Abstract
The aim of this study was to investigate the root canal configuration, accessory canals and number of main foramina of 123 maxillary second molars by means of micro-computed tomography. The teeth were scanned and reproduced with 3D software imaging. The root canal configuration and number of main foramina were evaluated by means of a four-digit system. The morphological complexity of human maxillary second molars is depicted by the number of accessory and connecting canals. The most frequently observed root canal configurations in the mesiobuccal root were 2-2-2/2 (19.5%), 2-2-1/1 (14.6%) and 2-1-1/1 (13.0%). A 1-1-1/1 configuration was observed in 93.5% and in 96.7% in the distobuccal and palatal roots, respectively. The MB1 root canal had one accessory canal (18.7%), and 8.9% of the MB2 root canal had one or two accessory canals. The distobuccal (11.3%) and palatal (14.6%) root canals had at least one accessory canal, and connecting canals were observed in 16.3% of mesiobuccal roots. The MB1, MB2, distobuccal and palatal root canals had one main foramen in 99.2%, 43.1%, 98.4% and 99.2% of samples, respectively. In the mesiobuccal root, one accessory foramen was detected in 14.6%, two were detected in 7.3%, and three were detected in 5.7%. The distobuccal root showed one or two accessory foramina in 9.1% of samples. The root canal configuration of maxillary second molars is quite heterogeneous; the mesiobuccal root has predominantly two root canal entrances (58.4%, 1 in 41.1%) with one main foramen (54.4%). Two main foramina were observed in 43.0%. Morphological variations, connecting and accessory canals were observed in all apical thirds.
Similar content being viewed by others
Introduction
Expertise in the field of root canal morphology is crucial for successful endodontic treatment.1, 2, 3 To avoid endodontic failure, especially during root canal preparation and/or obturation, the practitioner must have ample knowledge of the root morphology.3 Due to each tooth’s singularity, a large quantity of morphological variations is possible.3, 4 Such characteristics increase the difficulties in shaping, cleaning and filling the three-dimensional root canal system. Fulfilling such requirements is fundamental for a successful endodontic treatment and thus the long-term conservation of the tooth.5, 6 On the other hand, an inaccurate understanding of the complex internal root morphology invariably results in a deficient root canal preparation due to an inappropriate root canal shaping system and/or method. The most frequent anatomical root number described in the literature in maxillary second molars is three roots.7, 8, 9 However, these studies exhibit a lack of methodological accuracy when detecting and locating morphological microstructures such as accessory and communicating canals. These studies have employed a two-dimensional method, such as the radiographic method, which lacks a minute morphological interpretation. Currently, technological advancements in tooth imaging in clinical and in vitro settings have allowed the acquisition of high-resolution images. Micro-computed tomography offers in vitro possibilities for a relatively recent imaging technique, which allows for a precise, extensive and comprehensive description tooth morphology; however, it is a relatively expensive ex vivo research method.10, 11 The root canal morphology of the maxillary second molar has not been extensively reported; however, it is still controversial.7, 8, 9, 12 To the best of our knowledge, no study has been performed to assess the maxillary second molar with a high sample number by means of micro-computed tomography, thus allowing the practitioner to gain a broad morphological minute overview of this tooth. Different root canal system configuration classification systems are currently employed in the literature;1, 2 however, they do not encompass all possible root canal configurations. Therefore, considering the lack of detailed morphological information, specifically the root canal configuration of maxillary second molars, the aim of the present study was to investigate the morphology of three-rooted maxillary second molars and to describe their root canal system configuration by means of a previously proposed four-digit code system suggested by Briseño Marroquín et al.13
Materials and methods
Tooth selection
A total of 123 extracted human permanent maxillary second molars were obtained for reasons unrelated to the present study from dental clinics and dental practitioners. The teeth from an Egyptian population were stored in 5.25% sodium hypochlorite for 24 h for disinfection purposes.14 According to their morphological appearance with three clear distinct roots and a mesiodistal crown diameter of 9.0 mm (±0.2 mm),15 the selection criteria included complete development, no signs of root fracture or resorption, no radicular and coronal caries and no endodontic treatment. The teeth were cleaned, including any attached hard and soft tissues as well as calculus,with an ultrasonic scaler. The teeth were placed for one hour in a 3% hydrogen peroxide ultrasonic bath and then stored in 70% alcohol. For further investigation of the tooth’s internal morphology not related to that reported in this paper, endodontic access cavities, taking care not to influence the root canal system morphology nor the pulp chamber floor, were prepared under a stereo microscope (× 7; OPMIPico, Carl Zeiss Meditec AG, Jena, Germany) with a high-speed handpiece and a 801-014 diamond round bur (Komet, Lemgo, Germany). When required, ultrasonic tips were used to remove pulp stones exclusively from the pulp chamber. The pulp chambers were rinsed with 1% sodium hypochlorite (60 s) and dried via suction.
