Abstract
We analyzed the effect of antimicrobial use and implementation of a hand hygiene program on the incidence of healthcare-associated infections (HAIs) and healthcare-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) infections at the Chung Shan Medical University Hospital (Taichung, Taiwan). Monthly data were retrospectively reviewed from January 2004 to December 2010. Use of antimicrobials and alcohol-based hand cleaner were separately regressed against the incidences of HAIs and HA-MRSA infections. Infection incidence was expressed as persons per 1000 patient days (PDs), monthly use of i.v. antibiotics was expressed as defined daily doses per 1000 PDs and monthly alcohol-based hand cleaner use was expressed as bottle per 1000 PDs. Multivariate analysis indicated that use of hand cleaner was associated with reduced incidence of HAIs (P=0.0001) and HA-MRSA infections (P<0.0001). Time-series analysis indicated that increased use of hand cleaner was significantly associated with significant decreases in the incidences of HAIs and HA-MRSA infections. Total antibiotic use had no significant effect on HAIs, but was associated with more HA-MRSA infections. In addition, the use of J01CR01 antibiotics (combinations of penicillins, including β-lactamase inhibitors) in particular was correlated with significantly increased incidence of HA-MRSA infections. Our forecasting model demonstrates the efficacy of a hand hygiene program and the need to limit the use of certain restricted antimicrobials in order to reduce the incidence of HAIs and HA-MRSA infections.
Similar content being viewed by others
Introduction
The emergence of resistance to antimicrobial agents has become a major public health threat worldwide, especially in healthcare settings.1 In particular, infection with methicillin-resistant Staphylococcus aureus (MRSA) has increased rapidly during the last 15 years and is now a global health issue.2 MRSA has a significant prevalence in Asia, the United States and elsewhere, and has a significant impact on mortality and morbidity in healthcare settings.3
Recent studies have documented the epidemiology of healthcare-associated MRSA (HA-MRSA) and reported a recent trend of increasing prevalence in Europe and the USA. As of 2006, ∼20% of S. aureus isolates in Europe were reported as MRSA and 33–55% of isolates in the USA were reported as MRSA.4 Data from the National Nosocomial Infection Surveillance System indicate a steady increase in the incidence of HA-MRSA in intensive care unit (ICU) patients over time and that MRSA accounted for more than 60% of S. aureus isolates in ICUs from the USA in 2003.5
Before the 2003 epidemic of severe acute respiratory syndrome, the prevalence of HA-MRSA in Taiwan increased from 26.7% in 1990 to 60% in 1998–2000,6 then increased to 53–83% in 2003.7 Interestingly, after the 2003 severe acute respiratory syndrome epidemic, there was a decline in the prevalence of HA-MRSA in Taiwan. Lee et al.2 reported that the prevalence of MRSA decreased from 63.3% in 2001 to 54.1% in 2009 and that the incidence of HA-MRSA declined from 0.662 per patient day (PD) in 2001 to 0.233 per PD 2009 in central Taiwan. These findings agree with the results of Lai et al.8 in northern Taiwan, which indicated that the prevalence of MRSA decreased from 71.8% in 2000 to 54.9% in 2009.
We hypothesized that a decline in use of antibiotics and improved infection control measures would be associated with a decline in the incidence of HA-MRSA. Thus, in the present study, we used time-series analysis to retrospectively examine the relationship of antimicrobial usage, infection prevention by alcohol-based hand hygiene, and the presence of healthcare-associated infection (HAI) and HA-MRSA at a single medical institution in central Taiwan.
Results
Trends in HAIs and HA-MRSA infections and use of antimicrobials and hand cleaner
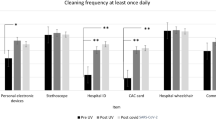
Table 1 shows the trends in the incidence of HAIs and HA-MRSA infections, in the use of antimicrobials and in the use of hand cleaner from January 2004 to December 2010. The monthly average incidences of HAIs and HA-MRSA infections were 3.24 per 1000 PD and 0.45 per 1000 PD, respectively, and there were significantly decreasing trends in the incidences of both types of infections, especially HAIs, after the initiation of hand hygiene promotion in January 2007 (Table 1, Figure 1). During the study period, the use of three antimicrobials increased, the use of six antimicrobials decreased and the use of three antimicrobials had no significant trend. The use of alcohol-based hand cleaner also increased significantly.
