Abstract
Background
Cushing Disease (CD) is a rare endocrine disorder associated with impaired growth hormone (GH) and short stature. Insulin-like growth factor-1 (IGF-1) is a marker of GH secretion.
Methods
Patients with young onset CD (<21 years old) and available IGF-1 levels at diagnosis and/or follow-up were studied (total = 194, diagnosis = 174, follow-up = 104). IGF-1 was reported as z-score (IGF1z).
Results
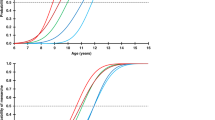
IGF1z was lower than expected in the general population (median IGF1z: −0.92 [−1.54, 0.07], p < 0.0001) at diagnosis and remained low at follow-up (median: −1.13 [−1.78, −0.66], p < 0.0001). There was no correlation of IGF1z at diagnosis with BMI; there was a weak correlation with height (rs = 0.19, p = 0.035). IGF1z was inversely correlated with markers of hypercortisolemia, including morning (rs = −0.31, p < 0.0001) and midnight cortisol (rs = −0.30, p < 0.0001), and with insulin resistance (Homeostatic Model Assessment for Insulin Resistance, HOMA-IR, rs = −0.27, p < 0.01).
Conclusions
IGF-1 levels in CS are on the lower side of the normal range during active disease and remain low at one year after treatment. IGF-1 levels correlated mainly with markers of hypercortisolemia rather than the short stature of patients and should not be used in the assessment of growth in this population.
Impact
-
We report that IGF-1 levels in childhood during active hypercortisolemia and up to 1 year after resolution are on the lower side of the normal range.
-
Our results demonstrate that IGF-1 levels during active hypercortisolemia correlate mainly with markers of Cushing syndrome.
-
This report adds data to the current literature where reports of IGF-1 in Cushing syndrome have shown variable results.
-
Understanding the lack of utility of IGF-1 in assessing growth parameters in the pediatric Cushing syndrome population is important for physicians caring for these patients who should not use IGF-1 for diagnostic or treatment decisions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Some datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request if patient confidentiality is preserved.
References
Tatsi, C. & Stratakis, C. A. Pediatric Cushing syndrome; an overview. Pediatr. Endocrinol. Rev. 17, 100–109 (2019).
Vandewalle, J., Luypaert, A., De Bosscher, K. & Libert, C. Therapeutic mechanisms of glucocorticoids. Trends Endocrinol. Metab. 29, 42–54 (2018).
Lodish, M. B., Keil, M. F. & Stratakis, C. A. Cushing’s syndrome in pediatrics: an update. Endocrinol. Metab. Clin. North Am. 47, 451–462 (2018).
Keil, M. F., Graf, J., Gokarn, N. & Stratakis, C. A. Anthropometric measures and fasting insulin levels in children before and after cure of Cushing syndrome. Clin. Nutr. 31, 359–363 (2012).
Magiakou, M. A., Mastorakos, G., Gomez, M. T., Rose, S. R. & Chrousos, G. P. Suppressed spontaneous and stimulated growth hormone secretion in patients with Cushing’s disease before and after surgical cure. J. Clin. Endocrinol. Metab. 78, 131–137 (1994).
Procopio, M. et al. GH response to GHRH combined with pyridostigmine or arginine in different conditions of low somatotrope secretion in adulthood: obesity and Cushing’s syndrome in comparison with hypopituitarism. Minerva Endocrinol. 24, 107–111 (1999).
Tzanela, M., Karavitaki, N., Stylianidou, C., Tsagarakis, S. & Thalassinos, N. C. Assessment of GH reserve before and after successful treatment of adult patients with Cushing’s syndrome. Clin. Endocrinol. (Oxf.) 60, 309–314 (2004).
English, K., Chikani, V., Dimeski, G. & Inder, W. J. Elevated insulin-like growth factor-1 in Cushing’s disease. Clin. Endocrinol. (Oxf.) 91, 141–147 (2019).
Clemmons, D. R. Metabolic actions of insulin-like growth factor-I in normal physiology and diabetes. Endocrinol. Metab. Clin. North Am. 41, 425–443 (2012). vii-viii.
Greulich, W. & Pyle, S. Radiographic Atlas of Skeletal Development of the Hand and Wrist 2nd edn, (Stanford University Press, 1959).
Bayley, N. & Pinneau, S. R. Tables for predicting adult height from skeletal age: revised for use with the Greulich-Pyle hand standards. J. Pediatr. 40, 423–441 (1952).
Breen, K. M. & Karsch, F. J. New insights regarding glucocorticoids, stress and gonadotropin suppression. Front Neuroendocrinol. 27, 233–245 (2006).
Miller, W. L. The hypothalamic-pituitary-adrenal axis: a brief history. Horm. Res. Paediatr. 89, 212–223 (2018).
Wajchenberg, B. L. et al. Growth hormone axis in Cushing’s syndrome. Horm. Res. 45, 99–107 (1996).
Acknowledgements
This study was funded by the intramural research program of the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), National Institutes of Health (NIH), Bethesda, MD 20892, USA.
Author information
Authors and Affiliations
Contributions
C.T., J.W. : conception, design, data collection, analysis, and interpretation. M.V., and M.K.: collection the data. C.A.S.: critical revision of the study. All the authors contributed to the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
Dr. Stratakis holds patents on the function of the PRKAR1A, PED11A, and GPR101 genes and related issues; his laboratory has also received research funding on the GPR101 gene, and on abnormal growth hormone secretion and its treatment by Pfizer, Inc. He is currently employed by ELPEN, SA and has been consulting for Lundbeck Pharmaceuticals and Sync, SA. Dr. Tatsi received funding by Pfizer, Inc., for unrelated studies.
Consent statement
All study procedures were approved by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) Institutional Review Board. Consent was obtained from participants and/or their parent or legal guardian to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weinberg, J.R., Voudouri, M., Keil, M. et al. The utility of IGF1 in the evaluation of pediatric patients with endogenous hypercortisolemia. Pediatr Res 95, 758–761 (2024). https://doi.org/10.1038/s41390-023-02906-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02906-6