma, I. & Yamamura, Y. Studies on the firmly bound lipids of human tubercle bacillus. J. Biochem. 53, 275–281 (1963).
Daffe, M., Brennan, P. J. & McNeil, M. Predominant structural features of the cell wall arabinogalactan of Mycobacterium tuberculosis as revealed through characterization of oligoglycosyl alditol fragments by gas chromatography/mass spectrometry and by 1H and 13C NMR analyses. J. Biol. Chem. 265, 6734–6743 (1990).
Asselineau, J. & Lederer, E. Structure of the mycolic acids of mycobacteria. Nature 166, 782–783 (1950).
Hoffmann, C., Leis, A., Niederweis, M., Plitzko, J. M. & Engelhardt, H. Disclosure of the mycobacterial outer membrane: cryo-electron tomography and vitreous sections reveal the lipid bilayer structure. Proc. Natl Acad. Sci. USA 105, 3963–3967 (2008).
Zuber, B. et al. Direct visualization of the outer membrane of mycobacteria and corynebacteria in their native state. J. Bacteriol. 190, 5672–5680 (2008).
Nikaido, H., Kim, S. H. & Rosenberg, E. Y. Physical organization of lipids in the cell wall of Mycobacterium chelonae. Mol. Microbiol. 8, 1025–1030 (1993).
Kaur, D., Guerin, M. E., Skovierova, H., Brennan, P. J. & Jackson, M. Chapter 2: Biogenesis of the cell wall and other glycoconjugates of Mycobacterium tuberculosis. Adv. Appl. Microbiol. 69, 23–78 (2009).
Jarlier, V. & Nikaido, H. Permeability barrier to hydrophilic solutes in Mycobacterium chelonei. J. Bacteriol. 172, 1418–1423 (1990).
George, K. M., Yuan, Y., Sherman, D. R. & Barry, R. C. E. The biosynthesis of cyclopropanated mycolic acids in Mycobacterium tuberculosis. Identification and functional analysis of CMAS-2. J. Biol. Chem. 270, 27292–27298 (1995).
Liu, J., Barry, R. C. E., Besra, G. S. & Nikaido, H. Mycolic acid structure determines the fluidity of the mycobacterial cell wall. J. Biol. Chem. 271, 29545–29551 (1996).
Glauner, B., Holtje, J. V. & Schwarz, H. The composition of the murein of Escherichia coli. J. Biol. Chem. 263, 10088–10095 (1988).
Lavollay, M. et al. The peptidoglycan of stationary-phase Mycobacterium tuberculosis predominantly contains cross-links generated by L,D-transpeptidation. J. Bacteriol. 190, 4360–4366 (2008).
Dover, L. G., Cerdeno-Tarraga, A. M., Pallen, M. J., Parkhill, J. & Besra, G. S. Comparative cell wall core biosynthesis in the mycolated pathogens, Mycobacterium tuberculosis and Corynebacterium diphtheriae. FEMS Microbiol. Rev. 28, 225–250 (2004).
Holtje, J. Growth of the stress-bearing and shape-maintaining murein sacculus of Escherichia coli. Microbiol. Mol. Biol. Rev. 62, 181–203 (1998).
Merkel, G. J., Stapleton, S. S. & Perry, J. J. Isolation and peptidoglycan of Gram-negative hydrocarbon-utilizing thermophilic bacteria. J. Gen. Microbiol. 109, 141–148 (1978).
Vollmer, W., Joris, B., Charlier, P. & Foster, S. Bacterial peptidoglycan (murein) hydrolases. FEMS Microbiol. Rev. 32, 259–286 (2008).
Hett, E. C. et al. A partner for the resuscitation-promoting factors of Mycobacterium tuberculosis. Mol. Microbiol. 66, 658–668 (2007).
Goffin, C. & Ghuysen, J. M. Multimodular penicillin-binding proteins: an enigmatic family of orthologs and paralogs. Microbiol. Mol. Biol. Rev. 62, 1079–1093 (1998).
Lavollay, M. et al. The peptidoglycan of Mycobacterium abscessus is predominantly cross-linked by L,D-transpeptidases. J. Bacteriol. 193, 778–782 (2011).
Mainardi, J.-L. et al. Novel mechanism of β-lactam resistance due to bypass of DD-transpeptidation in Enterococcus faecium. J. Biol. Chem. 275, 16490–16496 (2000).