Correlations in use of antimicrobials and hand cleaner with incidence of HAIs
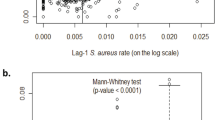
Figure 2 shows the trends in monthly usage of antimicrobials and hand cleaner vs the incidence of HAIs. Analysis of this data indicated a positive correlation between antimicrobial use and the logarithm of the incidence of HAIs (ρ=0.682, P<0.0001), and a negative correlation between use of hand cleaner and the logarithm of the incidence of HAIs (ρ=−0.390, P=0.0002).
Our multivariate model of the incidence of HAIs included two explanatory variables: total antimicrobial consumption and promotion of hand hygiene (Table 2). The results indicate that the promotion of hand hygiene was associated with a 0.015-unit decrease in the logarithm of the incidence of HAIs with no time lag (P=0.003), but there was no significant effect of total antimicrobial consumption on the incidence of HAIs. The multivariate model had an R2 of 0.539, indicating that 53.9% of the variation in the incidence of HAI is explained by these two variables.
Correlations of antimicrobial and hand cleaner use with incidence of HA-MRSA infections
Figure 3 shows the trends in monthly usage of antimicrobials and hand cleaner vs the incidence of HA-MRSA infections. Analysis of this data indicated a positive correlation between antimicrobial use and the incidence of HA-MRSA infections (ρ=0.439, P<0.0001), and a negative correlation between use of hand cleaner and the incidence of HA-MRSA infections (ρ=−0.350, P=0.0011). These trends are similar to those for HAIs (Figure 2), although there were much greater fluctuations in the incidence of moving average-MRSA infections (Figure 3).
Our first multivariate model (model I) of the incidence of HA-MRSA infections included two explanatory variables: total antibiotic use and the promotion of hand hygiene (Table 3). The results indicate that a 1-unit increase in total antibiotic use was associated with a 0.990-unit increase in the logarithm of incidence of HA-MRSA infections with a time lag of 2 months (P=0.0206) and that the promotion of hand hygiene was associated with a 0.400-unit decrease in the logarithm of the incidence of HA-MRSA infections with no time lag (P=0.00195). The multivariate model I had an R2 of 0.266, indicating that 26.6% of the variation in the incidence of HA-MRSA infections are explained by these two variables. The lower R2 of this model relative to the HAI model (Table 2) was related to the greater fluctuations in the incidence of HA-MRSA infections over time (Figure 3).
Model I indicated a significant association between total antibiotic use and incidence of HA-MRSA infections. Thus, we developed additional multivariate models to study the effect of each class of antimicrobial agents on the incidence of HA-MRSA infections (data not shown). Only the consumption of ‘J01CR01—combinations of penicillins, including β-lactamase inhibitors’—was significantly associated with the incidence of HA-MRSA, summarized as model II in Table 3. This model indicated that a 1-unit increase in the consumption of J01CR01 was associated with a 0.805-unit increase in the logarithm of incidence of HA-MRSA infections with a time lag of 1 month (P=0.0192) and that the promotion of hand hygiene was associated with a 0.491-unit decrease in the logarithm of the incidence of HA-MRSA infections with no time lag (P=0.0015). The multivariate model I had an R2 of 0.260, indicating that 26.0% of the variation in the incidence of HA-MRSA infections are explained by these two variables. The R2 of model II was 0.260, only slightly lower than that of model I (Table 3). In other words, a more restrictive model that only considers consumption of J01CR01 antibiotics explains almost as much of the variance as a model that considers consumption of all antimicrobials.
Discussion
The aim of the study was to assess the effect of antibiotic use and promotion of hand hygiene on the incidence of HAIs and HA-MRSA infections. There are three major findings in our study. First, our linear regression analysis indicated that the annual incidence of HAIs and HA-MRSA infections decreased over time. Second, forecasting models indicated that promotion of hand hygiene and use of antimicrobials was associated with reduced incidence of HAIs and reduced incidence of moving average-MRSA infections. Third, a forecasting model of the incidence of HA-MRSA that only considered use of J01CR01 antibiotics and hand hygiene was almost as effective as a model that considered use of all antimicrobials and hand hygiene.
