Abstract
Wall teichoic acids are a major and integral component of the Gram-positive cell wall. These structures are present across all species of Gram-positive bacteria and constitute roughly half of the cell wall. Despite decades of careful investigation, a definitive physiological function for wall teichoic acids remains elusive. Advances in the genetics and biochemistry of wall teichoic acid synthesis have led to a new understanding of the complexity of cell wall synthesis in Gram-positive bacteria. Indeed, these innovations have provided new molecular tools available to probe the synthesis and function of these cell wall structures. Among recent discoveries are unexpected roles for wall teichoic acid in cell division, coordination of peptidoglycan synthesis and β-lactam resistance in methicillin-resistant Staphylococcus aureus (MRSA). Notably, wall teichoic acid biogenesis has emerged as a bona fide drug target in S. aureus, where remarkable synthetic-viable interactions among biosynthetic genes have been leveraged for the discovery and characterization of novel inhibitors of the pathway.
Similar content being viewed by others
Introduction
Wall teichoic acids are a major component of the Gram-positive cell wall, present in roughly equal proportions to peptidoglycan (Figure 1).1 Initially thought to have an ancillary role in bacterial physiology, wall teichoic acids have emerged in recent years as a critical component of the cell wall of Gram-positive bacteria. Functional roles for wall teichoic acids include determination of cell shape in the model Gram-positive bacterium Bacillus subtilis, and in Staphylococcus aureus, these structures serve important roles in host colonization, coordination of peptidoglycan synthesis and resistance to β-lactam antibiotics.2, 3, 4, 5, 6, 7, 8 Interestingly, wall teichoic acid biosynthetic proteins are encoded by genes that exhibit paradoxical gene dispensability patterns; deletions in early genes in the pathway result in viable but non-infectious organisms, and exhibit synthetic-viable interactions with otherwise essential late-acting genes.2, 7, 9, 10 Synthetic viability describes a genetic interaction in which the lethal phenotype associated with interruption of an essential gene is suppressed by simultaneous disruption of a second (non-essential) gene. The discovery of such synthetic-viable interactions in wall teichoic acid synthesis has enabled the rational discovery and characterization of novel antibacterial compounds that block wall teichoic acid biogenesis in S. aureus. Indeed, where methicillin-resistant S. aureus (MRSA) is a leading Gram-positive pathogen in an infectious disease crisis of global scale, wall teichoic acid appears to be an exciting new target for antibacterial chemical matter of unique chemical class and mechanism.11, 12, 13
Early foundational work on the chemistry and biology of wall teichoic acids, named after the Greek word τɛιχoζ (teichos; wall), was carried out during the 1950s and 1960s on strains of Bacilli, Lactobacilli and Staphylocci.14 Nucleotide-activated ribitol-phosphate and glycerol-phosphate were first identified in lysates of Lactobacillus arabinosus and, based on their similarity to Park’s nucleotide and precursors to other glycosyl-based macromolecules, were predicted to have a role in cell wall formation.15, 16 Follow-up inquiry into the biological function of activated glycosyl units led to the first identification of poly(ribitol-phosphate) in the wall of L. arabinosus.17, 18 Early examination of the structure of teichoic acids showed the common presence of polymers composed of either 1–3 linked units of glycerol-3-phosphate or 1–5 linked units of ribitol-5-phosphate decorated with hexose or N-acetylhexosamine residues, respectively, and D-alanine.19, 20 This work was followed by the demonstration that both nucleotide precursors and wall teichoic acids were present across a wide range of Gram-positive organisms.14, 21 As technologies in sample preparation and analysis advanced, a common linkage unit that anchored wall teichoic acid polymers to peptidoglycan was described, containing (glycerol-phosphate)-N-acetylmannosamine-β(1–4)-N-acetylglucosamine, and covalently linked to the 6′ hydroxyl of N-acetylmuramic acid residues of peptidoglycan (Figure 2).22, 23, 24 Advancements in tools for molecular biology and biochemistry enabled elucidation of the genetic requirements for wall teichoic acid biosynthesis, and the indispensable phenotype of various wall teichoic acid biosynthetic genes suggested an essential role for these structures in B. subtilis.25, 26, 27 Most recently, the development of soluble substrate analogs for teichoic acid biosynthetic intermediates has allowed for in vitro biochemical characterization of recombinant wall teichoic acid biosynthetic proteins.28, 29, 30, 31, 32 Cumulatively, this work led to the definition of both the structures and biosynthetic requirements of canonical poly(glycerol-phosphate) and poly(ribitol-phosphate) wall teichoic acids in B. subtilis 168 and S. aureus, respectively (Figure 2).