Main and accessory foramina
Main foramina were described as those whose diameters were 0.25 mm or more, and smaller foramina diameters were considered as accessory foramina.
Morphological analysis with micro-computed tomography
The teeth were scanned at an isotropic resolution of 20 μm in a desktop micro-computed tomography unit (μCT 40; Scanco Medical, Brüttisellen, Switzerland) using a previously described method16, 17, 18 using settings of 70 kV and 114 μA, resulting in 800 to 1 200 slices per tooth by rotation steps of 0.36 to 180°.
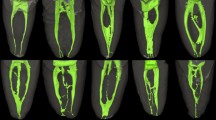
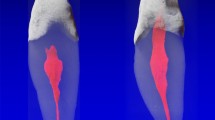
Different tooth structures were visualized through depiction in dummy colours in the 3D reconstructions of the micro-computed tomography scans using specific software (VGStudio Max 2.2; Volumegraphics, Heidelberg, Germany). The pulp chamber and root canal system were coloured red, the enamel and crown areas were coloured white to grey, and the root and dentin areas were coloured transparent grey (Figures 1 and 2). The root canal configuration was described by dividing the roots into thirds. The first, second and third configuration digits provide the root canal number at the respective coronal limit of the coronal, middle and apical thirds. The fourth digit is separated with a slash and indicates the number of main foramina.13 The number of accessory and connecting root canals (the one that connects one root canal with the same one or another without merging into the periapical tissue) as well as the number of apical accessory foramina observed under micro-computed tomography were also investigated. The results are expressed as absolute and relative values according to the sample number.
Maxillary second molar with a 1-1-1/1 root canal configuration in the palatal and distobuccal roots. This configuration type was found to be the most common (96.7% and 93.5%), respectively) in these roots. The configuration of the mesiobuccal root was 2-2-2/2 with a connecting canal in the middle third. This type of connecting canal could also be considered as an anastomosis; however, in this investigation, it was considered as a connecting canal for the sake of term consistency.
Results
The described root canal configurations of the mesiobuccal (MB), distobuccal (DB) and palatal (P) roots are shown in Table 1. The most frequently observed root canal configuration in the mesiobuccal root (MB1 and MB2 root canals together) was 2-2-2/2 (19.5%), followed by 2-2-1/1 (14.6%), 2-1-1/1 (13.0%), 2-1-2/2 (8.1%) and 1-1-2-/2 (7.3%). Nine additional different root canal configurations were observed with a frequency of <5% each. The distobuccal and palatal root canal configurations showed a 1-1-1/1 configuration as the highest incidence (93.5% and 96.7%, respectively). Five other root canal configuration variations were observed in the distobuccal root, whereas in the palatal root, only two variations could be observed.