Kardos, N. & Demain, A. L. Penicillin: the medicine with the greatest impact on therapeutic outcomes. Appl. Microbiol. Biotechnol. 92, 677–687 (2011).
Spratt, B. G. Distinct penicillin binding proteins involved in the division, elongation, and shape of Escherichia coli K12. Proc. Natl Acad. Sci. USA 72, 2999–3003 (1975).
Meyer, K. On penicillin. Science 96, 20–21 (1942).
Hobby, G. L., Meyer, K. & Chaffee, E. Observations on the mechanism of action of penicillin. Proc. Soc. Exp. Biol. Med. 50, 281–285 (1942).
Zapun, A., Contreras-Martel, C. & Vernet, T. Penicillin-binding proteins and beta-lactam resistance. FEMS Microbiol. Rev. 32, 361–385 (2008).
Mainardi, J. L., Hugonnet, J. E., Gutmann, L. & Arthur, M. Fighting resistant tuberculosis with old compounds: the carbapenem paradigm. Clin. Microbiol. Infect. 17, 1755–1756 (2011).
Nelson, D. E. & Young, K. D. Contributions of PBP 5 and DD-carboxypeptidase penicillin binding proteins to maintenance of cell shape in Escherichia coli. J. Bacteriol. 183, 3055–3064 (2001).
Dubee, V. et al. Kinetic analysis of Enterococcus faecium L,D-transpeptiase inactivation by carbapenems. Antimicrob. Agents Chemother. 56, 3409–3412 (2012).
Kohler, J. et al. In vitro activities of the potent, broad-spectrum carbapenem MK-0826 (L-749,345) against broad-spectrum beta-lactamase-and extended-spectrum beta-lactamase-producing Klebsiella pneumoniae and Escherichia coli clinical isolates. Antimicrob. Agents Chemother. 43, 1170–1176 (1999).
Hammond, M. L. Ertapenem: a Group 1 carbapenem with distinct antibacterial and pharmacologic properties. J. Antimicrob. Chemother. 53, ii7–ii9 (2004).
Dubee, V. et al. Inactivation of Mycobacterium tuberculosis L,D-transpeptidase LdtMt1 by carbapenems and cephalosporins. Antimicrob. Agents Chemother. 56, 4189–4195 (2012).
Dalhoff, A., Janjic, N. & Echols, R. Redefining penems. Biochem. Pharmacol. 71, 1085–1095 (2006).
Tomasz, A. The mechanism of the irreversible antimicrobial effects of penicillins: how the beta-lactam antibiotics kill and lyse bacteria. Annu. Rev. Microbiol. 33, 113–137 (1979).
Bayles, K. W. The bactericidal action of penicillin: new clues to an unsolved mystery. Trends Microbiol. 8, 274–278 (2000).
Uehara, T., Dinh, T. & Bernhardt, T. G. LytM-domain factors are required for daughter cell separation and rapid ampicillin-induced lysis in Escherichia coli. J. Bacteriol. 191, 5094–5107 (2009).
Suzuki, H., Nishimura, Y. & Hirota, Y. On the process of cellular division in Escherichia coli: a series of mutants of E. coli altered in the penicillin-binding proteins. Proc. Natl Acad. Sci. USA 75, 664–668 (1978).
Kawai, Y., Danilchanka, O. & Errington, J. Regulation of cell wall morphogenesis in Bacillus subtilis by recruitment of PBP1 to the MreB helix. Mol. Microbiol. 71, 1131–1144 (2009).
Valbuena, N. et al. Characterization of HMW-PBPs from the rod-shaped actinomycte Corynebacterium glutamicum: peptidoglycan synthesis in cells lacking actin-like cytoskeletal structures. Mol. Microbiol. 66, 643–657 (2007).
Hett, E. C., Chao, M. C. & Rubin, E. J. Interaction and modulation of two antagonistic cell wall enzymes of mycobacteria. PLoS Pathog. 6, e1001020 (2010).
Spratt, B. G. Temperature-sensitive cell division mutants of Escherichia coli with thermolabile penicillin-binding proteins. J. Bacteriol. 131, 293–305 (1977).