Synthesis of wall teichoic acid in B. subtilis 168 and S. aureus
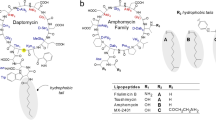
A number of Gram-positive bacteria are known to produce wall teichoic acid polymers having complex repeating units containing, for example, mannitol, erythritol, glucose or N-acetylglucosamine; however, a large proportion produce either poly(ribitol-phosphate) or poly(glycerol-phosphate) as the major polymer.33, 34, 35 Much of our knowledge of the genetics and biochemistry of wall teichoic acid synthesis has been elaborated in recent years in the model Gram-positive bacterium B. subtilis 168 and the pathogen S. aureus, which, respectively, produce poly(glycerol-phosphate) and poly(ribitol-phosphate) wall teichoic acids. In these organisms, wall teichoic acid is synthesized by tag (teichoic acid glycerol) or tar (teichoic acid ribitol) gene products. Regardless of polymer structure, wall teichoic acid synthesis occurs intracellularly on an undecaprenyl-phosphate lipid carrier that anchors the nascent polymer to the cytoplasmic face of the cellular membrane (Figure 3). Synthesis of a common linkage unit is initiated by TagO/TarO catalyzed transfer of an N-acetylglucosamine-1-phosphate residue from UDP-N-acetylglucosamine to undecaprenyl-phosphate to form the teichoic acid intermediate lipid α36 (Table 1 describes a straightforward nomenclature for teichoic acid intermediates based on the cognate enzyme.37 Lipid α is the substrate for TagA, lipid β is the substrate for TagB, etc. For polymeric substrates, such as the TagF substrate lipid φ.n, n denotes the number of repeating units in the polymer). Sequentially, TagA/TarA catalyzes the transfer of an N-acetylmannosamine residue to lipid α to generate lipid β.28, 29 Linkage unit synthesis is finalized by TagB/TarB with the addition of an sn-glycerol-3-phosphate unit yielding lipid φ.1.28, 38 Following linkage unit synthesis, steps for the completion of poly(glycerol-phosphate) and poly(ribitol-phosphate) polymers are unique to the respective polymers. In poly(glycerol-phosphate)-containing organisms, roughly 40 glycerol phosphate units are polymerized directly on lipid φ.1 via the TagF enzyme.39, 40, 41 Lipid-linked φ.40 is modified with multiple α-glucose units via the TagE enzyme, and exported to the extracellular surface of the cytoplasmic membrane via the TagGH ABC transport system.42, 43, 44, 45 In contrast, in poly(ribitol-phosphate)-containing organisms, lipid φ.1 is elaborated with an additional glycerol phosphate unit via the TarF enzyme to yield lipid φ.2, before ribitol phosphate polymerization via TarL.10, 32, 46 Intracellular decoration of lipid λ.40 in S. aureus includes modifications with both α-linked and β-linked N-acetylglucosamine, catalyzed by TarM and TarS, respectively.8, 47 Similar to the export of poly(glycerol-phosphate), poly(ribitol-phosphate) is transported to the extracellular surface of the cytoplasmic membrane by the TarGH ABC transport system. Once exported, the lipid-linked teichoic acid polymer is thought to be D-alanylated by gene products from the dltABCD operon and transferred from the undecaprenol lipid carrier to peptidoglycan.48 The final transfer of wall teichoic acid polymers from undecaprenol phosphate to muramic acid of peptidoglycan is thought to be carried out by a redundant set of three enzymes, namely LytR, Cps2a, Psr in B. subtilis 168 and Msr, SA0908 and SA2101 in S. aureus.49, 50 The latter biosynthetic assignments await in vitro biochemical confirmation.
Wall teichoic acid is a virulence factor required for host colonization
Wall teichoic acid is believed to have diverse functional roles including cation binding, osmotic tolerance, heat tolerance, regulation of autolysins, phage-binding and cell-shape determination.2, 51, 52, 53, 54 Further, the more recent discovery of the essential role for wall teichoic acid in coordinating mechanisms required for host infection and drug resistance in S. aureus has bolstered a concerted effort to uncover mechanisms underlying this physiology, and to discover inhibitors of wall teichoic acid biosynthesis for development as antimicrobial leads.5, 6, 55, 56
The importance of wall teichoic acid as a virulence factor was first elaborated by the Peschel group.3 In this study, the authors used a ΔtarO strain of S. aureus in a cotton rat nasal colonization model. Remarkably, after a 7-day incubation period, there was a complete absence of bacterial colonization in rats inoculated with the ΔtarO strain, whereas all rats in the test group inoculated with the isogenic wild-type strain were colonized (n=15 per group). Furthermore, the ΔtarO mutation caused a decrease in the capacity of S. aureus to both establish and disseminate infection in a rabbit endocarditis model.58 Careful investigation of the mechanistic underpinnings of the contribution of wall teichoic acid to these phenotypes was pursued. In an assessment of the effect of the ΔtarO genotype on the capacity of S. aureus to adhere to blood constituents, it was discovered that the mutation led to a reduction in bacterial adhesion to endothelial cells in in vitro models.58 These data established a role for wall teichoic acids in colonization via host tissue adhesion, and indicated a connection between deficiencies in in vivo bacterial proliferation and wall teichoic acid. The association between defects in wall teichoic acid and bacterial proliferation in vivo has been substantiated by reports of additional ΔtarO phenotypes in cell division and in susceptibility to innate immune components, including antimicrobial peptides, defencins and antimicrobial fatty acids.5, 57, 59, 60 Collectively, this work established a strict requirement for wall teichoic acid in the virulence of S. aureus, and helped to substantiate wall teichoic acid biosynthesis as an antibacterial drug target.
Complex dispensability patterns give rise to synthetic-viable genetic interactions among wall teichoic acid biosynthetic genes
Before the aforementioned reports investigating virulence of a ΔtarO S. aureus strain, wall teichoic acids were thought to be essential cellular structures. This conclusion was based on essential phenotypes evident for various wall teichoic acid biosynthetic genes.25, 26, 27 The revelation by the Peschel group that the tarO gene was dispensable in S. aureus led the Brown laboratory to undertake a meticulous reassessment of the dispensability of wall teichoic acid biosynthetic genes in B. subtilis 168 and S. aureus strain RN4220, chosen for its genetic malleability.2, 9 These investigations confirmed and extended previous studies revealing essential phenotypes both in B. subtilis 168 and S. aureus for genes encoding wall teichoic acid priming (tagB, tarB, tarF), polymerization (tagF), nucleotide-activated precursor synthesis (tagD, tarD, tarI, tarJ) and export (tarH). Paradoxically, these investigations also confirmed that viable and stable deletions could be generated in the first step in wall teichoic acid biosynthesis carried out by the tagO/tarO gene product. This paradox was resolved by demonstrating synthetic-viable genetic interactions between early and late steps. Indeed, both in B. subtilis 168 and S. aureus, the lethal phenotypes of all of the so-called ‘essential’ wall teichoic acid genes could be suppressed by deletion of tagO/tarO. The tagA/tarA gene, encoding the second step in wall teichoic acid synthesis, was also found to be dispensable and deletions therein could similarly suppress lethal phenotypes associated with loss of the downstream genes.7 The presence of two poly(ribitol-phosphate) polymerase genes in S. aureus has confounded definitive assignment of the dispensability of these genes, with indications that either one or both of the tarK and tarL polymerase genes are required to support growth in a wild-type background.10, 46 It is clear, however, that non-viable interruptions in polymerization step(s) can be rescued by deletion of tarO or tarA, similarly to remaining late-acting steps in wall teichoic acid synthesis. Through these genetic experiments, teichoic acid biosynthetic genes have been grouped into dispensable early-acting genes (tagO, tagA, tarO, tarA), or conditionally essential late-acting genes (tagB, tagD, tagF, tarB, tarD, tarF, tarI, tarJ, tarK, tarL). Furthermore, late-acting genes are essential in a wild-type background, but become dispensable in a ΔtagO/ΔtarO or ΔtagA/ΔtarA genetic background (Figure 4).
