Abstract
Background:
Lack of sleep and increased consumption of energy-dense foods and sugar-sweetened beverages (SSBs) have all been suggested as factors contributing to the increased prevalence of overweight and obesity.
Objective:
To evaluate whether objectively measured sleep duration (average and day-to-day variability) as well as parent-reported sleep problems are independently associated with proposed dietary risk factors for overweight and obesity in 8–11-year-old children.
Design:
In this cross-sectional study, data on sleep duration and day-to-day variability in sleep duration were measured in 676 Danish, apparently healthy children by an objective measure (actigraphy) for 8 nights, and the Children’s Sleep Habits Questionnaire (CSHQ) was filled out by the parents. Diet was recorded using a web-based food record for 7 consecutive days. Fasting blood samples were obtained for measurements of plasma leptin and ghrelin levels.
Results:
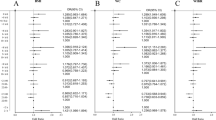
Sleep duration (h per night) was negatively associated with energy density (ED) of the diet (β=−0.32 kJ g−1), added sugar (β=−1.50 E%) and SSBs (β=−1.07 E%) (all P⩽0.003). Furthermore, variability in sleep duration (10-min per night) was positively associated with SSBs (β=0.20 E%, P=0.03), independent of sleep duration, and CSHQ score was positively associated with ED (β=0.16 kJ g−1, P=0.04). All of these associations were independent of potential confounders (age, sex, pubertal status, height, weight, screen time, moderate-to-vigorous physical activity and parental education and ethnicity).
Conclusion:
Our study suggests that short sleep duration, high sleep duration variability and experiencing sleep problems are all associated with a poor, obesity-promoting diet in children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kjøller M, Juel K, Kamper-Jørgensen F . Folkesundhedsrapporten. Statens Institut for Folkesundhed, Syddansk Universitet 2007.
Lakshman R, Elks CE, Ong KK . Childhood obesity. Circulation 2012; 126: 1770–1779.
Matricciani L, Olds T, Petkov J . In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev 2012; 16: 203–211.
Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT . Never enough sleep: a brief history of sleep recommendations for children. Pediatrics 2012; 129: 548–556.
Chaput JP, Lambert M, Gray-Donald K, McGrath JJ, Tremblay MS, O'Loughlin J et al. Short sleep duration is independently associated with overweight and obesity in Quebec children. Can J Public Health 2011; 102: 369–374.
Carter PJ, Taylor BJ, Williams SM, Taylor RW . Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ 2011; 342: d2712.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008; 31: 619–626.
Chahal H, Fung C, Kuhle S, Veugelers PJ . Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatr Obes 2012; 7: 1–10.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141: 846–850.
Spiegel K, Leproult R, L'hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E . Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab 2004; 89: 5762–5771.
Chaput JP, Despres JP, Bouchard C, Tremblay A . Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity (Silver Spring) 2007; 15: 253–261.
Chaput JP, Tremblay A . Insufficient sleep as a contributor to weight gain: an update. Curr Obes Res 2012; 1: 245–256.
Penev PD . Update on energy homeostasis and insufficient sleep. J Clin Endocrinol Metab 2012; 97: 1792–1801.
Klingenberg L, Chaput JP, Holmback U, Jennum P, Astrup A, Sjodin A . Sleep restriction is not associated with a positive energy balance in adolescent boys. Am J Clin Nutr 2012; 96: 240–248.
St-Onge MP, Roberts AL, Chen J, Kelleman M, O'Keeffe M, Roychoudhury A et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am J Clin Nutr 2011; 29: 410–416.
Schmid SM, Hallschmid M, Jauch-Chara K, Wilms B, Benedict C, Lehnert H et al. Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am J Clin Nutr 2009; 90: 1476–1482.
Garaulet M, Ortega FB, Ruiz JR, Rey-Lopez JP, Beghin L, Manios Y et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes (Lond) 2011; 35: 1308–1317.