Previous research has identified numerous risk factors for HA-MRSA, including prolonged hospital stay, exposure to broad-spectrum antibiotics and exposure to a greater number of antimicrobials.11, 12 Lucet et al.13 reported that the factors associated with MRSA in the ICU were older than 60 years, prolonged hospital stay, history of hospitalization or surgery and presence of open skin lesions in directly admitted patients. Antimicrobial use and infection control measures have important roles in the prevention of HAIs,14 but the need for a policy of active surveillance is controversial.15, 16
Much of the research on the effectiveness of hand-hygiene and antimicrobial stewardship has focused on the Gram-positive bacteria.15, 17 Previous studies have reported that most HAIs are transmitted via transient contamination of HCWs hands.12, 18 Thus, use of effective hand-hygiene practices, surveillance cultures and contact precautions have become major measures for infection control and prevention of MRSA.19
Studies of the effect of reducing antimicrobial use on the incidence of antimicrobial resistance have yielded various results.12, 14, 20 In 1990, Mouton et al.21 reported a correlation of methicillin resistance in coagulase-negative staphylococci and use of (flu)cloxacillin, cephalosporins and gentamicin. Other studies have reported correlations in use of antimicrobials and development of resistance in S. aureus.22 Tacconelli et al.23 performed a systemic meta-analysis and concluded that use of antibiotics increased the risk of MRSA.
Nonetheless, Monnet et al.22 reported the importance of study design in establishment of a relationship between antimicrobial use and MRSA and emphasized that confounding factors, such as noncompliance, selection bias and insufficiency of statistical power, are common. Thus, multicenter studies are recommended to reduce selection bias, and large sample sizes are recommended to increase statistical power.22 Nonetheless, many published studies have not fulfilled these criteria.15, 24
Importantly, Monnet et al.25 also noted that time-series analysis is a powerful and effective tool for analysis of the relationship of antimicrobial use and resistance surveillance data. Time-series analysis is a well-established area of statistical analysis that has been applied in various fields, such as industry and economics, and more recently in medical research.26 The Box–Jenkins approach uses autoregressive moving average (ARMA) or autoregressive integrated moving average (ARIMA) models for time-series analysis to make forecasts. López-Lozano et al.27 employed ARIMA (Box–Jenkins) and transfer function models to analyze antimicrobial use and resistance in ceftazidime-Gram-negative bacilli and imipenem-Pseudomonas aeruginasa. Their results indicated a temporal relationship between antimicrobial use and bacterial resistance. They were also able to quantify this effect and estimate the lag time between changes in antimicrobial use and changes in microbial resistance. An important requirement of time-series analysis is that it requires many measurements at uniform time intervals over a long period of time. Data on the monthly percentage of antimicrobial-resistant microorganisms and monthly use of antimicrobials in hospitals are readily available, so time-series analysis is well-suited for this type of data. Importantly, our monthly data indicate that significant short-term variations in microbial resistance and antimicrobial use, and these variations would have been obscured by simple analysis of yearly data.
We employed time-series analysis in the present study to overcome some of the limitations of our previous study on the effectiveness of infection control measures and changes in disease incidence.2 In particular, time-series analysis accounts for the lag period between the implementation of a control measure and the response. Nonetheless, our study had several limitations that must be noted. First, this study may have been subject to selection bias, because all the data were from a single institution. Thus, our findings may not reflect the overall situation in Taiwan.2 Second, our time-series analysis demonstrated a significant temporal relationship between antimicrobial use and promotion of the use of alcohol-based hand cleaner with the incidence of HAIs and HA-MRSA infections, but this relationship does not prove causality. Third, we did not assess the effect of numerous other variables, such as overall length of hospital stay, bed turnover rate, bed occupation rate, severity of disease and mortality.
Materials and methods
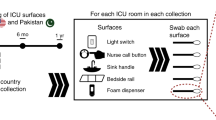
Hospital setting and infection control measures
Chung Shan Medical University Hospital (CSMUH) is a 1162-bed tertiary-care university hospital in Taichung, Taiwan. This was a retrospective study of adults admitted to CSMUH from January 2004 to December 2010. The guidelines of the Nosocomial Infection Control Society of Taiwan (NICST) and the Taiwan Center for Disease Control (CDC, http://www.cdc.gov.tw/) were used as infection control measures.
