Abstract
Objective:
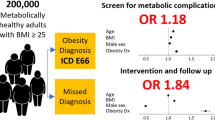
To examine the relationship between body mass index (BMI) and metabolic syndrome for Asian Americans and non-Hispanic Whites (NHWs), given that existing evidence shows racial/ethnic heterogeneity exists in how BMI predicts metabolic syndrome.
Research Design and Methods:
Electronic health records of 43 507 primary care patients aged 35 years and older with self-identified race/ethnicity of interest (Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese or NHW) were analyzed in a mixed-payer, outpatient-focused health-care organization in the San Francisco Bay Area.
Results:
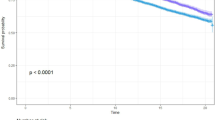
Metabolic syndrome prevalence is significantly higher in Asians compared with NHWs for every BMI category. For women at the mean age of 55 and BMI of 25 kg m–2, the predicted prevalence of metabolic syndrome is 12% for NHW women compared with 30% for Asians; similarly for men, the predicted prevalence of metabolic syndrome is 22% for NHWs compared with 43% of Asians. Compared with NHW women and men with a BMI of 25 kg m–2, comparable prevalence of metabolic syndrome was observed at BMI of 19.6 kg m–2 for Asian women and 19.9 kg m–2 for Asian men. A similar pattern was observed in disaggregated Asian subgroups.
Conclusions:
In spite of the lower BMI values and lower prevalence of overweight/obesity than NHWs, Asian Americans have higher rates of metabolic syndrome over the range of BMI. Our results indicate that BMI ranges for defining overweight/obesity in Asian populations should be lower than for NHWs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683–689.
Laaksonen DE, Lakka H-M, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA . Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 2002; 156: 1070–1077.
National Cholesterol Education Program (NCEP). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Final Report National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health (NIH) 2002.
Alexander CM, Landsman PB, Teutsch SM, Haffner SM . NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 2003; 52: 1210–1214.
Han TS, Williams K, Sattar N, Hunt KJ, Lean ME, Haffner SM . Analysis of obesity and hyperinsulinemia in the development of metabolic syndrome: San Antonio Heart Study. Obes Res 2002; 10: 923–931.
Palaniappan L, Carnethon MR, Wang Y, Hanley AJG, Fortmann SP, Haffner SM et al. Predictors of the incident metabolic syndrome in adults. Diabetes Care 2004; 27: 788–793.
Centers for Disease Control and Prevention (CDC). Defining Overweight and Obesity Overweight and Obesity. Department of Health and Human Services: Atlanta, GA, 2009.
Carnethon MR, Palaniappan LP, Burchfiel CM, Brancati FL, Fortmann SP . Serum insulin, obesity, and the incidence of type 2 diabetes in black and white adults: the atherosclerosis risk in communities study: 1987-1998. Diabetes Care 2002; 25: 1358–1364.
Palaniappan LP, Carnethon MR, Fortmann SP . Heterogeneity in the relationship between ethnicity, BMI, and fasting insulin. Diabetes Care 2002; 25: 1351–1357.
Haffner SM, Bowsher RR, Mykkanen L, Hazuda HP, Mitchell BD, Valdez RA et al. Proinsulin and specific insulin concentration in high- and low-risk populations for NIDDM (non-insulin-dependent diabetes mellitus). Diabetes 1994; v43: p1490–p1494.
Jee SH, Sull JW, Park J, Lee S-Y, Ohrr H, Guallar E et al. Body-mass index and mortality in Korean men and women. N Engl J Med 2006; 355: 779–787.
Lee W-Y, Park J-S, Noh S-Y, Rhee E-J, Kim S-W, Zimmet PZ . Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Res Clin Pract 2004; 65: 143–149.
Deurenberg-Yap M, Chew SK, Lin VF, Tan BY, van Staveren WA, Deurenberg P . Relationships between indices of obesity and its co-morbidities in multi-ethnic Singapore. Int J Obes Relat Metab Disord 2001; 25: 1554–1562.
Kim SM, Kim KM, Choi HJ, Yoon SJ, Lee DJ . A study on the obesity index of health examination center data. J Korean Soc Stud Obes 1997; 6: 137–142.
Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P . The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord 2000; 24: 1011–1017.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y . Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000; 72: 694–701.
He M, Tan KC, Li ET, Kung AW . Body fat determination by dual energy X-ray absorptiometry and its relation to body mass index and waist circumference in Hong Kong Chinese. Int J Obes Relat Metab Disord 2001; 25: 748–752.
Ko GT, Chan JC, Cockram CS, Woo J . Prediction of hypertension, diabetes, dyslipidaemia or albuminuria using simple anthropometric indexes in Hong Kong Chinese. Int J Obes Relat Metab Disord 1999; 23: 1136–1142.
Yajnik CS . The lifecycle effects of nutrition and body size on adult adiposity, diabetes and cardiovascular disease. Obes Rev 2002; 3: 217–224.