Synthetic-viable interactions between early- and late-acting wall teichoic acid biosynthetic genes. Deletions in late steps in wall teichoic acid biosynthesis are non-viable, whereas deletions in early steps are viable and can rescue the lethal phenotype of a late-step interruption. Depicted is a series of examples using the early gene tarO and late genes tarGH. (a) Wild-type organisms with intact early- and late-acting wall teichoic acid biosynthetic genes synthesize wall teichoic acid and are viable. (b) Interruption of late-steps, ΔtarGH shown, blocks wall teichoic acid synthesis and is non-viable. (c) Interruption of early steps, ΔtarO shown, blocks wall teichoic acid synthesis is and viable. (d) Simultaneous interruption of early and late steps blocks wall teichioc acid synthesis and is viable. Additional synthetic-viable combinations include ΔtarO/ΔtagO in combination with any late-acting gene deletion (tarBDFGHIJL/tagBDFGH), or ΔtarA/ΔtagA in combination with any late-acting gene deletion (tarBDFGHIJL/tagBDFGH).
Interestingly, additional synthetic-viable interactions have been noted recently in the MRSA strain COL. The TarG-mediated wall teichoic acid export step in this strain is essential in a wild-type background, however, viable mutations in strains resistant to inhibitors of the TarG exporter have been uncovered in the late-acting genes tarB and tarD.55 Although tarB and tarD have essential phenotypes in S. aureus strain RN4220,9 characterization of the S. aureus COL tarB and tarD suppressor mutants suggested loss-of-function mutations, and teichoic acid was found to be absent from the cell walls of these mutants. Nevertheless, tarB and tarD mutations conferred sensitivity to osmotic, temperature and antibiotic stresses that could be rescued by inactivation of tarO.55 Thus, although the observation of viable interruptions in late-acting genes in S. aureus COL is at odds with the binary essential/dispensable phenotypes documented in strain RN4220, a general relationship remains consistent: interruptions in late-acting genes give rise to compromised fitness, albeit of varying severity, that can be rescued by simultaneous inactivation of an early-acting gene. Genetic differences between S. aureus strains RN4220 and COL may explain the varying severity of phenotypes associated with deletions in late-acting steps within these strains. S. aureus strain RN4220 has been subjected to repeated mutagenesis to render it amenable to transformation with foreign DNA.61 This strain harbors interruptions in σB regulatory machinery, preventing the expression of associated stress response mechanisms.62 Stress sensing and response machinery is a vital component of an organism’s ability to survive cellular stressors. In the absence of this system, interruption of late-acting steps in wall teichoic acid synthesis may go unrecognized in strain RN4220 until a cell-death cascade is triggered. Conversely, in strain COL, a σB-mediated response could coordinate the required machinery to mitigate the deleterious effects of inhibition of wall teichoic acid biosynthesis. Ultimately, it is clear that genetic interactions among wall teichoic acid biosynthetic genes are complex and strain-dependent. Nevertheless, strong trends have emerged from a large body of work on this topic: the presence of teichoic acid polymers in the cell walls of B. subtilis 168 or S. aureus are not strictly essential, but deletion of a late-acting biosynthetic gene results in a fitness defect, the severity of which may range from sensitization to antibiotic stress, to death, and is dependent on both the bacterial strain and identity of the interrupted gene. Furthermore, late-acting genes display synthetic-viable interactions with early-acting genes, where the lethal phenotype caused by deletion of a late step can be suppressed by inactivation of an early step.
Insight into the mechanism underlying synthetic-viable interactions between early- and late-acting genes in wall teichoic acid synthesis was gained through an unbiased systems-scale investigation charting gene–gene and gene–chemical interactions in B. subtilis 168.63 In this study, the promoter PywaC was identified through microarray analysis as mounting an especially strong response following depletion of late enzymes in B. subtilis 168. Probing the PywaC promoter with a well-characterized library of bioactive small molecules (bioactives) demonstrated a similar induction of the promoter by cell–wall bioactives, with a strong bias toward chemicals that inhibit undecaprenol-linked metabolism. Furthermore, bioinformatic analysis examining gene–gene connectivity through genomic context inferred strong connectivity among genes involved in the biosynthesis of wall teichoic acid, undecaprenol and peptidoglycan. Taken together, these data suggested a model for the synthetic viability observed among early and late wall teichoic acid genes: deletion of a late-acting gene interrupts wall teichoic acid biosynthesis, resulting in the accumulation of dead-end undecaprenol-linked intermediates. Accumulation of undecaprenol-linked wall teichoic acid intermediates may deplete a limited cellular store of undecaprenol, similarly required for the synthesis of peptidoglycan, and thus result in cell death. Indeed, in a B. subtilis 168 strain with the tagF polymerase gene under the control of an inducible promoter, depletion of TagF resulted in a decrease in incorporation of D-[14C]glutamate into newly synthesized peptidoglycan.63 Alternately, as the structural integrity of membrane bilayers is determined by the physicochemical properties of bilayer components, it is possible that accumulation of undecaprenol-linked wall teichoic acid intermediates on the inner leaflet of the cytoplasmic membrane has a direct destabilizing effect on the bilayer.64 In either scenario, the deleterious accumulation of undecaprenol-linked wall teichoic acid intermediates can be avoided by preventing metabolite flux into the pathway with the deletion of the tagO or tagA genes.
Synthetic viability offers a platform for pathway-specific, cell-based screening for wall teichoic acid inhibitors
The discovery of unique synthetic-viable genetic interactions among wall teichoic acid genes underpinned the development of pathway-specific, cell-based screening for inhibitors of wall teichoic acid synthesis. The approach, which enables facile mechanistic follow-up on whole-cell-bioactive compounds while eliminating off-target nuisance compounds, has been successfully used in both academe and the pharmaceutical sector to discover inhibitors of the wall teichoic acid transport protein TarG.55, 56 First published by the Walker laboratory, compounds that are growth inhibitory to S. aureus are counter-screened against a tarO deletion strain.56 Chemicals leading to growth inhibition in the wild-type, and not the ΔtarO strain, are predominantly late-step inhibitors of wall teichoic acid synthesis. Compound 1835F03 was discovered and its potency was optimized through a structure–activity relationship analysis to yield targocil (Table 2).65 Interestingly, targocil has selective efficacy against S. aureus and no growth inhibitory effects on B. subtilis 168. In vitro enzymatic assays have been published for all intracellular steps in wall teichoic acid synthesis and these assays were subsequently used to rule out TarBDFIJL enzymes as potential targets. This pointed to either export or teichoic acid-peptidoglycan ligase enzymes as likely targets of targocil. Overexpression of tarGH was found to confer resistance, whereas expression of tagGH from the unsusceptible B. subtilis 168 in S. aureus conferred complete resistance. Mapping of spontaneous suppressor mutations conferring resistance to the action of targocil also identified TarG, the translocase component of the ABC export complex, was the antibiotic target.