Yanouri, A., Danilchanka, O., Errington, J. & Buchanan, C. E. Cloning and sequencing of the cell division gene pbpB, which encodes penicillin-binding protein 2B in Bacillus subtilis. J. Bacteriol. 175, 7604–7616 (1993).
Errington, J., Danilchanka, O. & Scheffers, D. J. Cytokinesis in bacteria. Microbiol. Mol. Biol. Rev. 67, 52–65 (2003).
Valbuena, N. et al. Morphological changes and proteome response of Corynebacterium glutamicum to a partial depletion of FtsI. Microbiology 152, 2491–2503 (2006).
Tipper, D. J. & Strominger, J. L. Mechanism of action of penicillins: a proposal based on their structural similarity to acyl-D-alanyl-D-alanine. Proc. Natl Acad. Sci. USA 54, 1133–1141 (1965).
Wise, E. M. Jr & Park, J. T. Penicillin: its basic site of action as an inhibitor of a peptide cross-linking reaction in cell wall mucopeptide synthesis. Proc. Natl Acad. Sci. USA 54, 75–81 (1965).
Goebel, W. F. & Avery, O. T. A study of pneumococcus autolysis. J. Exp. Med. 49, 267–286 (1929).
Tomasz, A., Albino, A. & Zanati, E. Multiple antibiotic resistance in a bacterium with suppressed autolytic system. Nature 227, 138–140 (1970).
Kitano, K. & Tomasz, A. Escherichia coli mutants tolerant to beta-lactam antibiotics. J. Bacteriol. 140, 955–963 (1979).
Rogers, H. J., Thurman, P. F. & Burdett, I. D. The bactericidal action of beta-lactam antibiotics on an autolysin-deficient strain of Bacillus subtilis. J. Gen. Microbiol. 129, 465–478 (1983).
Kitano, K., Williamson, R. & Tomasz, A. Murein hydrolase defect in the beta lactam tolerant mutants of Escherichia coli. FEMS Microbiol. Lett. 7, 133–136 (1980).
Tomasz, A. The role of autolysins in cell death. Ann. NY Acad. Sci. 235, 439–447 (1974).
Cole, S. T. et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393, 537–544 (1998).
Kana, B. D., Mizrahi, V. & Gordhan, B. G. Depletion of resuscitation-promoting factors has limited impact on the drug susceptibility of Mycobacterium tuberculosis. J. Antimicrob. Chemother. 65, 1583–1585 (2010).
Chung, H. S. et al. Rapid β-lactam-induced lysis requires successful assembly of the cell division machinery. Proc. Natl Acad. Sci. USA 106, 21872–21877 (2009).
Goodell, E. W., Lopez, R. & Tomasz, A. Suppression of the lytic effect of beta lactams on Escherichia coli and other bacteria. Proc. Natl Acad. Sci. USA 73, 3293–3297 (1976).
Lopez, R., Ronda-Lain, C., Tapia, A., Waks, S. B. & Tomasz, A. Suppression of the lytic and bactericidal effects of cell wall inhibitory antibiotics. Antimicrob. Agents Chemother. 10, 697–706 (1976).
Rice, K. C. & Bayles, K. W. Molecular control of bacterial death and lysis. Microbiol. Mol. Biol. Rev. 72, 85–109 (2008).
Horne, D. & Tomasz, A. Tolerant response of Streptococcus sanguis to beta-lactams and other cell wall inhibitors. Antimicrob. Agents Chemother. 11, 888–896 (1977).
Moreillon, P., Marie, A., Nachman, S. & Tomasz, A. Two bactericidal targets for penicillin in pneumococci: autolysis-dependent and autolysis-independent killing mechanisms. Antimicrob. Agents Chemother. 34, 33–39 (1990).
Rice, K. C. et al. The Staphylococcus aureus cidAB operon: evaluation of its role in regulation of murein hydrolase activity and penicillin tolerance. J. Bacteriol. 185, 2635–2643 (2003).
Young, R. & Blasi, U. Holins: form and function in bacteriophage lysis. FEMS Microbiol. Rev. 17, 191–205 (1995).
Patton, T. G., Yang, S. J. & Bayles, K. W. The role of proton motive force in expression of the Staphylococcus aureus cid and lrg operons. Mol. Microbiol. 59, 1395–1404 (2006).