The hand hygiene practices included established hand-washing procedures, indications for hand hygiene, and hand hygiene posters in hand-washing facilities that were labeled ‘My five moments for hand hygiene’. All healthcare workers (HCWs) received continuing education and pre-service education on hand hygiene issues, and were told to perform hand hygiene procedures before touching a patient, before performing a clean or aseptic procedure, after exposure to body fluids and after touching a patient or a patient’s surroundings by the experienced Infection Control Nurses (ICN). HCW adherence was monitored and feedback was provided every month by ICN. HCWs were encouraged to educate their patients and families about proper hand hygiene. The volume of alcohol-based hand cleaner was also monitored by the Infection Control Committee and Medical Management Department of hospital. The volume of alcohol-based cleaner consumption was expressed as a rate bottle per 1000 PD.
Microbiological data
Monthly data of MRSA isolates were obtained from the microbiological laboratory and monthly data for all HA-MRSA infections were obtained from the Infection Control Committee. All MRSA isolates were nonduplicate samples. A duplicate was defined as an isolate of the same species, patient and antimicrobial susceptibility pattern within 1 month. Susceptibility testing was performed using the disk diffusion method and interpreted by Clinical and Laboratory Standards guidelines.9
Antimicrobial consumption
Data on monthly consumption of restricted antimicrobials and i.v. antibiotics were obtained from the Pharmacy Department. The systemic i.v. antimicrobials were included the unrestricted antimicrobials J01C β-lactam antibacterials penicillins (J01CF04 oxacillin, J01CF05 flucloxacillin), J01DB first-generation cephalosporins (cephazolin, cephradine), and J01CR01 combination of penicillins and β-lactamase inhibitors (amoxicillin/clavulanic acid). The restricted antimicrobials were J01CR05 combination of a penicillin and an anti-pseudomonal (piperacillin/tazobactam), J01DC second-generation cephalosporins (cefuroxime, cefmetazole), J01DD third-generation cephalosporins (cefotaxime, ceftazidime, ceftriaxone, cefoperazone and flomoxef), J01DE fourth-generation cephalosporins (cefepime, cefpirome), J01DH carbapenems (meropenem, imipenem/cilastatin) and J01G aminoglycosides (gentamycin, amikacin, isepamicin) J01M fluoroquinolones (ciprofloxacin, levofloxacin, and moxifloxacin), J01XA glycopeptides (vancomycin, teicoplanin), and J01AA12 tigecycline. Tigecycline was first used in CSMUH in January 2007, and ertapenem was first used in January 2006. Antimicrobial consumption was standardized as defined daily dose, as previously described.10
Use of alcohol-based hand cleaner
The alcohol-based hand cleaner was from a local manufacturer and contained 95% ethanol. Dispensers with this solution were placed at the entrances of all patient rooms, all bedsides in ICUs and dialysis rooms, nursing care work vehicles and in public places throughout the hospital. HCWs were also provided with pocket-sized containers of hand cleaners. The Pharmacy Department provided data on the use of hand cleaner.
Antimicrobial stewardship
An antimicrobial stewardship programme, which began in 2000, established the following four measures for antimicrobial administration and monitoring:
Restricted antimicrobials
Restricted antimicrobials were penicillin plus β-lactamase inhibitor combinations (piperacillin/tazobactam), second-generation cephalosporins (cefuroxime, cefmetazole), third-generation cephalosporins (cefotaxime, ceftazidime, ceftriaxone, cefoperazone, flomoxef), fourth-generation cephalosporins (cefepime, cefpirome), carbapenems (ertapenem, meropenem, imipenem/cilastatin) and aminoglycosides (amikacin, isepamicin) fluoroquinolones (ciprofloxacin, levofloxacin, and moxifloxacin), glycopeptides (vancomycin, teicoplanin), and tigecycline.
Antimicrobial indications
The Bureau of National Health Insurance in Taiwan regulates the indications for restricted antimicrobials (http://www.ejmii.com/guidelines.php) and includes three important new regulations: (a) discouragement of prophylactic use for surgery; (b) limiting the duration of therapy to 3 days in some clean surgeries (total hip replacement, total knee replacement, coronary artery bypass graft); and (c) restricted use in treatment of upper respiratory tract infections.