Similarly, Merck and Company used this methodology to uncover inhibitors of wall teichoic acid biosynthesis within its whole-cell-bioactive collection of 20 000 anti-Staphylococcal small molecules.55 In this work, three diverse chemical classes of late-stage wall teichoic acid inhibitors were uncovered: tricyclic indole acids, N-aryl-triazoles and C-aryl-triazoles (Table 2). Mapping of suppressor mutations to the tarG gene once again implicated TarG as a target, and the inhibitors were found to be effective in reducing bacterial burden in a mouse thigh infection model. In both studies, the frequency of resistance to TarG inhibitors was high (∼7 × 106 at 8 × MIC), as resistance could be generated not only from mutations in the target protein but additionally from loss-of-function mutations in tarO or tarA. However, as deletions in early steps in wall teichoic acid synthesis render S. aureus avirulent, TarG inhibitor-resistant mutants with loss-of-function mutations in tarO or tarA were not viable in an in vivo model.
Taken together, efforts to search for late-step inhibitors at Merck and in the Walker laboratory, respectively, suggest that TarG is a highly druggable target that can be perturbed by chemicals of diverse structural class. The ease of discovery of TarG inhibitors is curious and due perhaps to its partial extracellular structure, or to its role as a wall teichoic acid translocase protein. Furthermore, the challenging biochemistry of this multitransmembrane domain protein remains an obstacle to rational in vitro optimization of bioactives targeting this structure, and efforts continue to discover leads that are active against more tractable late-step targets in the wall teichoic acid biosynthetic pathway.
A role for wall teichoic acid in β-lactam resistance in MRSA
The β-lactams are the most successful class of antibiotics in clinical history.66 Despite the clinical success of these molecules and the transformative role they have played in modern medicine, resistance to all β-lactam antibiotics has been documented, often shortly after introduction into the clinic. Resistance to β-lactams is commonly achieved via β-lactamase enzymes that inactivate the pharmacophore by hydrolyzing its β-lactam ring, rendering the antibiotic inert.67 To salvage efficacy of these drugs, β-lactams are commonly coformulated with a β-lactamase inhibitor, (e.g. Augmentin; amoxicillin+clavulanic acid). Although this approach is broadly successful for the treatment of Gram-negative infections, clinically important Gram-positive pathogens such as MRSA achieve β-lactam-resistance via additional mechanisms. In MRSA, resistance is determined in part by the presence of a horizontally acquired penicillin-binding protein (PBP), PBP2A, which is unsusceptible to inactivation by β-lactam antibiotics.68 While the presence of PBP2A was once thought to be the sole determinant for β-lactam resistance in S. aureus, it has become increasingly clear that this phenotype is supported by a complex network of resistance determinants, including PBPs (PBP2 and PBP4), and intriguingly, wall teichoic acid.
In 1994, the Murakami group69 conducted transposon-mediated mutagenesis of a clinical MRSA isolate to identify methicillin resistance determinants. The authors demonstrated that selective disruption of the llm gene could reverse high-level methicillin resistance in clinical isolates of MRSA. The llm gene was identified as the wall teichoic acid biosynthetic gene tarO almost a decade later and a focused evaluation of the connectivity between wall teichoic acid biosynthesis and β-lactam resistance in MRSA ensued.5, 36 This work demonstrated that selective genetic inactivation of tarO caused a β-lactam sensitization phenotype in both methicillin-sensitive and methicillin-resistant strains of S. aureus. The β-lactam sensitization phenotype was observed only upon interruption of the early-acting enzyme TarO and not the late-acting enzyme TarG, although coadministration of imipenem or oxacillin with a TarG inhibitor was able to elicit a three-log decrease in the frequency of TarG inhibitor-resistant mutations.5, 55 Furthermore, the β-lactam sensitization phenotype was found to be heterogeneous across a spectrum of β-lactam antibiotics, suggesting a very specific interaction between wall teichoic acids and peptidoglycan biosynthetic machinery. Further investigation of the connection between wall teichoic acid and peptidoglycan synthesis by electron microscopy uncovered clear phenotypes for defects in wall teichoic acid synthesis in cell division in S. aureus; interruption of TarO was linked to defects in cell septation and cell separation.5 Further analysis of the structural requirements for wall teichoic acid in β-lactam resistance linked this phenotype to the β-O-N-acetylglucosamine modification, rather than to the presence of the teichoic acid polymer itself.8 This observation is fascinating in the context of S. aureus wall teichoic acid modifications including both α- and β-O-N-acetylglucosamine, with only the β-linked sugar having a role in β-lactam resistance.8, 47
Ticlopidine reverses β-lactam resistance in MRSA: a new probe of wall teichoic acid synthesis and a promising drug combination
Given the requirement for wall teichoic acid in β-lactam resistance, there is strong therapeutic potential for a small-molecule inhibitor of an early step in teichoic acid synthesis. Toward this goal, the Brown laboratory developed a chemical combination screening strategy to exploit signature chemical–genetic interactions observed between tarO and β-lactam antibiotics.6 A pairwise screen of 2080 previously approved drugs in combination with cefuroxime was conducted against MRSA strain USA300. Previously approved drugs represent a rich source of bioactivity with the potential to be repurposed for new therapeutic benefit.70, 71 Furthermore, downstream drug development efforts with repurposed bioactives are advantaged by the availability of extensive safety and pharmacological data. While a screen for β-lactam sensitization should enrich for compounds targeting early steps in wall teichoic acid synthesis, Tan et al.72 recently demonstrated that inhibition of other cellular targets in S. aureus, including peptidoglycan biosynthesis and cell division, could likewise sensitize MRSA to β-lactams. Accordingly, molecules discovered to restore the efficacy of cefuroxime against MRSA were advanced to a counter screen to identify those that caused β-lactam sensitization via inhibition of an early step in wall teichoic acid biosynthesis. Bioactive molecules showing synergy in the primary screen were tested in a ΔtarO background for suppression of cefuroxime sensitization. Ticlopidine (Ticlid), an antihypertension drug that interrupts ADP-dependent platelet formation, was the only molecule to advance from this counter screen.73 Ticlopidine also showed signature synthetic-viable interactions with late-acting wall teichoic acid biosynthetic genes, suppressing the lethal phenotype caused by genetic or chemical inactivation of TarG. While ticopidine did not display any growth-inhibition activity, the ticlopidine–cefuroxime combination displayed potent and synergistic in vitro efficacy against 10 clinical S. aureus isolates, including nine MRSA strains, and efficacy in an in vivo S. aureus infection model. Phenotypes for ticlopine-treated S. aureus, including sensitization to β-lactam antibiotics, absence of teichoic acid from the cell wall and resistance to teichoic acid-specific phage, were consistent with phenotypes for tarO/tarA gene deletions, and provided further support for a mechanism for ticlopidine in inhibition of an early-step in wall teichoic acid biosynthesis. In vitro enzyme assays confirmed TarO to be the target, and the ticlopidine–cefuroxime combination was found to be selective for S. aureus.
