Abstract
Background:
Childhood obesity is an important risk factor for premature development of the metabolic syndrome (MetS) at adulthood. There is need for understanding of the mechanisms underlying the MetS and obesity. Patients with Cushing’s disease suffer from similar metabolic complications, leading to the hypothesis that inter-individual cortisol variation may contribute to the onset of obesity. In addition, glucocorticoid receptor (GR)-gene polymorphisms resulting in differential glucocorticoid (GC) sensitivity, have been associated with an adverse metabolic profile.
Aim:
To study associations of GC levels in scalp hair, as a marker of long-term systemic GC concentrations, and genetically determined GC sensitivity with obesity and body-fat distribution in children.
Methods:
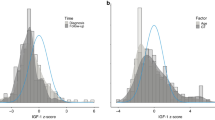
We performed a cross-sectional study of cortisol and cortisone concentrations over a 3-month period, measured by LC-MS/MS (Liquid Chromatography Tandem Mass Spectrometry) in hair of 3019 6-year-old children participating in the Generation R study. Genotyping of GR-gene polymorphisms was performed.
Results:
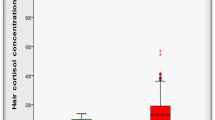
Of all children, 4.3% was obese and 13.4% overweight. Cortisol was significantly associated with risk of obesity (odd ratio (OR): 9.4 (3.3–26.9)) and overweight (OR: 1.4 (1.0–2.0)). Cortisone was associated with risk of obesity (OR: 1.9 (1.0–3.5)). Cortisol and cortisone were significantly positively associated with body mass index, fat mass (FM) index and android/gynecoid FM ratio. GR polymorphisms were not associated with adiposity parameters.
Conclusion:
Long-term cortisol concentrations are strongly associated with an increased risk of childhood obesity and adverse body-fat distribution. Future research may reveal whether these are causal relations and may be a target for therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 2005; 111: 1999–2012.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012; 307: 483–490.
Ljung T, Andersson B, Bengtsson BA, Bjorntorp P, Marin P . Inhibition of cortisol secretion by dexamethasone in relation to body fat distribution: a dose-response study. Obes Res 1996; 4: 277–282.
Marin P, Darin N, Amemiya T, Andersson B, Jern S, Bjorntorp P . Cortisol secretion in relation to body fat distribution in obese premenopausal women. Metabolism 1992; 41: 882–886.
Pasquali R, Cantobelli S, Casimirri F, Capelli M, Bortoluzzi L, Flamia R et al. The hypothalamic–pituitary–adrenal axis in obese women with different patterns of body fat distribution. J Clin Endocrinol Metab 1993; 77: 341–346.
Duclos M, Gatta B, Corcuff JB, Rashedi M, Pehourcq F, Roger P . Fat distribution in obese women is associated with subtle alterations of the hypothalamic–pituitary–adrenal axis activity and sensitivity to glucocorticoids. Clin Endocrinol (Oxf) 2001; 55: 447–454.
Duclos M, Marquez Pereira P, Barat P, Gatta B, Roger P . Increased cortisol bioavailability, abdominal obesity, and the metabolic syndrome in obese women. Obes Res 2005; 13: 1157–1166.
Steptoe A, Kunz-Ebrecht SR, Brydon L, Wardle J . Central adiposity and cortisol responses to waking in middle-aged men and women. Int J Obes Relat Metab Disord 2004; 28: 1168–1173.
Stewart PM, Boulton A, Kumar S, Clark PM, Shackleton CH . Cortisol metabolism in human obesity: impaired cortisone–cortisol conversion in subjects with central adiposity. J Clin Endocrinol Metab 1999; 84: 1022–1027.
Phillips DI, Barker DJ, Fall CH, Seckl JR, Whorwood CB, Wood PJ et al. Elevated plasma cortisol concentrations: a link between low birth weight and the insulin resistance syndrome? J Clin Endocrinol Metab 1998; 83: 757–760.
Reynolds RM, Labad J, Strachan MW, Braun A, Fowkes FG, Lee AJ et al. Elevated fasting plasma cortisol is associated with ischemic heart disease and its risk factors in people with type 2 diabetes: the Edinburgh type 2 diabetes study. J Clin Endocrinol Metab 2010; 95: 1602–1608.
Stolk RP, Lamberts SW, de Jong FH, Pols HA, Grobbee DE . Gender differences in the associations between cortisol and insulin in healthy subjects. J Endocrinol 1996; 149: 313–318.
Abraham SB, Rubino D, Sinaii N, Ramsey S, Nieman LK . Cortisol, obesity, and the metabolic syndrome: a cross-sectional study of obese subjects and review of the literature. Obesity (Silver Spring) 2013; 21: E105–E117.