The number and mean of accessory and connecting canals observed are shown in Table 2. Connecting canal I describes the communication between two root canals in the form of an isthmus, and connecting canal II resembles a “handle like” connecting canal that emerges from and returns to the same root canal. MB1, MB2, DB and P had no accessory canals in 74.8%, 91.1%, 79.7% and 85.4%, respectively. Connecting canals I and II were observed in only 20.3 and 6.5%, respectively. MB1 had one (18.7%), two (3.3%) or three (3.3%) accessory canals. MB2 showed one or two accessory canals in 8.9% of samples. The distobuccal (11.3%) and palatal (14.6%) roots had an incidence of at least one accessory canal. Connecting canal I was observed in 16.3% of teeth, and connecting canal II was observed in 6.5%.
The number and mean of main and accessory (Acc) apical foramina observed are shown in Table 3. The MB1, distobuccal and palatal root canals had one main foramen in 99.2%, 98.4% and 99.2% of samples, respectively. A main foramen in MB2 was observed in only 43.1% of samples. An additional root canal was rarely observed in the mesiobuccal (MB3), distobuccal (DB2) and palatal (P2) roots. Accessory foramina in the mesiobuccal root (MB-Acc) were detected in one (14.6%), two (7.3%) and three (5.7%) instances. In the distobuccal root, one or two accessory foramina were observed in 9.1% of samples (DB-Acc).
Discussion
A number of studies have investigated root canal morphology using various research methods.2, 4, 11, 19 For the analysis of the root canal system, the most accurate ex vivo method considered to be the gold standard20 today is micro-computed tomography.3 Fine internal morphological structures of the tooth can be observed with this noninvasive and reproducible technique after appropriate 3D reconstruction.21 Although we cannot completely exclude the possibility of tooth dehydration caused by the 70% alcohol storing procedure, if it happened, it did not influence the results, as it was extremely rare to observe an artefact in the resulting images after software rendering with micro-computed tomography that could have suggested possible dehydration. In experimental endodontic research, this method renders detailed qualitative and quantitative information.10, 21 Knowledge of the three-dimensional root canal system is mandatory to avoid errors during all phases of root canal treatment; thus, it will enhance the success of endodontic therapy.
To keep the number of samples high, only three-rooted maxillary second molars were included in the present study because two-7 and four-rooted maxillary second molars are rare.8 The most common root canal configuration systems employed are those of Vertucci2 and Weine et al.1 However, with different computer-supported imaging techniques such as micro-computed tomography, it has been possible to depict further root canal configurations that cannot be properly classified with these classification systems.4, 22, 23, 24, 25 The present study offers a comprehensive four-digit classification system based on dividing the root into thirds and using the fourth digit to describe the number of main apical foramina.13
The successive introduction of actual treatment modalities (microscopes) and different investigation methodologies9, 26, 27 showed that the prevalence of the MB2 root canal in maxillary molars is higher in comparison to radiographic studies.4 Therefore, only reports of high-resolution imaging systems were taken into consideration in the discussion.
In this study, 15 different root canal configurations were observed in the mesiobuccal root in maxillary second molars compared with 10 observed in the conventional microscopic investigation.28 The most frequently observed root canal configuration in the mesiobuccal root canal in this study was 1-1-1/1 (26.0%). With the same methodology, similar values of 26.0% were reported by Sert and Bayirli23 using teeth of male origin. Other authors4, 20, 29 report a relatively higher frequency of this configuration ranging from 38.1% to 45.09%. Versiani et al.12 reported a higher frequency of this configuration (76%) with the same investigative methodology; however, they used a smaller research sample (n=25) in four-rooted maxillary second molars. The frequency contrast with other investigations2, 23, 24 ranging from 56.0% to 71.0% and employing different methodologies also contrasted with these results. In the present study, a 2-2-2/2 configuration was observed in 19.5% of samples. Different authors using different methods2, 4, 12, 23, 26, 29 reported similar results to ours, whereas the results of other investigations with different methodologies or sample numbers that reported frequencies of 3.9%24 or 57.0%,11 and 60.3%22 deviated noticeably from ours.
