Abstract
Objective:
Resistance at the brain receptors for leptin and insulin has been associated with increased feeding, obesity and cognitive impairments. The causal agent for central resistance is unknown but could be derived from the blood. Here we postulate whether hypertriglyceridemia, the major dyslipidemia of the metabolic syndrome, could underlie central leptin and insulin resistance.
Design:
We used radioactively labeled triglycerides to measure blood–brain barrier (BBB) penetration, western blots to measure receptor activation, and feeding and cognitive tests to assess behavioral endpoints.
Results:
Human CSF was determined to contain triglycerides, a finding previously unclear. The radioactive triglyceride triolein readily crossed the BBB and centrally administered triolein and peripherally administered lipids induced in vivo leptin and/or insulin resistance at hypothalamic receptors. Central triolein blocked the satiety effect of centrally administered leptin. Decreasing serum triglycerides with gemfibrozil improved both learning and memory inversely proportionate to triglyceride levels.
Conclusions:
Triglycerides cross the blood–brain barrier rapidly, are found in human cerebrospinal fluid, and induce central leptin and insulin receptor resistance, decreasing satiety and cognition.
Similar content being viewed by others
Introduction
Leptin is a pluripotent regulatory protein that is secreted by adipose tissue and, crossing the blood–brain barrier (BBB), acts at its receptors in the brain to induce anorexia, increase thermogenesis, and support a number of central nervous system (CNS)-mediated actions related to cognition.1, 2, 3, 4, 5 A lack of leptin action in the brain, whether caused by the absence of the protein, an inability to cross the BBB (peripheral resistance), or resistance at its CNS receptor (central resistance), will result in profound obesity.6, 7 In humans, obesity is characterized not by an absence of leptin but by a resistance to its actions.8, 9 The cause of leptin resistance at its CNS receptor is unknown, but it is possibly a blood-derived factor that arises with the development of obesity.
Insulin is a peptide derived from the pancreas that crosses the BBB to affect feeding and cognition.10 Insulin resistance, especially CNS insulin resistance, is increasingly associated with cognitive impairment in general and Alzheimer’s disease in particular.11, 12, 13 Delivery of insulin to the brain has been shown to rapidly improve some aspects of cognition in individuals with Alzheimer’s disease and in young adults.14, 15 The cause of CNS insulin resistance is unknown, but its association with obesity, diabetes mellitus, and the metabolic syndrome are consistent with the involvement of a blood-derived factor.
Triglycerides could be that blood-derived factor. With fasting, serum triglycerides decrease, as they are used by peripheral tissues as an energy source. With prolonged fasting and during starvation, triglycerides are mobilized from adipose tissue,16 increasing blood levels of free fatty acids.17 Blood triglyceride levels also increase and their source is likely the liver. In the fasting/starved state, circulating free fatty acids are rapidly taken up by liver and reappear in the circulation as triglycerides.18, 19 Elevated blood triglycerides may have evolved as a starvation signal to the brain, with triglyceride-induced leptin resistance promoting survival by increasing the feeding drive and decreasing caloric expenditures that are unrelated to seeking calories. Triglycerides can indeed impair leptin transport across the BBB, inducing peripheral resistance.20 Hypertriglyceridemia is the classic dyslipidemia of obesity and the obesity-related conditions of metabolic syndrome and type II diabetes mellitus.21 In obesity, the hypertriglyceridemia-induced leptin resistance that promoted survival in starvation would be detrimental as it would promote continued feeding. Triglycerides are directly associated with the cognitive impairment associated with leptin-resistant conditions, including obesity and type II diabetes mellitus.22, 23 These direct effects on cognition raise the possibility that triglycerides can induce central leptin resistance. Similarly, several lines of evidence connect Alzheimer’s disease with triglycerides, dyslipidemia, and apolipoprotein E dysfunctions.24
However, we could find little information about the occurrence of triglycerides in the cerebrospinal fluid25 and no assessment on their ability to cross the BBB. Here, we determined the presence of triglycerides in human CSF, and in mice their ability to cross the BBB and to alter leptin and insulin brain receptor functions.
