Abstract
Therapeutic human papillomavirus (HPV) vaccines have the potential to inhibit the progression of an established HPV infection to precancer and cancer lesions by targeting HPV oncoproteins. We have previously developed a therapeutic DNA vaccine encoding calreticulin (CRT) linked to E7, CRT/E7 DNA vaccine, for use in the treatment of HPV-associated lesions. Since the transfection efficiency of DNA vaccines administered in vivo is typically low, we examined the use of electroporation as well as different routes of administration to enhance antigen-specific tumor control. We tested the effects of the CRT/E7 DNA vaccine administered intramuscularly or intravaginally, with or without electroporation, on the generation of CD8+ T-cell immunity and therapeutic antitumor effects in HPV16 E7-expressing cervicovaginal tumor-bearing mice. We found that intravaginal vaccination of CRT/E7 DNA followed by electroporation-induced potent E7-specific CD8+ T-cell responses in the cervicovaginal tract, compared with intramuscular injection followed by electroporation. Furthermore, tumor-bearing mice vaccinated intravaginally followed by electroporation had an enhanced survival, antitumor effects and local production of IFN-γ+CD8+ T cells compared with those vaccinated intramuscularly with electroporation. Thus, we show that intravaginal CRT/E7 DNA vaccination followed by electroporation generates the most potent therapeutic antitumor effects against an orthotopic E7-expressing tumor model. The current study will have significant clinical implications once a clinically applicable electroporation device for intravaginal use becomes available.
Similar content being viewed by others
Introduction
Human papillomaviruses (HPVs) are the primary etiologic agents of cervical cancer,1 and cervical cancer is the third most common female cancer worldwide.2 The identification of HPV as the etiologic factor for cervical cancer creates an opportunity for developing therapeutic HPV vaccines in order to inhibit the progression of established HPV infection toward HPV-precancer and cancer lesions (for review see3, 4, 5). The two HPV viral oncoproteins, E6 and E7, are required for the induction and maintenance of cellular transformation, and are consistently co-expressed in HPV-associated cancers.6, 7 Thus, they represent ideal targets for the development of a therapeutic HPV vaccine.
We have previously employed a therapeutic DNA vaccine targeting E7 for use in HPV-associated disease. This vaccine, pcDNA3-CRT/E7, encodes calreticulin (CRT), linked to E7 and has been shown to enhance antigen-specific CD8+ T-cell-mediated immune responses in a preclinical model.8, 9 Although the CRT/E7 DNA vaccine elicited potent antigen-specific antitumor effects against E7-expressing TC-1 tumors in mice, DNA vaccines typically suffer from low transfection efficiency. Therefore, an improved administration strategy for CRT/E7 DNA vaccination is an attractive immunotherapeutic approach for an enhanced antigen-specific tumor control.
Electroporation, used immediately following a DNA vaccine injection, transiently increases the permeability of the plasma membrane by an electrical current, which allow increased uptake of the DNA plasmid.10 Previously, we have shown that intramuscular DNA vaccine administration followed by electroporation elicits the strongest CD8+ T-cell immune responses compared with intramuscular injection alone, or to delivery by a gene gun.10 Thus, electroporation is an ideal strategy to enhance the efficacy of the CRT/E7 DNA vaccine.
Another important consideration regarding the delivery of a therapeutic vaccine is the route of administration, which can have an effect on the location in which the most potent cell-mediated immune responses are generated. It has been shown that the generation of an antitumor response at the location of the tumor, compared with a systemic immune response in the blood, is important for tumor regression.11 Local immune responses at the lesion site have been associated with disease clearance, suggesting the importance of both eliciting an HPV immune response and appropriately targeting it to the lesion site.12, 13 Intravaginal (Ivag) immunization with HPV pseudoviruses carrying DNA encoding HPV antigens was found to induce local HPV-specific CD8+ T-cell responses.14 Therefore, the therapeutic effects of CRT/E7 DNA vaccine against HPV-associated cervicovaginal tumors may be enhanced when the vaccine is delivered intravaginally.
In the current study, we examined the effects of a therapeutic HPV DNA vaccine administered through different routes with or without electroporation on the generation of HPV-specific CD8+ T-cell-mediated immunity and therapeutic antitumor effects using an orthotopic HPV16 E7-expressing tumor model. We found that electroporation increased the expression of the protein encoded by DNA construct delivered submucosally in the cervicovaginal tract. Furthermore, we observed that intravaginal vaccination of CRT/E7 DNA followed by electroporation induced significantly more potent E7-specific CD8+ T-cell responses, especially in the cervicovaginal tract, compared with intramuscular injection with or without electroporation. Additionally, orthotopic TC-1 tumor-bearing mice vaccinated intravaginally followed by electroporation demonstrated improved survival and antitumor effects as well as increased local production of IFN-γ+ CD8+ T cells compared with those vaccinated intramuscularly followed by electroporation. Furthermore, we observed that mice vaccinated with CRT/E7 intravaginally with electroporation generated a significantly higher percentage of α4β7+ E7-specific CD8+ T cells in the cervicovaginal tract compared with mice vaccinated intramuscularly with electroporation. Thus, our results indicate that intravaginal vaccination with CRT/E7 DNA followed by electroporation may be a promising way to generate potent therapeutic antitumor effects against in the cervicovaginal tract.