The availability of a small-molecule inhibitor for TarO provided an opportunity to probe the mechanism of synergy between early steps in wall teichoic acid biosynthesis and transpeptidation steps in peptidoglycan biosynthesis. Indeed, well-characterized bioactive small molecules have frequently proved highly useful in understanding complex biological processes.74, 75, 76 Here, growth-inhibition phenotypes in MRSA were explored with a diverse collection β-lactam antibiotics in conjunction with TarO inhibition. Interestingly, blocking TarO function either with ticlopidine or by gene deletion sensitized MRSA only to β-lactams with a high affinity for PBP2, particularly the cephalosporins, and not to all β-lactams.6 The selective interaction of ticlopidine with PBP2-specific β-lactams is fascinating in the context of an emerging literature on the unique functions of individual PBPs in MRSA. PBP2 is the only bifunctional PBP with transpeptidase and transglycosylase activities in S. aureus and is essential to support life.77, 78 Localization of PBP2 to the division septum is required for the essential transglycosylase activity of this enzyme, and is mediated by an interaction between the transpeptidase active site and its transpeptidation substrate.79 Under β-lactam challenge, the transpeptidase active site on PBP2 is acylated, and autonomous localization to the division septum is inhibited. Under this stress, PBP2A, a horizontally acquired transpeptidase unsusceptible to inhibition by β-lactam antibiotics, carries out transpeptidation activities, and acts as a structural scaffold to recruit acylated PBP2 to the division septum.77, 79 In this manner, PBP2 remains properly localized under β-lactam challenge and can perform its essential transglycosylation function. This cooperative function of PBP2 and PBP2A yields peptidoglycan strands with low-level crosslinking, up to approximately five units in length.4, 80 Glycan strands with low-level crosslinking are substrates for PBP4, which functions as a secondary transpeptidase at the division septum to generate highly crosslinked peptidoglycan.4, 81 Thus, the activities of PBP2, PBP2A and PBP4 are required to synthesize the highly crosslinked cell wall in MRSA. Indeed, many MRSA strains are able to survive inhibition of transpeptidase activities on either PBP2 or PBP4, albeit with decreased amounts of highly crosslinked cell wall. However, simultaneous inhibition of both PBP2 and PBP4 transpeptidase activities is lethal.82 Remarkably, Atilano and co-workers demonstrated that the localization of PBP4 at the division site is dependent on the presence of the wall teichoic acid polymer.4 Taken together, these data allowed the Brown group to propose a model for the mechanistic basis for the synergy observed in MRSA between the TarO inhibitor ticlopidine and PBP2-specific antibiotics: PBP2-specific β-lactams inhibit the transpeptidation activity of PBP2, resulting in lowered levels of primary crosslinked cell wall, whereas ticlopidine inhibits the synthesis of wall teichoic acid, preventing proper localization and function of PBP4, and preventing secondary cell wall crosslinking. The low level of primary crosslinked cell wall synthesized under this challenge is insufficient to support life (Figure 5). Although untested at this time, it appears likely that β-lactam sensitivity reported to be associated with the loss of β-O-N-acetylglucosamine modifications to wall teichoic acid may also be due to a loss of PBP4 localization.8 Indeed, it is an intriguing idea that the wall teichoic acid polymer may well be a specific scaffold for subtle functions in peptidoglycan synthesis and cell division that are nevertheless absolutely critical to the complex manifestation of β-lactam resistance in MRSA.
A model for wall teichoic acid in β-lactam resistance in MRSA. (a) In the absence of β-lactam challenge, transglycosylase (TG) and transpeptidase (TP) domains in PBP2 work in concert with PBP2A to produce high levels of primary crosslinked peptidoglycan (PG). Wall teichoic acid (WTA) recruits PBP4 to the division septum where it catalyzes formation of highly crosslinked PG. (b) Under β-lactam challenge, the TP site of PBP2 is inhibited. TG activity of PBP2 and TP activity of PBP2A work in concert to produce reduced levels of primary crosslinked PG compared with the unchallenged condition. Primary crosslinked PG is further crosslinked by PBP4 in a WTA-dependent manner. (c) Under simultaneous challenge with a β-lactam and WTA inhibitor, PBP4 is mislocalized and does not synthesize highly crosslinked PG. The presence of low levels of primary crosslinked PG synthesized by PBP2 and PBP2A under β-lactam challenge are insufficient to support life.
Concluding remarks
Wall teichoic acid biosynthesis has recently emerged as an exciting new target in antibiotic research. Long thought to be ancillary structures in the cell wall of Gram-positive organisms, new roles for wall teichoic acid in the coordination of cell division, peptidoglycan synthesis and resistance to β-lactam antibiotics have emerged. A detailed understanding of the biology underpinning these events and the description of unique chemical and genetic interactions within these processes have provided the opportunity to develop focused cell-based screening tools for the discovery of inhibitors of both wall teichoic acid biosynthesis and β-lactam resistance in MRSA. Indeed, mechanistic follow-up on bioactives from high-throughput screening efforts is a time- and resource-intensive endeavor with low rates of success. The pathway-specific, cell-based screening strategies highlighted herein have exploited synthetic-viable interactions to enable focused discovery of pathway-specific bioactives, facilitating streamlined follow-up, elimination of nuisance compounds and ultimately, the discovery of inhibitors for TarO and TarG. Indeed, TarG appears to be a highly druggable target that is susceptible to a variety of chemical classes. Ticlopidine, a selective inhibitor of TarO, is strongly synergistic with PBP2-specific β-lactam antibiotics and restores the efficacy of these once-successful drugs for treatment of MRSA infections. Cumulatively, inhibitors of wall teichoic acid synthesis offer an exciting opportunity for the development of novel antibacterial leads with a new mechanism of action to treat drug-resistant Staphylococcal infections.