Materials and methods
Presence of triglycerides in human cerebrospinal fluid
Human CSF samples were collected as part of research studies approved by human subjects review committees of the University of Washington and the Veterans Affairs Puget Sound Health Care System. Written informed consent was obtained from all participants. A total of 39 subjects were fasted overnight, were aged 68±1.04 years, had a BMI 28±0.6 kg m−2, 20 (51%) subjects were female and 21 (53%) had the diagnosis of mild cognitive impairment. To obtain CSF, the L4-L5 space was accessed with a 24-gauge Sprott spinal needle (Sprott; Pajunk), and 30 ml of CSF was withdrawn into sterile syringes. Samples were divided into aliquots in prechilled polyethylene tubes, immediately frozen with dry ice, and stored at −70 °C until assays were performed. Colorimetric kit ‘L-Type Triglyceride M’ (Wako Diagnostics, Moutain View, CA, USA) was used to measure triglyceride levels and read in a standard plate reader at 620 nm at 37 °C.
Passage of triglycerides across the BBB
Male mice from our in-house colony (John Cochran VA, St Louis, MO, USA) were anesthetized with urethane and the right jugular vein and the left carotid artery exposed. 106 dpm of 3H-triolein (American Radiolabeled Chemicals, Inc. St. Louis, MO, USA) was injected into the jugular vein. At 2, 10 and 20 min after the iv injection, blood was obtained from the carotid artery and the mouse immediately decapitated. The levels of radioactivity were determined in arterial serum and whole brain by beta counting and results expressed as brain/serum ratios.
Preparation of triolein micelles
Triolein and l-phosphatidylcholine (Sigma-Aldrich Chemical Co., St Louis, MO, USA) were each dissolved in chloroform, mixed, and dried under a stream of nitrogen gas.20 Zlokovic’s buffer (pH 7.4; 7.19 g l−1 NaCl, 0.3 g l−1 KCl, 0.28 g l−1 CaCl2, 2.1 g l−1 NaHCO3, 0.16 g l−1 KH2PO4, 0.17 g l−1 anhydrous MgCl2, 0.99 g l−1 d-glucose and 10 g l−1 bovine serum albumin (BSA; which was added on the day of use) was added and the material vigorously mixed, homogenized and alternatively frozen in liquid nitrogen and thawed in a warm water bath for 12 cycles. The resulting lipid micelles were diluted to the desired concentration and used immediately or stored at minus 20 °C for use within 48 h.
Radioactive labeling of leptin and insulin
Recombinant murine leptin (R&D Systems, Minneapolis, MN, USA) or insulin was labeled by the chloramine-T method.3 Briefly, 5 microg of leptin or insulin was mixed with 1 mCi of 125I in a volume of 45 microl of 0.25 mm chloride-free sodium phosphate solution (pH 7.5). A volume of 5 μl of freshly prepared chloramine-T (2 mg ml−1 in sodium phosphate buffer) was added and mixed for 60 s at room temperature. The radioactively labeled leptin or insulin was separated from unincorporated iodine by purification on a G-10 column.
Effects of intracerebroventricular triglycerides on CNS leptin or insulin signaling
On day of study, male, 6–8-week-old CD-1 mice were fasted for 6 h the morning of the experiment. First, a dose–response curve was constructed for leptin in mice that were anesthetized with 40% urethane. Control mice received vehicle only and other mice received 1 μl of vehicle containing either 1 ng, 10 ng, 100 ng or 1 μg of leptin or 10 ng, 100 ng, 1 μg or 5 μg of human insulin into the lateral ventricle of the brain. These intracerebroventricular (ICV) injections were performed by reflecting the scalp and drilling a hole 1 mm lateral and 0.5 mm posterior to the bregma, followed by injection at a depth of 2.5 mm using a 26 g Hamilton syringe.