The 2-2-1/1 and 2-1-1/1 root canal configurations were observed in 14.6% and 13.0% of the distobuccal and palatal roots, respectively. Indeed, when using different classification systems, these root canal configurations showed a similar outcome when compared with the results of other authors.2, 23 The findings of Sert and Bayirli23 (31.0% male and 22.0% female derived teeth) and Alavi et al.19 (7.7%) differed from ours; however, these authors used the type II (2-1) classification of Vertucci.2 A 1-1-1/1 root canal configuration in the distobuccal (93.5%) and palatal (96.7%) roots was observed in the present study. Similar results were obtained by Alavi et al.19 (98.1%–100% and 100%, respectively), Kim et al.24 (97.58% and 97.58%, respectively) and Sert and Bayirli23 (98% and 100%, respectively).
Although a MB2 root canal entrance was quite often present in the pulp chamber floor in this study (57.6%), our results and those of Vertucci2 show that the subsequent root canal configuration in the apical direction does not always reveal two separate root canals. A second mesiobuccal canal in the mesiobuccal roots was reported in 57%,11 66.6%29 and 70.3%;23 however, Versiani et al.12 and Kim et al.24 observed it in only 24.0% and 34.39%, respectively. Different investigations11, 23, 30 report that >50% of maxillary second molars have a second root canal (MB2) in the mesiobuccal root; therefore, if it is not properly anticipated, instrumented and filled, success in endodontic treatment is endangered.
Vertucci2 reported to have frequently found one main foramen in the mesiobuccal (88.0%), distobuccal (100.0%) and palatal (100.0%) roots. These results are similar when compared to those obtained in the present study (99.2%, 98.4% and 99.2%, respectively).
One, two and three lateral canals were observed in mesiobuccal roots in 14.6%, 7.3% and 5.7% of these roots, respectively. In the present study, the distobuccal root showed one or two lateral canals in 9.1% of samples. Contrastingly, Vertucci2 reported higher values in the mesiobuccal (50%), distobuccal (29%) and palatal (42%) roots. Alavi et al.19 reported lateral canals in 11.0% of the middle (0.5%) and apical thirds (10.5%), a result thatwas similar to our results. Furthermore, Alavi et al.19 reported a frequency of connecting canals between the mesiobuccal root canals of 16.2%, which was also in accordance with our results (16.3%). Vertucci2 reported a 21.0% frequency; however, he describes such connecting canals as “anastomosis.” We could also describe many of these connecting canals as anastomosis; however, we decided to compromise, using the term “connecting canal” for the sake of terminus unification to remain consistent throughout any reporting in this and other investigations.
In the present study, one to six accessory canals were observed in 27.6% of molars when considering the entire mesiobuccal and distobuccal root canal length. Similar findings were reported by De Deus31 in a study of three-rooted molars (23.3%). A higher prevalence in four-rooted maxillary second molars (38.0%) was reported by Versiani et al.12 These results are also in contrast with those of Cleghorn et al.3 in which they reported observing only one accessory canal in 10.8% of the mesiobuccal roots.
Differences between this and other studies can be explained by sample size, study methodology and design, ethnic origin of samples, and differences in age26 and sex.24, 32 However, to the best of our knowledge, only one micro-computed tomography study has investigated the root canal morphology and configuration of maxillary second molars.12 The results of our study also suggest that reported differences might be associated with the total root number of maxillary second molars.
The results of this study show that 49.5% of the mesiobuccal roots of maxillary second molars have two root canal entrances and that only 27.6% of them have only one physiological foramen. These conditions suggest that 55.7% of these teeth with two root canal entrances merge at some level of the root to ultimately end in only one physiological foramen. The meaning of these results could be erroneously interpreted as comforting for the operator. They could clinically explain why success has been achieved in many cases where only “three root canals” have been treated. However, the operator will practically never be aware of this clinical situation. Furthermore, the analysis of this information is beyond the scope of this investigation and will be extensively addressed in a future report.