References
Hancock, I. C. Bacterial cell surface carbohydrates: structure and assembly. Biochem. Soc. Trans. 24, 183–187 (1997).
D’Elia, M. A., Millar, K. E., Beveridge, T. J. & Brown, E. D. Wall teichoic acid polymers are dispensable for cell viability in Bacillus subtilis. J. Bacteriol. 188, 8313–8316 (2006).
Weidenmaier, C. et al. Role of teichoic acids in Staphylococcus aureus nasal colonization, a major risk factor in nosocomial infections. Nat. Med. 10, 243–245 (2004).
Atilano, M. L. et al. Teichoic acids are temporal and spatial regulators of peptidoglycan cross-linking in Staphylococcus aureus. Proc. Natl Acad. Sci. USA 107, 18991–18996 (2010).
Campbell, J. et al. Synthetic lethal compound combinations reveal a fundamental connection between wall teichoic acid and peptidoglycan biosyntheses in Staphylococcus aureus. ACS Chem. Biol. 6, 106–116 (2011).
Farha, M. A. et al. Inhibition of WTA synthesis blocks the cooperative action of PBPs and sensitizes MRSA to β-lactams. ACS Chem. Biol. 8, 226–233 (2013).
D'Elia, M. A., Henderson, J. A., Beveridge, T. J., Heinrichs, D. E. & Brown, E. D. The N-acetylmannosamine transferase catalyzes the first committed step of teichoic acid assembly in Bacillus subtilis and Staphylococcus aureus. J. Bacteriol. 191, 4030–4034 (2009).
Brown, S. et al. Methicillin resistance in Staphylococcus aureus requires glycosylated wall teichoic acids. Proc. Natl Acad. Sci. USA 109, 18909–18914 (2012).
D'Elia, M. A. et al. Lesions in teichoic acid biosynthesis in Staphylococcus aureus lead to a lethal gain of function in the otherwise dispensable pathway. J. Bacteriol. 188, 4183–4189 (2006).
Pereira, M. P., D'Elia, M. A., Troczynska, J. & Brown, E. D. Duplication of teichoic acid biosynthetic genes in Staphylococcus aureus leads to functionally redundant poly(ribitol phosphate) polymerases. J. Bacteriol. 190, 5642–5649 (2008).
Klevens, R. M. et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298, 1763–1771 (2007).
Boucher, H. W. et al. Bad bugs, no drugs: no ESKAPE! An Update from the Infectious Diseases Society of America. Clin. Infect. Dis. 48, 1–12 (2009).
Brown, E. D. Is the GAIN Act a turning point in new antibiotic discovery? Can. J. Microbiol. 59, 153–156 (2013).
Armstrong, J. J., Baddiley, J., Buchanan, J. G., Carss, B. & Greenberg, G. R. Isolation and structure of ribitol phosphate derivatives (teichoic acids) from bacterial cell walls. J. Chem. Soc. 4344–4354 (1958).
Baddiley, J. & Mathias, A. P. Cytidine nucleotides. Part I. Isolation from Lactobacillus arabinosus. J. Chem. Soc. 2723–2731 (1954).
Baddiley, J., Buchanan, J. G., Carss, B., Mathias, A. P. & Sanderson, A. R. The isolation of cytidine diphosphate glycerol, cytidine diphosphate ribitol and mannitol 1-phosphate from Lactobacillus arabinosus. Biochem. J. 64, 599–603 (1956).
Baddiley, J., Buchanan, J. G. & Greenberg, G. R. A substance containing glycerophosphate and ribitol phosphate residues in Lactobacillus arabinosus. Biochem. J. 66, 51P–52P (1957).
Baddiley, J., Buchanan, J. G. & Carss, B. The presence of ribitol phosphate in bacterial cell walls. Biochim. Biophys. Acta 27, 220 (1958).
Burger, M. M. & Glaser, L. The synthesis of teichoic acids I. Polyglycerophosphate. J. Biol. Chem. 239, 3168–3177 (1964).
Glaser, L. The synthesis of teichoic acids. II. Polyribitol phosphate. J. Biol. Chem. 239, 3178–3186 (1964).
Clarke, P. H., Glover, P. & Mathias, A. P. The occurrence of polyol derivatives of cytidine diphosphate in micro-organisms. J. Gen. Microbiol. 20, 156–164 (1959).
Kaya, S., Yokoyama, K., Araki, Y. & Ito, E. N-acetylmannosaminyl(1–4)N-acetylglucosamine, a linkage unit between glycerol teichoic acid and peptidoglycan in cell walls of several Bacillus strains. J. Bacteriol. 158, 990–996 (1984).
Kojima, N., Araki, Y. & Ito, E. Structure of the linkage units between ribitol teichoic acids and peptidoglycan. J. Bacteriol. 161, 299–306 (1985).
Coley, J., Tarelli, E., Archibald, A. R. & Baddiley, J. The linkage between teichoic acid and peptidoglycan in bacterial cell walls. FEBS Lett. 88, 1–9 (1978).
Mauël, C., Young, M., Margot, P. & Karamata, D. The essential nature of teichoic acids in Bacillus subtilis as revealed by insertional mutagenesis. Mol. Gen. Genet. 215, 388–394 (1989).
Bhavsar, A. P., Beveridge, T. J. & Brown, E. D. Precise deletion of tagD and controlled depletion of its product, glycerol 3-phosphate cytidylyltransferase, leads to irregular morphology and lysis of Bacillus subtilis grown at physiological temperature. J. Bacteriol. 183, 6688–6693 (2001).
Bhavsar, A. P., Erdman, L. K., Schertzer, J. W. & Brown, E. D. Teichoic acid is an essential polymer in Bacillus subtilis that is functionally distinct from teichuronic acid. J. Bacteriol. 186, 7865–7873 (2004).
Ginsberg, C., Zhang, Y.-H., Yuan, Y. & Walker, S. In vitro reconstitution of two essential steps in wall teichoic acid biosynthesis. ACS Chem. Biol. 1, 25–28 (2006).