Second, the effect of triolein on leptin signaling as measured by the pSTAT3/STAT3 ratio was determined in three groups: mice receiving vehicle ICV, mice receiving 100 ng of leptin ICV, and mice receiving an ICV injection of 1 μl triglycerides (180 mg ml−1) 15 min prior to the ICV injection of leptin. Mice were killed 30 min after the second ICV injection. For insulin signaling, a similar protocol was used except that 1 μg of insulin rather than leptin was injected, mice were killed at 10 min after the second ICV injection, and the pAKT/AKT ratio was measured.
For analysis of pAKT and pSTAT3, supernatants were prepared from hypothalamic tissues dissolved in 100 μl of lysis buffer (PBS with 1% Triton X-1000, 5 mm EDTA, 1 mm PMSF, and protease and phosphatase inhibitor cocktail) and were resolved on a 4–12% Bis-Tris gel (Invitrogen, Grand Island, NY, USA). Protein was then transferred to nitrocellulose membranes using an iBlot transfer device (Invitrogen) and blocked for 1 h in 5% BSA dissolved in TBS-T. All antibody incubations were done at 4 °C overnight. The membranes were probed with an anti-pAKT or pSTAT3 rabbit monoclonal antibody (Cell Signaling, Danvers, MA USA). Membranes were then washed, and probed with anti-rabbit secondary antibody conjugated to horseradish peroxidase (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA). Following band visualization, blots were stripped. Blots were then re-probed with an anti-AKT mouse monoclonal antibody or anti-STAT3 rabbit monoclonal antibody (Cell Signaling), washed, and probed with anti-mouse or rabbit secondary (Santa Cruz Biotechnology, Inc.). Band intensities for phosphor-antibodies were then normalized to total antibody signal and made relative to the vehicle control. All immunoreactive bands were visualized using West Pico chemiluminescent substrate (Thermo Scientific, Rockford, IL, USA) and all images were captured using an ImageQuant LAS4000 CCD imaging system (GE Life Sciences, Piscataway, NJ, USA). Densitometric analysis was done using IQTL software (GE Life Sciences, Piscataway, NJ, USA).
Effect of triolein on brain distribution of ICV administered leptin
I-Lep was injected into the lateral ventricle of the brain as previously described in a volume of 1 μl of lactated Ringer’s solution. Triolein at a concentration of 180 mg ml−1 was included in the ICV injection. Arterial serum from the carotid artery was obtained 15 min after the ICV injection and then mice were immediately decapitated, the olfactory bulb collected and the whole brain dissected into 10 brain regions according to the method of Glowinski and Iverson.26 Brain regions were weighed and the levels of radioactivity determined.
Effect of triolein on leptin-induced anorexia
Mice were 12-week-old male CD-1 mice obtained from Charles River (Wilmington, MA, USA). Mice were adapted after transport from Charles River by giving food and water on an ad lib basis in rooms with a 12 h ligh–dark cycle with lights on at 0600 hours. Forty-eight hours prior to testing, the mice were anesthetized with isoflurane, placed in a stereotaxic instrument, and the scalp was deflected. A unilateral hole was drilled 0.5 mm posterior to and 1.0 mm to the right of the bregma. The injection depth was 2.0 mm into the third ventricle. Mice were individually housed and food deprived overnight before study. Fifteen minutes prior to the introduction of food, the mice were again placed under light anesthesia, and injected ICV with drug or vehicle. Two injections of 1 μl each, the first being 180 μg triolein or vehicle (Zlokovics buffer) and the second being 0.5 μg leptin or vehicle, were delivered over 30 s through a 30 gauge needle, which was attached to a 10 μl syringe. After the ICV injections, the scalp was closed and the mice were returned to their cages. Mice were given food of a known amount 15 min post injection, which was weighed 4 and 24 h later.
Gemfibrozil effects on cognition, brain weight and body weight
Retired breeders from our in-house colony (John Cochran VA, St Louis, MO, USA) were randomized into two groups given either gemfibrozil orally 1 g/kg dissolved in vegetable oil twice daily or vehicle. After 2 weeks, acquisition was measured in the active avoidance T-maze and after another 1 week of treatment, retention was measured. Higher T-maze scores reflect impaired acquisition (learning) and retention (memory). Mice were weighed at the beginning of treatment and after the measure of retention. Mice were then killed and brains weighed.