Zhou BF . Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002; 15: 83–96.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163.
Palaniappan LP, Wong EC, Shin JS, Moreno MR, Otero-Sabogal R . Collecting patient race/ethnicity and primary language data in ambulatory care settings: a case study in methodology. Health Serv Res 2009; 44: 1750–1761.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763–778.
Flegal KM, Graubard BI, Williamson DF, Gail MH . Excess deaths associated with underweight, overweight, and obesity. JAMA 2005; 293: 1861–1867.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE et al. Body weight and mortality among women. N Engl J Med 1995; 333: 677–685.
Deurenberg P, Deurenberg-Yap M . Validity of body composition methods across ethnic population groups. Forum Nutr 2003; 56: 299–301.
Deurenberg P, Ge K, Hautvast JGAJ, Wang J . Body mass index as predictor for body fat: comparison between Chinese and Dutch adult subjects. Asia Pac J Clin Nutr 1997; 6: 102–105.
Wang J, Thornton JC, Bari S, Williamson B, Gallagher D, Heymsfield SB et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr 2003; 77: 379–384.
Kagawa M, Byrne NM, Hills AP . Comparison of body fat estimation using waist:height ratio using different waist measurements in Australian adults. Br J Nutr 2008; 100: 1135–1141.
Rudolf MCJ, Walker J, Cole TJ . What is the best way to measure waist circumference? Int J Pediatr Obes 2007; 2: 58–61.
Kiernan M, Winkleby MA . Identifying patients for weight-loss treatment: an empirical evaluation of the NHLBI obesity education initiative expert panel treatment recommendations. Arch Intern Med 2000; 160: 2169–2176.
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB . How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996; 143: 228–239.
Norgan NG . Interpretation of low body mass indices: Australian aborigines. Am J Phys Anthropol 1994; 94: 229–237.
Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB . Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatr 1998; 132: 204–210.
Clinical Guidelines on the Identification Evaluation Treatment of Overweight Obesity in Adults—The Evidence Report. National Institutes of Health. Obes Res 1998; 6 (Suppl 2): 51S–209S.
Obesity: preventing managing the global epidemic Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: i–xii, 1-253.
Haffner SM, D’Agostino R, Saad MF, Rewers M, Mykkanen L, Selby J et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes 1996; 45: 742–748.
Haffner SM, Miettinen H, Gaskill SP, Stern MP . Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes 1995; 44: 1386–1391.
Haffner SM, Stern MP, Hazuda HP, Mitchell BD, Patterson JK . Cardiovascular risk factors in confirmed prediabetic individuals. Does the clock for coronary heart disease start ticking before the onset of clinical diabetes? JAMA 1990; 263: 2893–2898.
Alberti KGMM, Zimmet P, Shaw J . The metabolic syndrome—a new worldwide definition. The Lancet 366: 1059–1062.
US Census Bureau 2006 American Community Survey: Summary File 2, PCT5.
Tang PC, Ralston M, Arrigotti MF, Qureshi L, Graham J . Comparison of methodologies for calculating quality measures based on administrative data versus clinical data from an electronic health record system: implications for performance measures. J Am Med Inform Assoc 2007; 14: 10–15.
Acknowledgements
This study is supported by the American Heart Association 0885049N: Asian American Heart Study; and NIDDK/NIH 1 R01 DK081371-01A1 (identifying disparities in type 2 diabetes among Asian Americans: The Pan Asian Cohort Study).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The study was presented as an abstract at the American Heart Association Joint Conference for Cardiovascular Disease Epidemiology and Prevention and Nutrition, Physical Activity and Metabolism, 10–14 March 2009.
Disclaimer
All research conducted for this study was approved by the Palo Alto Medical Foundation Institutional Review Board. This material has not been published previously (either in print or electronically) and is not under consideration for publication elsewhere.
Rights and permissions
About this article
Cite this article
Palaniappan, L., Wong, E., Shin, J. et al. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes 35, 393–400 (2011). https://doi.org/10.1038/ijo.2010.152
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.152
Keywords
This article is cited by
-
Risk of Sleep Apnea Is Associated with Abdominal Obesity Among Asian Americans: Comparing Waist-to-Hip Ratio and Body Mass Index
Journal of Racial and Ethnic Health Disparities (2024)
-
Cardiovascular Risk Factors Among Asian Americans: Perspectives on the Role of Acculturation in Cardiovascular Diseases Health Disparities
Journal of Immigrant and Minority Health (2023)
-
Infant Body Composition in an Asian Pacific Islander Population
Journal of Racial and Ethnic Health Disparities (2023)
-
Impact of pre-pregnancy body mass index and gestational weight gain on the risk of maternal and infant pregnancy complications in Korean women
International Journal of Obesity (2022)
-
Novel and traditional anthropometric indices for identifying metabolic syndrome in non-overweight/obese adults
Nutrition & Metabolism (2021)