Zhang, Y.-H., Ginsberg, C., Yuan, Y. & Walker, S. Acceptor substrate selectivity and kinetic mechanism of Bacillus subtilis TagA. Biochemistry 45, 10895–10904 (2006).
Pereira, M. P. et al. The wall teichoic acid polymerase TagF efficiently synthesizes poly(glycerol phosphate) on the TagB product lipid III. Chem. Bio. Chem. 9, 1385–1390 (2008).
Sewell, E. W., Pereira, M. P. & Brown, E. D. The wall teichoic acid polymerase TagF is non-processive in vitro and amenable to study using steady state kinetic analysis. J. Biol. Chem. 284, 21132–21138 (2009).
Brown, S., Zhang, Y.-H. & Walker, S. A revised pathway proposed for Staphylococcus aureus wall teichoic acid biosynthesis based on in vitro reconstitution of the intracellular steps. Chem. Biol. 15, 12–21 (2008).
Archibald, A. R. in Advances in Microbial Physiology Vol. 11 (eds Rose A. H.) 53–96 Academic Press: London, (1974).
Naumova, I. B. et al. Cell wall teichoic acids: structural diversity, species specificity in the genus Nocardiopsis, and chemotaxonomic perspective. FEMS Microbiol. Rev. 25, 269–284 (2001).
Hancock, I. C. & Baddiley, J. Biosynthesis of the wall teichoic acid in Bacillus licheniformis. Biochem. J. 127, 27–37 (1972).
Soldo, B., Lazarevic, V. & Karamata, D. TagO is involved in the synthesis of all anionic cell-wall polymers in Bacillus subtilis 168. Microbiology (Reading, UK) 148, 2079–2087 (2002).
Pereira, M. P. & Brown, E. D. in Microbial Glycobiology: Structures, Relevance And Applications (eds Moran A. P., Holst O., Brennan P., Itzstein, von M.) 337–348 Academic Press: Burlington, MA, (2009).
Bhavsar, A. P., Truant, R. & Brown, E. D. The TagB protein in Bacillus subtilis 168 is an intracellular peripheral membrane protein that can incorporate glycerol phosphate onto a membrane-bound acceptor in vitro. J. Biol. Chem 280, 36691–36700 (2005).
Schertzer, J. W. & Brown, E. D. Purified, recombinant TagF protein from Bacillus subtilis 168 catalyzes the polymerization of glycerol phosphate onto a membrane acceptor in vitro. J. Biol. Chem. 278, 18002–18007 (2003).
Schertzer, J. W., Bhavsar, A. P. & Brown, E. D. Two conserved histidine residues are critical to the function of the TagF-like family of enzymes. J. Biol. Chem. 280, 36683–36690 (2005).
Schertzer, J. W. & Brown, E. D. Use of CDP-glycerol as an alternate acceptor for the teichoic acid polymerase reveals that membrane association regulates polymer length. J. Bacteriol. 190, 6940–6947 (2008).
Young, F. E., Smith, C. & Reilly, B. E. Chromosomal location of genes regulating resistance to bacteriophage in Bacillus subtilis. J. Bacteriol. 98, 1087–1097 (1969).
Honeyman, A. L. & Stewart, G. C. The nucleotide sequence of the rodC operon of Bacillus subtilis. Mol. Microbiol. 3, 1257–1268 (1989).
Allison, S. E., D'Elia, M. A., Arar, S., Monteiro, M. A. & Brown, E. D. Studies of the genetics, function, and kinetic mechanism of TagE, the wall teichoic acid glycosyltransferase in Bacillus subtilis 168. J. Biol. Chem. 286, 23708–23716 (2011).
Lazarevic, V. & Karamata, D. The tagGH operon of Bacillus subtilis 168 encodes a two-component ABC transporter involved in the metabolism of two wall teichoic acids. Mol. Microbiol. 16, 345–355 (1995).
Meredith, T. C., Swoboda, J. G. & Walker, S. Late-stage polyribitol phosphate wall teichoic acid biosynthesis in Staphylococcus aureus. J. Bacteriol. 190, 3046–3056 (2008).
Xia, G. et al. Glycosylation of wall teichoic acid in Staphylococcus aureus by TarM. J. Biol. Chem. 285, 13405–13415 (2010).
Neuhaus, F. C. & Baddiley, J. A continuum of anionic charge: structures and functions of D-alanyl-teichoic acids in gram-positive bacteria. Microbiol. Mol. Biol. Rev. 67, 686–723 (2003).
Kawai, Y. et al. A widespread family of bacterial cell wall assembly proteins. EMBO J. 30, 4931–4941 (2011).
Dengler, V. et al. Deletion of hypothetical wall teichoic acid ligases in Staphylococcus aureus activates the cell wall stress response. FEMS Microbiol. Lett. 333, 109–120 (2012).
Hoover, D. G. & Gray, R. J. Function of cell wall teichoic acid in thermally injured Staphylococcus aureus. J. Bacteriol. 131, 477–485 (1977).
Vergara-Irigaray, M. et al. Wall teichoic acids are dispensable for anchoring the PNAG exopolysaccharide to the Staphylococcus aureus cell surface. Microbiology 154, 865–877 (2008).
Young, F. E. Requirement of glucosylated teichoic acid for adsorption of phage in Bacillus subtilis 168. Proc. Natl Acad. Sci. USA 58, 2377–2384 (1967).
Schlag, M. et al. Role of Staphylococcal wall teichoic acid in targeting the major autolysin Atl. Mol. Microbiol. 75, 864–873 (2010).
Wang, H. et al. Discovery of wall teichoic acid inhibitors as potential anti-MRSA β-lactam combination agents. Chem. Biol. 20, 272–284 (2013).
Swoboda, J. G. et al. Discovery of a small molecule that blocks wall teichoic acid biosynthesis in Staphylococcus aureus. ACS Chem. Biol. 4, 875–883 (2009).
Peschel, A. et al. Inactivation of the dlt Operon in Staphylococcus aureus confers sensitivity to defensins, protegrins, and other antimicrobial peptides. J. Biol. Chem. 274, 8405–8410 (1999).
Weidenmaier, C. et al. Lack of wall teichoic acids in Staphylococcus aureus leads to reduced interactions with endothelial cells and to attenuated virulence in a rabbit model of endocarditis. J. Infect. Dis. 191, 1771–1777 (2005).