A precise understanding of endodontic morphology of the maxillary second molar by means of imaging of a large sample number through micro-computed tomography is provided in the present study. This information will enable practitioners to understand and anticipate the challenge of three-dimensional endodontic treatment, especially during the cleaning and shaping of the root canal system. The results of this study showed that the maxillary second molar has a high incidence of morphological endodontic variables, indicating that it is even more complex than the maxillary first molar.13
Conclusions
-
The most frequently observed root canal configurations in the mesiobuccal root were 1-1-1/1 (26.0%), 2-2-2/2 (19.5%), 2-2-1/1 (14.6%) and 2-1-1/1 (13.0%).
-
The 1-1-1/1 root canal configuration was observed in the distobuccal root in 93.5% of samples and in the palatal root in 96.7% of samples.
-
The MB1 had one accessory canal in 18.7% of samples and the MB2 had one or two accessory canals in 8.9% of samples. The distobuccal and palatal root canals had at least one accessory canal in 11.3 and 14.6% of samples, respectively. Connecting canals were observed in 16.3% of the mesiobuccal roots.
-
Only one main foramen at the apex was observed in the MB1, distobuccal and palatal root canals in 99.2%, 98.4% of samples, respectively. A main foramen of MB2 was observed in 43.1% of samples. In 56.1% of samples, it did not exist due to the one (/1) final configuration in the mesiobuccal root.
-
One accessory foramen in mesiobuccal roots was detected in 14.6% of samples, two in 7.3% and three in 5.7%. The distobuccal root showed one or two accessory foramina in 9.1% of samples.
References
Weine FS, Healey HJ, Gerstein H et al. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surg Oral Med Oral Pathol 1969; 28 (3): 419–425.
Vertucci FJ . Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol 1984; 58 (5): 589–599.
Cleghorn BM, Christie WH, Dong CC . Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod 2006; 32 (9): 813–821.
Degerness RA, Bowles WR . Dimension, anatomy and morphology of the mesiobuccal root canal system in maxillary molars. J Endod 2010; 36 (6): 985–989.
Schilder H . Filling root canals in three dimensions. Dent Clin North Am 1967, 723–744.
Schilder H . Cleaning and shaping the root canal. Dent Clin North Am 1974; 18 (2): 269–296.
Eskoz N, Weine FS . Canal configuration of the mesiobuccal root of the maxillary second molar. J Endod 1995; 21 (1): 38–42.
Libfeld H, Rotstein I . Incidence of four-rooted maxillary second molars: literature review and radiographic survey of 1200 teeth. J Endod 1989; 15 (3): 129–131.
Peikoff MD, Christie WH, Fogel HM . The maxillary second molar: variations in the number of roots and canals. Int Endod J 1996; 29 (6): 365–369.
Rhodes JS, Ford TR, Lynch JA et al. Micro-computed tomography: a new tool for experimental endodontology. Int Endod J 1999; 32 (3): 165–170.
Domark JD, Hatton JF, Benison RP et al. An ex vivo comparison of digital radiography and cone-beam and micro computed tomography in the detection of the number of canals in the mesiobuccal roots of maxillary molars. J Endod 2013; 39 (7): 901–905.
Versiani MA, Pécora JD, de Sousa-Neto MD . Root and root canal morphology of four-rooted maxillary second molars: a micro-computed tomography study. J Endod 2012; 38 (7): 977–982.
Briseño-Marroquín B, Paqué F, Maier K et al. Root canal morphology and configuration of 179 maxillary first molars by means of micro-computed tomography. An ex vivo-study. J Endod 2015; 41 (12): 2008–2013.
Marroquín BB, El-Sayed MA, Willershausen-Zönnchen B . Morphology of the physiological foramen: I. Maxillary and mandibular molars. J Endod 2004; 30 (5): 321–328.