Effects of peripherally administered lipids on CNS leptin signaling
One mililiter of either whole milk or nonfat milk was administered intraperitoneally (IP) at t=0, 1h or 2 h. Four hours after the first IP injection, mice were anesthetized with urethane and received an ICV injection of lactated Ringer’s with or without 100 ng of leptin. Thirty minutes after the ICV injection, the hypothalamus was collected to determine leptin signaling as above. In additional animals, 106 dpm of tritiated triolein was included in the IP injections and the level of radioactivity measured in brain regions and serum 4 h after the first IP injection. The results for this part of the study are reported as the percent of the radioactive dose found in a gram of brain or ml of serum.
Statistics
Means are reported with their n’s and s.e., including those for the human CSF parameters. Two means were compared by t-test and more than two means were compared by analysis of variance (ANOVA) followed by Newman–Keuls multiple comparisons test. ANOVAs are reported with their degrees of freedom and P values. Regression lines were computed by the least squares method using the Prism 5 statistical package (GraphPad Inc., San Diego, CA, USA).
Results
Triglycerides were present in low amounts in human cerebrospinal fluid obtained from a convenience sample, having a mean level of 0.65±0.06 mg dl−1 (n=39, Figure 1a). To determine whether triglycerides could cross the BBB, we injected radioactive triolein into the jugular vein of the mouse and obtained the whole brain and blood from the carotid artery 2, 10 or 20 min later. Brain/serum ratios (Figure 1b) showed a rapid uptake of tritiated triolein into the brain. Radioactivity obtained from brains in which the vascular space had been washed out eluted in the position of tritiated triolein on thin layer chromatography, demonstrating that it was intact triolein and not the free fatty acid oleate or the glycerol backbone that had crossed the BBB.
Triglycerides are present in human CSF and cross the murine blood–brain barrier. (a) Triglycerides are detected in human lumbar cerebrospinal fluid drawn from a convenience sample (n=39). (b) The radioactively labeled triglyceride triolein crossed the mouse blood–brain barrier to accumulate in brain (n shown in parentheses).
We then determined whether trigylcerides could induce leptin resistance in the brain. We first injected leptin into the lateral ventricle of the brain to determine the dose needed to induce phosphorylation of STAT3 by the hypothalamic leptin receptor (Figure 2a ANOVA: F(4,14)=6.1, P<0.01). The dose–response curve indicated that 100 ng per mouse induced partial activation of the leptin receptor. To determine whether triglycerides could induce leptin receptor resistance, 100 ng of leptin was injected into the lateral ventricle of the brain with or without triolein (180 μg) and leptin receptor activation measured as the pSTAT3/STAT3 ratio. Triolein completely blocked the ability of leptin to activate its receptor (Figure 2b; ANOVA: F(2,14)=6.67, P<0.01), demonstrating that it can induce leptin resistance. Similarly, triolein blocked the ability of insulin to stimulate its receptor (Figure 2c; ANOVA: F(4,32)=7.4, P<0.001; 2D ANOVA F(2,25)=5.4, P<0.05).
Activation of the leptin or insulin receptor is inhibited by the triglyceride triolein. (a) Leptin given by intracerebroventricular (ICV) injection activates receptor signaling in a dose-dependent manner. (b) Co-administered triolein prevents leptin from activating its receptor. (c) Insulin given by ICV injection activates receptor signaling in a dose-dependent manner. (d) Co-administration of triolein prevents insulin from activating its receptor. Number in parentheses represents the n; *P<0.05; **P<0.01
We then determined whether triolein affected leptin binding in various brain regions. Triolein increased the uptake of I-Lep by whole brain, striatum, hypothalamus, occipital cortex, cerebellum, and midbrain. Levels of I-Lep were not affected by triolein administration in olfactory bulb, frontal cortex, parietal cortex, hippocampus, thalamus, pons-medulla or serum (Figure 3).