Kohler, T., Weidenmaier, C. & Peschel, A. Wall teichoic acid protects Staphylococcus aureus against antimicrobial fatty acids from human skin. J. Bacteriol. 191, 4482–4484 (2009).
Weidenmaier, C. & Peschel, A. Teichoic acids and related cell-wall glycopolymers in Gram-positive physiology and host interactions. Nat. Rev. Microbiol. 6, 276–287 (2008).
Nair, D. et al. Whole-genome sequencing of Staphylococcus aureus strain RN4220, a key laboratory strain used in virulence research, identifies mutations that affect not only virulence factors but also the fitness of the strain. J. Bacteriol. 193, 2332–2335 (2011).
van Schaik, W. & Abee, T. The role of sigmaB in the stress response of Gram-positive bacteria - targets for food preservation and safety. Curr. Opin. Biotechnol. 16, 218–224 (2005).
D'Elia, M. A. et al. Probing teichoic acid genetics with bioactive molecules reveals new interactions among diverse processes in bacterial cell wall biogenesis. Chem. Biol. 16, 548–556 (2009).
Zhang, Y.-M. & Rock, C. O. Membrane lipid homeostasis in bacteria. Nat. Rev. Microbiol. 6, 222–233 (2008).
Lee, K., Campbell, J., Swoboda, J. G., Cuny, G. D. & Walker, S. Development of improved inhibitors of wall teichoic acid biosynthesis with potent activity against Staphylococcus aureus. Bioorg. Med. Chem. Lett. 20, 1767–1770 (2010).
Walsh, C. Antibiotics: Actions, Origins, Resistance 1–335 ASM Press: Washington, DC, (2003).
Drawz, S. M. & Bonomo, R. A. Three decades of beta-lactamase inhibitors. Clin. Microbiol. Rev. 23, 160–201 (2010).
Lim, D. & Strynadka, N. C. J. Structural basis for the beta-lactam resistance of PBP2a from methicillin-resistant Staphylococcus aureus. Nat. Struct. Biol. 9, 870–876 (2002).
Maki, H., Yamaguchi, T. & Murakami, K. Cloning and characterization of a gene affecting the methicillin resistance level and the autolysis rate in Staphylococcus aureus. J. Bacteriol. 176, 4993–5000 (1994).
Ejim, L. et al. Combinations of antibiotics and nonantibiotic drugs enhance antimicrobial efficacy. Nat. Chem. Biol. 7, 348–350 (2011).
Spitzer, M. et al. Cross-species discovery of syncretic drug combinations that potentiate the antifungal fluconazole. Mol. Syst. Biol. 7, 499 (2011).
Tan, C. M. et al. Restoring methicillin-resistant Staphylococcus aureus susceptibility to beta-lactam antibiotics. Sci. Transl. Med. 4, 126ra35 (2012).
O'Brien, J. R., Etherington, M. D. & Shuttleworth, R. O. Ticlopidine—an antiplatelet drug: effects in human volunteers. Thromb. Res. 13, 245–254 (1978).
Farha, M. A. & Brown, E. D. Chemical probes of Escherichia coli uncovered through chemical–chemical interaction profiling with compounds of known biological activity. Chem. Biol. 17, 852–862 (2010).
Root, D. E., Flaherty, S. P., Kelley, B. P. & Stockwell, B. R. Biological mechanism profiling using an annotated compound library. Chem. Biol. 10, 881–892 (2003).
Falconer, S. B., Czarny, T. L. & Brown, E. D. Antibiotics as probes of biological complexity. Nat. Chem. Biol. 7, 415–423 (2011).
Pinho, M. G., de Lencastre, H. & Tomasz, A. An acquired and a native penicillin-binding protein cooperate in building the cell wall of drug-resistant staphylococci. Proc. Natl Acad. Sci. USA 98, 10886–10891 (2001).
Pinho, M. G., Filipe, S. R., de Lencastre, H. & Tomasz, A. Complementation of the essential peptidoglycan transpeptidase function of penicillin-binding protein 2 (PBP2) by the drug resistance protein PBP2A in Staphylococcus aureus. J. Bacteriol. 183, 6525–6531 (2001).
Pinho, M. G. & Errington, J. Recruitment of penicillin-binding protein PBP2 to the division site of Staphylococcus aureus is dependent on its transpeptidation substrates. Mol. Microbiol. 55, 799–807 (2005).
Leski, T. A. & Tomasz, A. Role of penicillin-binding protein 2 (PBP2) in the antibiotic susceptibility and cell wall cross-linking of Staphylococcus aureus: evidence for the cooperative functioning of PBP2, PBP4, and PBP2A. J. Bacteriol. 187, 1815–1824 (2005).
Wyke, A. W., Ward, J. B., Hayes, M. V. & Curtis, N. A. A role in vivo for penicillin-binding protein-4 of Staphylococcus aureus. Eur. J. Biochem. 119, 389–393 (1981).
Memmi, G., Filipe, S. R., Pinho, M. G., Fu, Z. & Cheung, A. Staphylococcus aureus PBP4 is essential for lactam resistance in community-acquired methicillin-resistant strains. Antimicrob. Agents. Chemother. 52, 3955–3966 (2008).
Acknowledgements
This work was supported by a Canada Research Chair salary award to EDB and operating funding from the Canadian Institutes of Health Research (MOP-15496).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sewell, E., Brown, E. Taking aim at wall teichoic acid synthesis: new biology and new leads for antibiotics. J Antibiot 67, 43–51 (2014). https://doi.org/10.1038/ja.2013.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2013.100
Keywords
This article is cited by
-
Lead generation of UPPS inhibitors targeting MRSA: Using 3D-QSAR pharmacophore modeling, virtual screening, molecular docking, and molecular dynamic simulations
BMC Chemistry (2024)
-
Anti-bacterial monoclonal antibodies: next generation therapy against superbugs
Applied Microbiology and Biotechnology (2022)
-
Structure of a proton-dependent lipid transporter involved in lipoteichoic acids biosynthesis
Nature Structural & Molecular Biology (2020)
-
Discovery of an antivirulence compound that reverses β-lactam resistance in MRSA
Nature Chemical Biology (2020)
-
Synergistic enhancement of beta-lactam antibiotics by modified tunicamycin analogs TunR1 and TunR2
The Journal of Antibiotics (2019)