Wester VL, Lamberts SW, van Rossum EF . Advances in the assessment of cortisol exposure and sensitivity. Curr Opin Endocrinol Diabetes Obes 2014; 21: 306–311.
Sauve B, Koren G, Walsh G, Tokmakejian S, Van Uum SH . Measurement of cortisol in human hair as a biomarker of systemic exposure. Clin Invest Med 2007; 30: E183–E191.
Manenschijn L, Koper JW, Lamberts SW, van Rossum EF . Evaluation of a method to measure long term cortisol levels. Steroids 2011; 76: 1032–1036.
Perogamvros I, Keevil BG, Ray DW, Trainer PJ . Salivary cortisone is a potential biomarker for serum free cortisol. J Clin Endocrinol Metab 2010; 95: 4951–4958.
Stalder T, Kirschbaum C, Alexander N, Bornstein SR, Gao W, Miller R et al. Cortisol in hair and the metabolic syndrome. J Clin Endocrinol Metab 2013; 98: 2573–2580.
Manenschijn L, van Kruysbergen RG, de Jong FH, Koper JW, van Rossum EF . Shift work at young age is associated with elevated long-term cortisol levels and body mass index. J Clin Endocrinol Metab 2011; 96: E1862–E1865.
Chan J, Sauve B, Tokmakejian S, Koren G, Van Uum S . Measurement of cortisol and testosterone in hair of obese and non-obese human subjects. Exp Clin Endocrinol Diabetes. 2014; 122: 356–362.
Noppe G, Van Rossum EFC, Koper JW, Manenschijn L, Bruining GJ, de Rijke YB et al. Validation and reference ranges of hair cortisol measurement in healthy children. Horm Res Paediat 2014; 82: 97–102.
Veldhorst MAB, Noppe G, Jongejan MHTM, Kok CBM, Mekic S, Koper JW et al. Increased scalp hair cortisol concentrations in obese children. J Clin Endocr Metab 2014; 99: 285–290.
Wester VL, Staufenbiel SM, Veldhorst MA, Visser JA, Manenschijn L, Koper JW et al. Long-term cortisol levels measured in scalp hair of obese patients. Obesity (Silver Spring) 2014; 22: 1956–1958.
Manenschijn L, Schaap L, van Schoor NM, van der Pas S, Peeters GM, Lips P et al. High long-term cortisol levels, measured in scalp hair, are associated with a history of cardiovascular disease. J Clin Endocrinol Metab 2013; 98: 2078–2083.
van Rossum EF, Koper JW, Huizenga NA, Uitterlinden AG, Janssen JA, Brinkmann AO et al. A polymorphism in the glucocorticoid receptor gene, which decreases sensitivity to glucocorticoids in vivo, is associated with low insulin and cholesterol levels. Diabetes 2002; 51: 3128–3134.
van Rossum EF, Voorhoeve PG, te Velde SJ, Koper JW, Delemarre-van de Waal HA, Kemper HC et al. The ER22/23EK polymorphism in the glucocorticoid receptor gene is associated with a beneficial body composition and muscle strength in young adults. J Clin Endocrinol Metab. 2004; 89: 4004–4009.
Huizenga NA, Koper JW, De Lange P, Pols HA, Stolk RP, Burger H et al. A polymorphism in the glucocorticoid receptor gene may be associated with and increased sensitivity to glucocorticoids in vivo. J Clin Endocrinol Metab 1998; 83: 144–151.
Dobson MG, Redfern CP, Unwin N, Weaver JU . The N363S polymorphism of the glucocorticoid receptor: potential contribution to central obesity in men and lack of association with other risk factors for coronary heart disease and diabetes mellitus. J Clin Endocrinol Metab 2001; 86: 2270–2274.
Roussel R, Reis AF, Dubois-Laforgue D, Bellanne-Chantelot C, Timsit J, Velho G . The N363S polymorphism in the glucocorticoid receptor gene is associated with overweight in subjects with type 2 diabetes mellitus. Clin Endocrinol (Oxf) 2003; 59: 237–241.
Kruithof CJ, Kooijman MN, van Duijn CM, Franco OH, de Jongste JC, Klaver CC et al. The Generation R Study: Biobank update 2015. Eur J Epidemiol 2014; 29: 911–927.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. Brit Med J 2000; 320: 1240–1243.
Noppe G, de Rijke YB, Dorst K, van den Akker EL, van Rossum EF . LC-MS/MS-based method for long-term steroid profiling in human scalp hair. Clin Endocrinol (Oxf) 2015; 83: 162–166.
Geelhoed MJ, Steegers EA, Koper JW, van Rossum EF, Moll HA, Raat H et al. Glucocorticoid receptor gene polymorphisms do not affect growth in fetal and early postnatal life. The Generation R Study. BMC Med Genet 2010; 11: 39.
R Core Team, R Foundation for Statistical Computing. R: a language and environment for statistical computing. Available at: http://www.R-projectorg/. 2013.