Mann, E. E. et al. Modulation of eDNA release and degradation affects Staphylococcus aureus biofilm maturation. PloS One 4, e5822 (2009).
Islam, M. S., Richards, J. P. & Ojha, A. K. Targeting drug tolerance in mycobacteria: a perspective from mycobacterial biofilms. Expert Rev. Anti. Infect. Ther. 10, 1055–1066 (2012).
Kohanski, M. A., Dwyer, D. J., Hayete, B., Lawrence, C. A. & Collado, I. A common mechanism of cellular death induced by bactericidal antibiotics. Cell 130, 797–810 (2007).
Foti, J. J., Devadoss, B., Winkler, J. A., Collins, J. J. & Walker, G. C. Oxidation of the guanine nucleotide pool underlies cell death by bactericidal antibiotics. Science 336, 315–319 (2012).
Keren, I., Wu, Y., Inocencio, J., Mulcahy, L. R. & Lewis, K. Killing by bactericidal antibiotics does not depend on reactive oxygen species. Science 339, 1213–1216 (2013).
Liu, Y. & Imlay, J. A. Cell death from antibiotics without the involvement of reactive oxygen species. Science 339, 1210–1213 (2013).
Grant, S. S., Kaufmann, B. B., Chand, N. S., Haseley, N. & Hung, D. T. Eradication of bacterial persisters with antibiotic-generated hydroxyl radicals. ACS Chem. Biol. 109, 12147–12152 (2012).
Wilke, M. S., Hills, T. L., Zhang, H.-Z., Chambers, H. F. & Strynadka, N. C. Crystal structures of the Apo and penicillin-acylated forms of the BlaR1 beta-lactam sensor of Staphylococus aureus. J. Biol. Chem. 579, 47278–47287 (2004).
Sala, C. et al. Genome-wide regulon and crystal structure of BlaI (Rv1846c) from Mycobacterium tuberculosis. Mol. Microbiol. 71, 1102–1116 (2009).
Yeats, C., Finn, R. D. & Bateman, A. The PASTA domain: a beta-lactam-binding domain. Trends Biochem. Sci. 27, 438 (2002).
Miller, C. et al. SOS response induction by beta-lactams and bacterial defense against antibiotic lethality. Science 305, 1629–1631 (2004).
Litzinger, S. et al. Muropeptide rescue in Bacillus subtilis involves sequential hydrolysis by beta-N-acetylglucosaminidase and N-acetylmuramyl-L-alanine amidase. J. Bacteriol. 192, 3132–3143 (2010).
Nikaido, H. Role of permeability barriers in resistance to beta-lactam antibiotics. Pharmacol. Ther. 27, 197–231 (1985).
Alvarez-Ortega, C., Wiegand, I., Olivares, J., Hancock, R. E. & Martinez, J. L. The intrinsic resistome of Pseudomonas aeruginosa to β-lactams. Virulence 2, 144–146 (2011).
Godfrey, A. J., Hatlelid, L. & Bryan, L. E. Correlation between lipopolysaccharide structure and permeability resistance in beta-lactam-resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 26, 181–186 (1984).
Ames, G. F.-L., Spudich, E. N. & Nikaido, H. Protein composition of the outer membrane of Salmonella typhimurium: effect of lipopolysaccharide mutations. J. Bacteriol. 117, 406–416 (1974).
Farhat, M. R. et al. Genomic analysis identifies targets of convergent positive selection in drug-resistant Mycobacterium tuberculosis. Nat. Genet. 45, 1183–1189 (2013).
Mailaender, C. et al. The MspA porin promotes growth and increases antibiotic susceptibility of both Mycobacterium bovis BCG and Mycobacterium tuberculosis. Microbiology 150, 853–864 (2004).
Niederweis, M., Danilchanka, O., Huff, J., Hoffmann, C. & Engelhardt, H. Mycobacterial outer membranes: in search of proteins. Trends Microbiol. 18, 109–116 (2010).
Danilchanka, O., Mailaender, C. & Niederweis, M. Identification of a novel multidrug efflux pump in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 52, 2503–2511 (2008).
Voladri, R. K. et al. Recombinant expression and characterization of the major beta-lactamase of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 42, 1375–1381 (1998).
Segura, C., Salvado, M., Collado, I., Chaves, J. & Coira, A. Contribution of beta-lactamases to beta-lactam susceptibilities of susceptible and resistant Mycobacterium tuberculosis clinical isolates. Antimicrob. Agents Chemother. 42, 1524–1526 (1998).