The behavioral consequences of triglyceride-induced leptin resistance were assessed by measuring two endpoints of leptin action within the CNS: inhibition of feeding and cognition. To assess feeding, 500 ng per mouse of leptin was injected into the lateral ventricle of the brain with or without 180 μg of triolein and food intake measured for 24 h (n=25, 26, 27/per group, respectively). In comparison to mice given an injection of vehicle, those injected with leptin ate less food as measured at 0–24 and 4–24 h, whereas those who were given leptin+triolein ate slightly more (Figure 4a; ANOVA: F(2,75)=4.43, P<0.05; Figure 4b ANOVA: F(2,75)=4.80, P<0.05); there were no statistically significant differences among the groups at 0–4 h (data not shown). Learning and memory were tested in a T maze avoidance task in mice treated with or without gemfibrozil. The drug lowered serum triglyceride levels by 46% and the measures of both acquisition (learning) and retention (memory) correlated inversely with blood triglyceride levels (Figure 5a: r=0.703, n=18, P<0.01); Figure 5b: r=0.733, n=18, P<0.001). Gemfibrozil had no significant effect on brain or body weight.
Co-Administration of the triglyceride triolein blocks the anorectic effect of leptin given by intracerebroventricular (ICV) injection. (a) Feeding results for 0–24 after ICV administrations (b) Feeding results for 4–24 h after ICV administrations. N=10 per group. V–-V: only vehicle was injected; V–L: leptin injected without triolein; T-–L: triolein and leptin co-injected. *P<0.05.
To determine whether peripheral triglycerides can cross the BBB in amounts sufficient to induce leptin resistance, we gave mice a total of 3 ml of whole milk IP over a 2 h period and then measured the ability of ICV leptin to activate the hypothalamic leptin receptor as measured by STAT phosphorylation (n=8–10 per group). We used nonfat milk as the control as it has a very similar composition to whole milk excepting the absence of fat, of which 98% is in the form of triglycerides.27 We found that the percent phosphorylation of STAT by the leptin receptor was decreased by about 1/3 in mice treated with IP whole milk in comparison to those treated with IP nonfat milk (Figures 5a and b; ANOVA: F(3,33)=19.5, P<0.001). We estimated the amount of the IP dose of triglycerides entering the brain and blood by including radioactive triolein in the IP injection of some animals. We found that about 1.3%, 1.1% and 4.1% of the administered dose was taken up per g of the hypothalamus, hippocampus, and whole brain, respectively (Figure 6c). About 12.8% was found per milliliter of serum. As about 3.5% of whole milk is triglycerides, this would suggest that about 1.25 mg of triglycerides were taken up per gram of hypothalamus.
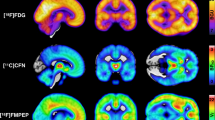
Peripheral triglycerides cross the BBB to induce leptin resistance. (a) Samples of western blots after IP no fat milk and ICV lactated Ringers’s solution (NC, n=9), IP no fat milk and ICV leptin (NL, n=8), IP whole fat milk and ICV lactated Ringer’s solution (WC, n=10), or IP whole fat milk and ICV leptin (WL, n=10). (b) ICV leptin induced less STAT phosphorylation in mice treated with IP whole milk than in mice treated with IP no fat milk. (c) Percent of IP dose of radioactive triolein co-administered with whole fat milk that was taken up by brain regions or serum; n=5 per group. *P<0.05; ***P<0.005; ****P<0.001.
Discussion
Triglycerides have been shown to induce peripheral leptin resistance.20 This raised the question of whether triglycerides could also induce central resistance to leptin or to insulin, two proteins noted for their centrally mediated effects on body weight and cognition. To induce central resistance, triglycerides would have to cross the BBB. However, we could find no studies assessing whether triglycerides could cross the BBB and very limited data on whether triglycerides were even present in the CSF.25 As such, we first determined whether triglycerides were detectable in human CSF. We found that triglycerides were present at about 0.65 mg dl−1, a level representing about 0.6% of blood levels.