Westerlund L, Ray C, Roos E . Associations between sleeping habits and food consumption patterns among 10-11-year-old children in Finland. Br J Nutr 2009; 102: 1531–1537.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S . The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep 2010; 33: 1201–1209.
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD . Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr 2009; 89: 126–133.
Hogenkamp PS, Nilsson E, Nilsson VC, Chapman CD, Vogel H, Lundberg LS et al. Acute sleep deprivation increases portion size and affects food choice in young men. Psychoneuroendocrinology 2013. e-pub ahead of print 18 February 2013 doi:10.1016/j.psyneuen.2013.01.012.
Benedict C, Brooks SJ, O'Daly OG, Almen MS, Morell A, Aberg K et al. Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: an fMRI study. J Clin Endocrinol Metab 2012; 97: E443–E447.
St-Onge MP, McReynolds A, Trivedi ZB, Roberts AL, Sy M, Hirsch J . Sleep restriction leads to increased activation of brain regions sensitive to food stimuli. Am J Clin Nutr 2012; 95: 818–824.
WHO. Diet, nutrition and the prevention of chronic diseases Report of a Joint WHO/FAO Consultation. WHO Technical Report Series 916 2003.
Thorleifsdottir B, Bjornsson JK, Benediktsdottir B, Gislason T, Kristbjarnarson H . Sleep and sleep habits from childhood to young adulthood over a 10-year period. J Psychosom Res 2002; 53: 529–537.
Kim CW, Choi MK, Im HJ, Kim OH, Lee HJ, Song J et al. Weekend catch-up sleep is associated with decreased risk of being overweight among fifth-grade students with short sleep duration. J Sleep Res 2012; 12: 546–551.
Golley RK, Maher CA, Matricciani L, Olds TS . Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond) 2013; 37: 546–551.
Fleig D, Randler C . Association between chronotype and diet in adolescents based on food logs. Eat Behav 2009; 10: 115–118.
Damsgaard CT, Dalskov SM, Petersen RA, Sorensen LB, Molgaard C, Biltoft-Jensen A et al. Design of the OPUS School Meal Study: a randomised controlled trial assessing the impact of serving school meals based on the New Nordic Diet. Scand J Public Health 2012; 29: 1–11.
Black AE . The sensitivity and specificity of the Goldberg cut-off for EI:BMR for identifying diet reports of poor validity. Eur J Clin Nutr 2000; 54: 395–404.
Morris NM, Udry KR . Validation of a self-administered instrument to assess stage of adolescent development. J Youth Adolesc 1980; 9: 271–280.
Owens JA, Spirito A, McGuinn M . The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 2000; 23: 1043–1051.
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA . Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011; 43: 1360–1368.
Sadeh A, Sharkey KM, Carskadon MA . Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep 1994; 17: 201–207.
Biltoft-Jensen A, Bysted A, Trolle E, Christensen T, Knuthsen P, Damsgaard CT et al. Evaluation of Web-based Dietary Assessment Software for Children: comparing reported fruit, juice and vegetable intakes with plasma carotenoid concentration and school lunch observations. Br J Nutr 2012; 27: 1–10.
Biltoft-Jensen A, Trolle E, Christensen T, Islam N, Andersen LF, Egenfeldt-Nielsen S et al. WebDASC: a web-based dietary assessment software for 8-11-year-old Danish children. J Hum Nutr Diet 2012; 18: 1–11.
Henry CJ . Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr 2005; 8: 1133–1152.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660.
Cole TJ, Flegal KM, Nicholls D, Jackson AA . Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 2007; 335: 194.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Chaput JP, Klingenberg L, Sjodin A . Do all sedentary activities lead to weight gain: sleep does not. Curr Opin Clin Nutr Metab Care 2010; 13: 601–607.
Chaput JP, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr 2011; 93: 1196–1203.
Robinson TN . Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA 1999; 282: 1561–1567.