Bebrone, C. et al. Current challenges in antimicrobial chemotherapy: focus on ss-lactamase inhibition. Drugs 70, 651–679 (2010).
Cornaglia, G., Giamarellou, H. & Rossolini, G. M. Metallo-β-lactamases: a last frontier for β-lactams? Lancet Infect. Dis. 11, 381–393 (2011).
Parsons, L. M., Jankowski, C. S. & DeRiemer, K. Conjugal transfer of chromosomal DNA in Mycobacterium smegmatis. Mol. Microbiol. 28, 571–582 (1998).
Hirsh, A. E., Tsolaki, A. G., DeRiemer, K., Feldman, M. W. & Small, P. M. Stable association between strains of Mycobacterium tuberculosis and their human host populations. Proc. Natl Acad. Sci. USA 101, 4871–4876 (2004).
Dowson, C. G. et al. Horizontal transfer of penicillin-binding protein genes in penicillin-resistant clinical isolates of Streptococcus pneumoniae. Proc. Natl Acad. Sci. USA 86, 8842–8846 (1989).
Sifaoui, F., Arthur, M., Rice, L. B. & Gutmann, L. Role of penicillin-binding protein 5 in expression of ampicillin resistance and peptidoglycan structure in Enterococcus faecium. Antimicrob. Agents Chemother. 45, 2594–2597 (2001).
Pinho, M. G., Filipe, S. R., de Lencastre, H. & Tomasz, A. Complementation of the essential peptidoglycan transpeptidase function of penicillin-binding protein 2 (PBP2) by the drug resistance protein PBP2A in Staphylococcus aureus. J. Bacteriol. 183, 6525–6531 (2001).
Lu, W. P. et al. Penicillin-binding protein 2a from methicillin-resistant Staphylococcus aureus: kinetic characterization of its interactions with beta-lactams using electrospray mass spectrometry. Biochemistry 38, 6537–6546 (1999).
Pinho, M. G., de Lencastre, H. & Tomasz, A. An acquired and a native penicillin-binding protein cooperate in building the cell wall of drug-resistant staphylococci. Proc. Natl Acad. Sci. USA 98, 10886–10891 (2001).
Pucci, M. J. & Dougherty, T. J. Direct quantitation of the numbers of individual penicillin-binding proteins per cell in Staphylococcus aureus. J. Bacteriol. 184, 588–591 (2002).
Ito, T. et al. Structural comparison of three types of staphylococcal cassette chromosome mec integrated in the chromosome in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 45, 1323–1336 (2001).
Basu, J. et al. Identification and overexpression in Escherichia coli of a Mycobacterium leprae gene, pon1, encoding a high-molecular-mass class A penicillin-binding protein, PBP1. J. Bacteriol. 178, 1707–1711 (1996).
Sacco, E. et al. Activation of the L,D-transpeptidation peptidoglycan cross-linking pathway by a metallo-D,D-carboxypeptidase in Enterococcus faecium. Mol. Microbiol. 75, 874–885 (2010).
Gupta, R. et al. The Mycobacterium tuberculosis protein LdtMt2 is a nonclassical transpeptidase required for virulence and resistance to amoxicillin. Nat. Med. 16, 466–469 (2010).
Kumar, P. et al. Meropenem inhibits D,D-carboxypeptidase activity in Mycobacterium tuberculosis. Mol. Microbiol. 86, 367–381 (2012).
Acknowledgements
We wish to thank Lauren Solomon and the Broad Institute Communications Department for help with the illustrations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wivagg, C., Bhattacharyya, R. & Hung, D. Mechanisms of β-lactam killing and resistance in the context of Mycobacterium tuberculosis. J Antibiot 67, 645–654 (2014). https://doi.org/10.1038/ja.2014.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2014.94
This article is cited by
-
Structural insight into the inactivation of Mycobacterium tuberculosis non-classical transpeptidase LdtMt2 by biapenem and tebipenem
BMC Biochemistry (2017)
-
Non-classical transpeptidases yield insight into new antibacterials
Nature Chemical Biology (2017)
-
Protein-imprinted material for the treatment of antibiotic-resistant bacteria
Science Bulletin (2016)