Jordan RE, Abrams L, Kraus BS . Kraus’ Dental Anatomy and Occlusion. St Louis: Mosby Year Book. 1992.
Paqué F, Ganahl D, Peters OA . Effects of root canal preparation on apical geometry assessed by micro-computed tomography. J Endod 2009; 35 (7): 1056–1059.
Peters OA, Boessler C, Paqué F . Root canal preparation with a novel nickel-titanium instrument evaluated with micro-computed tomography: canal surface preparation over time. J Endod 2010; 36 (6): 1068–1072.
Peters OA, Paqué F . Root canal preparation of maxillary molars with the self-adjusting file: a micro-computed tomography study. J Endod 2011; 37 (1): 53–57.
Alavi AM, Opasanon A, Ng YL et al. Root and canal morphology of Thai maxillary molars. Int Endod J 2002; 35 (5): 478–485.
Park JW, Lee JK, Ha BH et al. Three-dimensional analysis of maxillary first molar mesiobuccal root canal configuration and curvature using micro-computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108 (3): 437–442.
Plotino G, Grande NM, Pecci R et al. Three-dimensional imaging using microcomputed tomography for studying tooth macromorphology. J Am Dent Assoc 2006; 137 (11): 1555–1561.
Kim Y, Perinpanayagam H, Lee JK et al. Comparison of mandibular first molar mesial root canal morphology using micro-computed tomography and clearing technique. Acta Odontol Scand 2015; 73 (6): 427–432.
Sert S, Bayirli GS . Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod 2004; 30 (6): 391–398.
Kim Y, Lee SJ, Woo J . Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a korean population: variations in the number of roots and canals and the incidence of fusion. J Endod 2012; 38 (8): 1063–1068.
Lee KW, Kim Y, Perinpanayagam H et al. Comparison of alternative image reformatting techniques in micro-computed tomography and tooth clearing for detailed canal morphology. J Endod 2014; 40 (3): 417–422.
Pineda F, Kuttler Y . Mesiodistal and buccolingual roentgenographic investigation of 7275 root canals. Oral Surg Oral Med Oral Pathol 1972; 33 (1): 101–110.
Weine FS, Hayami S, Hata G et al. Canal configuration of the mesiobuccal root of the maxillary first molar of a Japanese sub-population. Int Endod J 1999; 32 (2): 79–87.
Kulild JC, Peters DD . Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod 1990; 16 (7): 311–317.
Silva EJ, Nejaim Y, Silva AI et al. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod 2014; 40 (2): 173–176.
Imura N, Hata GI, Toda T et al. Two canals in mesiobuccal roots of maxillary molars. Int Endod J 1998; 31 (6): 410–414.
De Deus QD . Frequency, location, and direction of the lateral, secondary, and accessory canals. J Endod 1975; 1 (11): 361–366.
Thomas RP, Moule AJ, Bryant R . Root canal morphology of maxillary permanent first molar teeth at various ages. Int Endod J 1993; 26 (5): 257–267.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Wolf, T., Paqué, F., Woop, AC. et al. Root canal morphology and configuration of 123 maxillary second molars by means of micro-CT. Int J Oral Sci 9, 33–37 (2017). https://doi.org/10.1038/ijos.2016.53
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijos.2016.53
Keywords
This article is cited by
-
The morphology of permanent maxillary first molars evaluated by cone-beam computed tomography among a Yemeni population
BMC Oral Health (2023)
-
A microcomputed tomographic analysis of the morphological variabilities and incidence of extra canals in mandibular first molar teeth in an Egyptian subpopulation
Scientific Reports (2023)
-
Three-dimensional morphologic classifications and analysis of canal isthmuses in permanent molars
Surgical and Radiologic Anatomy (2021)
-
The MB3 canal in maxillary molars: a micro-CT study
Clinical Oral Investigations (2020)
-
X-ray-Based 3D Virtual Histology—Adding the Next Dimension to Histological Analysis
Molecular Imaging and Biology (2018)