We then assessed whether triglycerides could cross the BBB by injecting radioactive triolein into the jugular vein of anesthetized CD-1 male mice. Triglycerides rapidly appeared in brain with accumulation over time. To reach the observed level of nearly 100 μl g−1 at 20 min, the influx rate would have to be about 5 μl g−1 min−1, a rate associated with BBB transport for regulatory proteins.3, 28
We next determined whether triglycerides in the brain could induce leptin or insulin resistance at their CNS receptors. We first performed a dose–response curve to determine the amount of leptin needed to activate the leptin receptor at the hypothalamus. We chose 100 ng of leptin as a dose for further study as it partially activated the receptor. We found that triglycerides blocked the ability of leptin or insulin to activate their canonical signaling pathways. Because of the different structures of triglycerides and proteins, it is unlikely that triolein induces receptor resistance by competitively blocking the binding of a protein to its receptor. To begin to assess how a triglyceride might act to inhibit receptor activation, we injected radioactive leptin ICV with or without triolein and assessed leptin binding throughout the brain. Triolein altered leptin binding in whole brain and in five of the eleven brain regions assessed. However, leptin binding was not decreased, but increased, by triglycerides. This is not consistent with a competitive mechanism for inhibiting receptor activation but suggestive of an allosteric or post-receptor mechanism.
The consequences of triglyceride-induced receptor resistance were assessed by measuring two endpoints of leptin action within the CNS: inhibition of feeding and cognition. Administering leptin ICV decreases feeding and so we here assessed the effect of triolein on the anorexia induced by ICV-administered leptin. We found that leptin induced significant anorexia during the 24 h after its ICV administration. Triglycerides effectively inhibited the leptin-induced anorexia. Previous work has shown that injecting triglycerides directly into the brain impairs learning and memory.23 Here we assessed the effect of serum triglycerides on learning and memory by decreasing serum triglycerides with the drug gemfibrozil. This drug lowers serum triglyceride levels without affecting cholesterol levels and is used clinically to treat severe hyperlipidemia. We found that lowering serum triglycerides not only improved cognition, but that cognition was inversely related to serum levels of triglycerides.
Finally, we gave triglycerides peripherally in the form of whole milk. As we gave 3 ml of whole milk, which in the US is 3.25–-3.5% fat, we estimate we gave an IP dose of about 100 mg of triglycerides. We found that ICV leptin produced an increase in phophorylated STAT that was about 1/3 less in mice treated with whole milk as compared to those treated with no fat milk. By including radioactive triolein in a set of mice that had received the same regimen of whole milk as those studied for STAT phosphorylation, we could estimate how much of the IP triglycerides could have entered the brain. For hypothalamus, this value was about 1.3% of the IP dose per gram of brain tissue, which calculates to a little over 1 mg of triglycerides taken up per gram of brain tissue. However, unlike the formal measure of BBB permeability (Figure 1b), we did not determine the percent of the radioactivity that represented intact triglycerides. Since in this experiment the triglycerides would have been exposed to the peritoneum and circulated for hours and not minutes, it may be that some of this material represented breakdown product.
Triglyceride-induced leptin resistance would convey an evolutionary advantage during the early starvation phase by reducing anorexia and caloric expenditure. Serum leptin levels are typically reduced to 10–40% of baseline levels with starvation, with the amount of reduction being influenced by length of starvation and serum levels of insulin and glucose.29, 30, 31, 32 It may be that reversal of leptin’s actions during starvation is so advantageous to reproductive success that three levels of such inhibition have been conserved: impaired secretion by adipose tissue, inhibition of transport across the blood–brain barrier, inhibition of receptor function.
The above findings provide an additional mechanism by which the metabolic syndrome can contribute to cognitive difficulties and how it can ‘feed forward’ towards the obesity phenotype. The work also suggests that a significant lowering of serum triglyceride levels could reverse the cognitive impairments and help with weight loss, although these and our previous studies suggest that triglycerides will likely have to be lowered to below 100 mg dl−1.