Computer assistance system
A hospital information system was used to monitor the prescriptions of all systemic i.v. antimicrobials with the following two rules: (a) an unrestricted antimicrobial was automatically discontinued on the seventh day; and (b) a restricted antibiotic required authorization from the infectious disease specialist, who provided authorization based on prior use of more than two different classes of antibiotics or use of antibiotics for more than 7 days.
Education and feedback
An infectious disease specialist educated clinicians, pharmacists and medical staff on the principles of antibiotic use in biannual education seminars. These seminars presented information about the appropriate use of antimicrobials, recommendations based on clinical symptoms and signs, diagnosis, liver and renal function, comorbidities, culture-susceptibility tests and adherence to guidelines.
Statistical analysis
All variables were initially log10-transformed to normalize distributions. The augmented Dickey–Fuller test indicated that variables were stationary at the 5% level. Trend analyses of variables were based on regressions vs time. Correlations between the use of all antimicrobials and of alcohol hand cleaners vs incidence of HAIs and HA-MRSA infections were evaluated by Spearman’s correlation coefficient (ρ).
A two-stage time series approach was used to determine the impact of antibiotic use and hand hygiene practice promotion on the incidence of HAIs and HA-MRSA infections. In the first step, ARIMA (p, d, q) models for the incidence of HAIs and HA-MRSA infections were indentified to control the self-effect of the incidences of HAIs and HA-MRSA infections, where p indicates the linear combination of the previous p terms in the time series, d is the times of the differences used to make the series stationary and q is the moving average term; that is, the weighted average from the previous q random noises. In this step, the ARIMA (0, 1, 1) model was used to determine the incidence of HAIs and the ARIMA (1, 0, 1) model was determine the incidence of HA-MRSA infections.
In the second step, the intervention of hand hygiene practice promotion and the total antimicrobial consumption were included in the multivariable models. If the total antimicrobial consumption was statistically significant, the nine variables for each kind of antimicrobial agent were included in the multivariable model, with the optimal lag length determined by the normalized BIC (Bayesian information criterion). The R2 is an indication of the percentage of variance in the outcome variable that is explained by the model.
A P-value less than 0.05 was considered statistically significant and all statistical analyses were performed with SPSS 15.0 (SPSS Inc, Chicago, IL, USA).
Conclusion
In conclusion, we successfully used a forecasting model to demonstrate a decline in the incidence of HAIs and HA-MRSA infections were associated with reductions in the use of some antimicrobials and with increased use of an alcohol-based hand cleaner over a 7-year period at a single hospital in Taiwan. Time-series analysis in conjunction with a broadly applied a stewardship program.12, 16 appears to be a powerful clinical tool for the analysis and prediction of infectious diseases and has potential to help reduce the incidence of HAIs and HA-MRSA infections.
References
Richet, H. M., Mohammed, J., McDonald, L. C. & Jarvis, W. R. Building communication networks: international network for the study and prevention of emerging antimicrobial resistance. Emerg. Infect. Dis. 7, 319–322 (2001).
Lee, Y. T. et al. Decline in the incidence of healthcare-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) correlates with deceased antimicrobial consumption at a tertiary care hospital in Taiwan, 2001-2009. Int. J. Antimicrob. Agents 36, 523–530 (2010).
Boucher, H. W. & Corey, G. R. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 46, S344–S349 (2008).
Appelbaum, P. C. MRSA-the tip of the iceberg. Clin. Microb. Infect. 12, 3–10 (2006).
Klevens, R. M. et al. System NNIS: changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992–2003. Clin. Infect. Dis. 42, 389–391 (2006).
Chen, M. L. et al. Longitudinal analysis of methicillin-resistant Staphylococcus aureus isolates at a teaching hospital in Taiwan. J. Formos. Med. Assoc. 98, 426–432 (1999).
Hsueh, P. R., Liu, C. Y. & Luh, K. T. Current status of antimicrobial resistance in Taiwan. Emerg. Infect. Dis. 8, 132–137 (2002).
Lai, C. C. et al. Correlation between antimicrobial consumption and resistance among Staphylococcus aureus and enterococci causing healthcare-associated infections at a university hospital in Taiwan from 2000 to 2009. Eur. J. Clin. Microbiol. Infect. Dis. 30, 265–271 (2010).
Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Tests. Approved Standard 9th Edition M2-A9 Wayne, PA, CLSI (2006).