Park S, Blanck HM, Sherry B, Brener N, O'Toole T . Factors associated with sugar-sweetened beverage intake among United States high school students. J Nutr 2012; 142: 306–312.
Van den Bulck J, Van Mierlo J . Energy intake associated with television viewing in adolescents, a cross sectional study. Appetite 2004; 43: 181–184.
Hasler BP, Dahl RE, Holm SM, Jakubcak JL, Ryan ND, Silk JS et al. Weekend-weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biol Psychol 2012; 91: 334–341.
Holm SM, Forbes EE, Ryan ND, Phillips ML, Tarr JA, Dahl RE . Reward-related brain function and sleep in pre/early pubertal and mid/late pubertal adolescents. J Adolesc Health 2009; 45: 326–334.
Lutter M, Nestler EJ . Homeostatic and hedonic signals interact in the regulation of food intake. J Nutr 2009; 139: 629–632.
Crispim CA, Zimberg IZ, dos Reis BG, Diniz RM, Tufik S, de Mello MT . Relationship between food intake and sleep pattern in healthy individuals. J Clin Sleep Med 2011; 7: 659–664.
Herzog N, Friedrich A, Fujita N, Gais S, Jauch-Chara K, Oltmanns KM et al. Effects of daytime food intake on memory consolidation during sleep or sleep deprivation. PLoS One 2012; 7: e40298.
Pollak CP, Bright D . Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics 2003; 111: 42–46.
Reedy J, Krebs-Smith SM . Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc 2010; 110: 1477–1484.
de Ruyter JC, Olthof MR, Seidell JC, Katan MB . A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med 2012; 367: 1397–1406.
Hansen TK, Dall R, Hosoda H, Kojima M, Kangawa K, Christiansen JS et al. Weight loss increases circulating levels of ghrelin in human obesity. Clin Endocrinol (Oxf) 2002; 56: 203–206.
Cummings DE, Foster-Schubert KE, Overduin J . Ghrelin and energy balance: focus on current controversies. Curr Drug Targets 2005; 6: 153–169.
Williams DL, Cummings DE . Regulation of ghrelin in physiologic and pathophysiologic states. J Nutr 2005; 135: 1320–1325.
Hjorth MF, Chaput JP, Damsgaard CT, Dalskov S, Michaelsen KF, Tetens I et al. Measure of sleep and physical activity by a single accelerometer: can a waist-worn Actigraph adequately measure sleep in children? Sleep Biol Rhythms 2012; 10: 328–335.
Acknowledgements
The study is part of the OPUS project ‘Optimal well-being, development and health for Danish children through a healthy New Nordic Diet’ supported by a grant from the Nordea Foundation. We are grateful to the participants and would also like to acknowledge the school staffs as well as other researchers and staff in the OPUS project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Designed research: AA, KFM, IT, J-PC and AS; coordinated data collection: MFH and RA; analyzed and interpreted data: JSK and MFH; discussed the analysis and interpretation of the data: AS and J-PC; wrote paper: JSK and MFH; had primary responsibility of the final content: AS. All authors reviewed the manuscript critically and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Kjeldsen, J., Hjorth, M., Andersen, R. et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int J Obes 38, 32–39 (2014). https://doi.org/10.1038/ijo.2013.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.147
Keywords
This article is cited by
-
Shorter sleep among adolescents is associated with lower fruit and vegetable consumption the following day
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
The impact of dietary and sleep rhythms on blood pressure in children and adolescents: a cross-sectional study
Hypertension Research (2023)
-
Weekdays’ sleeping condition and its influence on occurrence of general malaise in Japanese children aged 10 to 12 years
Sleep and Biological Rhythms (2023)
-
Association of healthy beverage index with circadian rhythm and quality of sleep among overweight and obese women: a cross-sectional study
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)
-
Effects of an intensive lifestyle intervention and the role of sleep in people living with HIV and prediabetes: a pilot and feasibility study
BMC Research Notes (2021)