In conclusion, we showed that triglycerides cross the BBB and induce central receptor resistance to leptin and insulin, with resulting effects on feeding and cognition. These results suggest that targeting triglyceride levels in blood could be a strategy for treating obesity and the cognitive problems associated with CNS resistance to leptin and insulin.
References
Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P . Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science (Washington DC) 1995; 269: 546–549.
Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz D et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Science (Washington DC) 1995; 269: 543–546.
Banks WA, Kastin AJ, Huang W, Jaspan JB, Maness LM . Leptin enters the brain by a saturable system independent of insulin. Peptides 1996; 17: 305–311.
Oomura Y, Hori N, Shiraishi T, Fukunaga K, Takeda H, Tsuji M et al. Leptin facilitates learning and memory performance and enhances hippocampal CA1 long-term potentiation and CaMK II phosphorylation in rats. Peptides 2006; 27: 2738–2749.
Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T et al. Effects of the obese gene product on body weight regulation in ob/ob mice. Science (Washington DC) 1995; 269: 540–543.
Halaas JL, Boozer c, Blair-West J, Fidahusein N, Denton DA, Friedman JM . Physiological response to long-term peripheral and central leptin infusion in lean and obese mice. Proc Natl Acad Sci USA 1997; 94: 8878–8883.
van Heek M, Compton DS, France CF, Tedesco RP, Fawzi AB, Graziano MP et al. Diet-induced obese mice develop peripheral, but not central, resistance to leptin. J Clin Invest 1997; 99: 385–390.
Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 1996; 334: 292–295.
Schwartz MW, Peskind E, Raskind M, Boyko EJ, Porte D Jr . Cerebrospinal fluid leptin levels: relationship to plasma levels and adiposity in humans. Nat Med 1996; 2: 589–593.
Banks WA . Insulin in the brain: there and back again. Pharmacol Ther 2012; 136: 82–93.
Craft S, Peskind E, Schwartz MW, Schellenberg GD, Raskind M, Porte D Jr . Cerebrosinal fluid and plasma insulin levels in Alzheimer's disease: relationship to severity of dementia and apolipoprotein E genotype. Neurology 1998; 50: 164–168.
Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM . Diabetes and the risk of dementia: The Rotterdam Study. Neurology 1999; 53: 1907–1909.
Talbot K, Wang H-Y, Kazi H, Han L-Y, Bakshi KP, Stucky A et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dyregulation, and cognitive decline. J Clin Invest 2012; 122: 1316–1338.
Benedict C, Hallschmid M, Hatke A, Schultes B, Fehm HL, Born J et al. Intranasal insulin improves memory in humans. Psychoneuroendocrinology 2004; 29: 1326–1334.
Craft S, Baker LD, Montine TJ, Minoshima S, watson GS, Claxton A et al. Intranasal insulin therapy for Alzheimer's disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch Neurol 2012; 69: 29–38.
MacDonald RS, Smith RJ . Starvation. In: Becker KL (ed) Principles and Practice of Endocrinology and Metabolism vol. 3 Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2007; pp 1247–1251.
Samra JS, Clark ML, Humphreys SM, McDonald IA, Frayn KN . Rgulation of lipid metabolism in adipose tissue during early starvation. Am J Physiol 1996; 271: E541–E546.
Guiducci L, Jarvisalo M, Kiss J, Nagren K, Viljanen A, Naum AG et al. [11C]palmitate kinetics across the splanchnic bed in arterial, portal and hepatic venous plasma during fasting and euglycemic hyperinsulinemia. Nucl Med Biol 2006; 33: 521–528.
Palmer JF, Cooper C, Shipley RA . Rate of release of hepatic triacylglycerol into serum in the starve rat. Biochem J 1978; 172: 219–226.
Banks WA, Coon AB, Robinson SM, Moinuddin A, Shultz JM, Nakaoke R et al. Triglycerides induce leptin resistance at the blood-brain barrier. Diabetes 2004; 53: 1253–1260.