Monnet, D. L. Measuring antimicrobial use: the way forward. Clin. Infect. Dis. 44, 671–673 (2007).
Herwaldt, L. A. Control of methicillin-resistant Staphylococcus aureus in the hospital setting. Am. J. Med. 106, S11–S18 (1999).
Cipolla, D., Giuffrè, M., Mammina, C. & Corsello, G. Prevention of nosocomial infections and surveillance of emerging resistances in NICU. J. Matern. Fetal Neonatal Med. 24, 23–6 (2011).
Lucet, J. C., Chevret, S., Durand-Zaleski, I., Chastang, C. & Regnier, B. . for the Multicenter Study Group. Prevalence and risk factors for carriage of methicillin-resistant Staphylococcus aureus at admission to the intensive care unit: results of a multicenter study. Arch. Intern. Med. 163, 181–188 (2003).
Weinstein, R. A. Controlling antimicrobial resistance in hospitals: infection control and use of antibiotics. Emerg. Infect. Dis. 7, 188–192 (2001).
Harris, A. D., McGregor, J. C. & Furuno, J. P. What infection control interventions should be undertaken to control multidrug-resistant gram-negative bacteria? Clin Infect Dis 43, S57–S61 (2006).
Ernst, E. J et al. Recommendations for training and certification for pharmacists practicing, mentoring, and educating in infectious diseases pharmacotherapy. Pharmacotherapy 29, 482–8 (2009).
Goff, D. A. Antimicrobial stewardship: bridging the gap between quality care and cost. Curr. Opin. Infect. Dis. 24, S11–20 (2011).
Cookson, B. et al. Staff carriage of epidemic methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 27, 1471–1476 (1989).
Alp, E. et al. Importance of structured training programs and good role models in hand hygiene in developing countries. J. Infect. Public Health 4, 80–90 (2011).
Cook, P. P., Catrou, P. G., Christie, J. D., Young, P. D. & Polk, R. E. Reduction in broad-spectrum antimicrobial use associated with no improvement in hospital antibiogram. J. Antimicrob. Chemother. 53, 853–859 (2004).
Mouton, R. P. et al. Correlations between consumption of antibiotics and methicillin resistance in coagulase negative staphylococci. J. Antimicrob. Chemother. 26, 573–583 (1990).
Monnet, D. L. Methicillin-resistant Staphylococcus aureus and its relationship to antimicrobial use: possible implications for control. Infect. Control Hosp. Epidemiol. 19, 552–559 (1998).
Tacconelli, E., De Angelis, G., Cataldo, M. A., Pozzi, E. & Cauda, R. Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis. J. Antimicrob. Chemother. 61, 26–38 (2008).
MacDougall, C. & Polk, R. E. Antimicrobial stewardship programs in health care systems. Clin. Microbiol. Rev. 18, 638–656 (2005).
Monnet, D. L. et al. Making sense of antimicrobial use and resistance surveillance data: application of ARIMA and transfer function models. Clin. Microbial. Infect. 7, 29–36 (2001).
Helfenstein, U. Box-jenkins modelling in medical research. Stat. Methods Med. Res. 5, 3–22 (1996).
López-Lozano, J. M. et al. Modelling and forecasting antimicrobial resistance and its dynamic relationship to antimicrobial use: a time series analysis. Int. J. Antimicrob. Agents 14, 21–31 (2000).
Acknowledgements
The study was supported by the Chung Shan Medical University Hospital Grant No. CSH-2009-C-004.
Author contributions: We declare that all the listed authors have participated actively in the study and all meet the requirements of the authorship. Dr YT Lee designed the study and wrote the protocol, Dr HC Hung and SM Tsao performed the study, Dr MC Lee and HJ Huang managed the literature searches and analyses, Dr SC Chen and HC Lin undertook the statistical analysis and Dr YT Lee wrote the first draft of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, YT., Chen, SC., Lee, MC. et al. Time-series analysis of the relationship of antimicrobial use and hand hygiene promotion with the incidence of healthcare-associated infections. J Antibiot 65, 311–316 (2012). https://doi.org/10.1038/ja.2012.20
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2012.20
Keywords
This article is cited by
-
Usefulness of dynamic regression time series models for studying the relationship between antimicrobial consumption and bacterial antimicrobial resistance in hospitals: a systematic review
Antimicrobial Resistance & Infection Control (2023)