Van Buuren S, Groothuis-Oudshoorn CGM . Mice: multivariate Imputation by chained equations in R. J Stat Softw 2011; 45: 1–67.
Medina-Gomez C, Felix JF, Estrada K, Peters MJ, Herrera L, Kruithof CJ et al. Challenges in conducting genome-wide association studies in highly admixed multi-ethnic populations: the generation R Study. Eur J Epidemiol 2015; 30: 317–330.
Wester VL, Staufenbiel SM, Veldhorst MAB, Visser JA, Manenschijn L, Koper JW et al. Long-term cortisol levels measured in scalp hair of obese patients. Obesity 2014; 22: 1956–1958.
Geelen CC, van Greevenbroek MM, van Rossum EF, Schaper NC, Nijpels G, t Hart LM et al. BclI glucocorticoid receptor polymorphism is associated with greater body fatness: the Hoorn and CODAM studies. J Clin Endocrinol Metab 2013; 98: E595–E599.
Barat P, Corcuff JB, Tauber M, Moisan MP . Associations of glucocorticoid receptor and corticosteroid-binding globulin gene polymorphisms on fat mass and fat mass distribution in prepubertal obese children. J Physiol Biochem 2012; 68: 645–650.
Voorhoeve PG, van den Akker EL, van Rossum EF, Koper JW, van Mechelen W, Lamberts SW et al. Glucocorticoid receptor gene variant is associated with increased body fatness in youngsters. Clin Endocrinol (Oxf) 2009; 71: 518–523.
Manenschijn L, van den Akker EL, Ester WA, Leunissen RW, Willemsen RH, van Rossum EF et al. Glucocorticoid receptor gene haplotypes are not associated with birth anthropometry, blood pressure, glucose and insulin concentrations, and body composition in subjects born small for gestational age. Eur J Endocrinol 2010; 163: 911–918.
Berardelli R, Karamouzis I, D'Angelo V, Zichi C, Fussotto B, Giordano R et al. Role of mineralocorticoid receptors on the hypothalamus–pituitary–adrenal axis in humans. Endocrine 2013; 43: 51–58.
Harris AP, Holmes MC, de Kloet ER, Chapman KE, Seckl JR . Mineralocorticoid and glucocorticoid receptor balance in control of HPA axis and behaviour. Psychoneuroendocrinology 2013; 38: 648–658.
Gishti O, Gaillard R, Durmus B, Abrahamse M, van der Beek EM, Hofman A et al. Body mass index, total and abdominal fat distribution and cardiovascular risk factors in school-age children. Pediatr Res 2015; 77: 710–718.
Handelsman DJ, Wartofsky L . Requirement for mass spectrometry sex steroid assays in the Journal of Clinical Endocrinology and Metabolism. J Clin Endocrinol Metab 2013; 98: 3971–3973.
Fardet L, Feve B . Systemic glucocorticoid therapy: a review of its metabolic and cardiovascular adverse events. Drugs 2014; 74: 1731–1745.
Acknowledgements
We are grateful for the financial support by the Thrasher Research Fund (Grant TRF-11643), which enabled this research project. The general design of Generation R Study is made possible by financial support from the Erasmus Medical Center, Rotterdam, the Erasmus University Rotterdam, the Netherlands Organization for Health Research and Development (ZonMw), the Netherlands Organisation for Scientific Research (NWO), the Ministry of Health, Welfare and Sport and the Ministry of Youth and Families. Vincent Jaddoe received an additional grant from the Netherlands Organisation for Scientific Research (NWO, ZonMW-VIDI). Elisabeth van Rossum is additionally supported by a grant of the Netherlands Brain Foundation (F2011(1)-12) and an Erasmus MC Fellowship. The analytical support of Mrs. Kristien Dorst has been greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Noppe, G., van den Akker, E., de Rijke, Y. et al. Long-term glucocorticoid concentrations as a risk factor for childhood obesity and adverse body-fat distribution. Int J Obes 40, 1503–1509 (2016). https://doi.org/10.1038/ijo.2016.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.113
This article is cited by
-
Differences in segmental hair cortisol concentration analysis among children and adolescents with overweight and obesity, their parents, and normal weight peers
Hormones (2023)
-
Effects of a novel mobile health intervention compared to a multi-component behaviour changing program on body mass index, physical capacities and stress parameters in adolescents with obesity: a randomized controlled trial
BMC Pediatrics (2021)
-
Environmental mismatch and obesity in humans: The Jerusalem Perinatal Family Follow-Up Study
International Journal of Obesity (2021)
-
Ipercortisolismo funzionale e sue possibili conseguenze cliniche
L'Endocrinologo (2021)
-
Hair cortisol-a method to detect chronic cortisol levels in patients with Prader-Willi syndrome
BMC Endocrine Disorders (2020)