Eckel RH, Grundy SM, Zimmet PZ . The metabolic syndrome. Lancet 2005; 365: 1415–1428.
Perlmuter LC, Nathan DM, Goldfinger SH, Russo PA, Yates J, Larkin M . Triglyceride levels affect cognitive function in noninsulin-dependent diabetics. J Diabet Complications 1988; 2: 210–213.
Farr SA, Yamada KA, Butterfield DA, Abdul HM, Xu L, Miller NE et al. Obesity and hypertriglyceridemia produce cognitive impairment. Endocrinology 2008; 149: 2628–2636.
Salameh TS, Rhea EM, Banks WA, HAnson AJ . Insulin resistance, dyslipidemia, and apolipoprotein E interactions as mechanisms in cognitive impairment and Alzheimer's disease. Exp Biol and Med 2016; 241: 1676–1683.
Kamat DV, Chakravorty BP . Comparative values of CSF-cholesterol and CSF-triglycerides along with other biochemical parameters in neurological disorders. Indian J Med Sci 1996; 50: 280–284.
Glowinski J, Iversen LL . Regional studies of catecholamines in the rat brain. I. The disposition of [3H]norepinephrine, [3H]dopamine and [3H]dopa in various regions of the brain. J Neurochem 1966; 13: 655–669.
Christie W . C Composition and structure of milk lipids. In:Fox PF (ed) Advanced Dairy Chemistry Volume 2: Lipids. Chapman and Hall: London, UK, 1994. pp 1–36.
Banks WA, Ortiz L, Plotkin SR, Kastin AJ . Human interleukin (IL) 1alpha, murine IL-1alpha and murine IL-1 beta are transported from blood to brain in the mouse by a shared saturable mechanism. J Pharmacol Exp Ther 1991; 259: 988–996.
Boden G, Chen X, Mozzoli M, Ryan I . Effect of fasting on serum leptin in normal human subjects. J Clin Endocrinol Metab 1996; 81: 3419–3423.
Weigle DS, Duell PB, Connor WE, Steiner RA, Soules MR, Kuijper JL . Effect of fasting, refeeding, and dietary fat restriction on plasma leptin levels. J Clin Endocrinol Metab 1997; 82: 561–565.
Faggioni R, Moser A, Feingold KR, Grunfeld C . Reduced leptin levels in starvation increase susceptibility to endotoxic shock. Am J Pathol 2000; 156: 1781–1787.
Sinha MK, Opentanova I, Ohannesian JP, Kolaczynski JW, Heiman ML, Hale J et al. Evidence of free and bound leptin in human circulation. Studies in lean and obese subjects during short-term fasting. J Clin Invest 2008; 98: 1277–1282.
Acknowledgements
This work is supported by the VA, R01AG046619 and R21NS093368.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Banks, W., Farr, S., Salameh, T. et al. Triglycerides cross the blood–brain barrier and induce central leptin and insulin receptor resistance. Int J Obes 42, 391–397 (2018). https://doi.org/10.1038/ijo.2017.231
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.231
This article is cited by
-
Ameliorative effects of zinc supplementation on cognitive function and hippocampal leptin signaling pathway in obese male and female rats
Scientific Reports (2023)
-
Novel insights into non-alcoholic fatty liver disease and dementia: insulin resistance, hyperammonemia, gut dysbiosis, vascular impairment, and inflammation
Cell & Bioscience (2022)
-
Biomolecular Effects of Dance and Dance/Movement Therapy: A Review
American Journal of Dance Therapy (2022)
-
Targeting the TLR4/NF-κΒ Axis and NLRP1/3 Inflammasomes by Rosuvastatin: A Role in Impeding Ovariectomy-Induced Cognitive Decline Neuropathology in Rats
Molecular Neurobiology (2022)
-
Associations between lipids in selected brain regions, plasma miRNA, and behavioral and cognitive measures following 28Si ion irradiation
Scientific Reports (2021)