Results
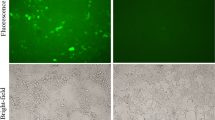
Electroporation increases expression of the protein encoded by DNA construct delivered submucosally in the vaginal tract
We first examined the efficiency of protein expression of a DNA construct delivered by submucosal injection in the cervicovaginal tract with or without electroporation by using C57BL/6 mice and a luciferase-expressing DNA construct. Mice were left untreated or were submucosally injected in the vagina with 20 μg pcDNA3-luciferase followed with or without electroporation. As shown in Figure 1a, after 48 h, the luciferase activity in the mice was measured by IVIS. Mice vaccinated intravaginally followed by electroporation had a significantly greater luciferase activity in the cervicovaginal tract compared with mice that received the vaccination without electroporation (Figure 1b). These data indicate that electroporation can significantly enhance the expression of DNA construct delivered submucosally in the cervicovaginal tract compared with delivery without electroporation.
Electroporation significantly increased the luciferase expression by vaginal tissue after the submucosal injection. pcDNA3-luciferase (20 μg) was submucosally injected into the vagina of 5–8-week-old female C57BL/6 mice with or without subsequent electroporation. After 48 h, the luciferase activity was measured by IVIS. (a) Imaging analysis of vaginal tissue luciferase activity. (b) Graphical summary of vaginal tissue luciferase activity detected by IVIS. **P<0.01.
Potent systemic and local antigen-specific CD8+ T-cell responses are induced by vaginal submucosal vaccination with electroporation
We then examined HPV16 E7-specific CD8+ T-cell immune responses in C57BL/6 mice vaccinated with pcDNA3-CRT/E7 by various routes with or without electroporation. Mice were vaccinated with pcDNA3-CRT/E7 (20 μg) through either intravaginal or intramuscular injection with or without subsequent electroporation. The mice were then boosted with the same regimen 1 week later. Seven days after the last vaccination, splenocytes and cervicovaginal cells were harvested for analysis by flow cytometry. As shown in Figures 2a and b, the number of E7-specific CD8+ T cells among splenocytes was significantly higher in mice receiving electroporation following pcDNA3-CRT/E7 vaccination, compared with those that did not receive electroporation. Figures 2c and d demonstrate that mice vaccinated intravaginally followed by electroporation generated the highest number of E7-specific CD8+ T cells among cervicovaginal cells compared with all other treatment groups. Interestingly, CD8+ cells are rare in the vaginal tissue; only mice vaccinated intravaginally followed by EP generated higher amount of CD8+ T cells with many being E7-specific (Figure 2c). These data indicate that intravaginal vaccination followed by electroporation generates potent antigen-specific CD8+ T-cell-mediated immune responses both systemically and locally, whereas intramusuclar vacciniation followed by electroportaiont only generates systemic immune responses.
Comparison of HPV16 E7-specific CD8+ T-cell responses induced by either intramuscular or vaginal submucosal vaccination with or without electroporation. Female C57BL/6 mice (5–8-week old) tetramer followed a by flow cytometry analysis. (a) Representative images of flow cytometry analysis of splenocytes. (b) Bar graph summary of the number of E7 tetramer+ CD8+ T cells among splenocytes. (c) Representative images of flow cytometry analysis of cervicovaginal cells. (d) Bar graph summary of the number of E7 tetramer+ CD8+ T cells among the cervicovaginal cells. *P<0.05 **P<0.01.
Intravaginal injection of HPV DNA vaccine followed by electroporation generates better antitumor effects and significantly prolonged survival in tumor-bearing mice compared with intramuscular injection followed by electroporation
Next, we tested the ability of the vaccine, administered by various routes with electroporation, to treat mice with cervicovaginal tumor. Mice were injected with 2 × 104 TC1-luc cells submucosally in the cervicovaginal tract. The mice were then vaccinated with pcDNA3-CRT/E7 via intramuscular or intravaginal injection followed by electroporation on day 3 and then boosted with the same regimen 1 week later. As shown in Figure 3, mice treated with pcDNA3-CRT/E7 intravaginally followed by electroporation had significantly increased antitumor effects compared with those vaccinated intramuscularly followed by electroporation, as shown by decreased luciferase activity. Furthermore, mice treated with pcDNA3-CRT/E7 intravaginally followed by electroporation had a significantly prolonged survival compared with those vaccinated intramuscularly. Taken together, these data suggest intravaginal vaccination with CRT/E7 DNA followed by electroporation significantly improves antitumor effects and survival of tumor-bearing mice compared with intramuscular vaccination followed by electroporation.
Intravaginal submucosal injection of HPV DNA vaccine followed by electroporation generated significantly better antitumor effects and prolonged survival of tumor-bearing mice. Female C57BL/6 mice (5–8-week old) were injected with 2 × 104 TC1-luc cells submucosally. The mice were then vaccinated with pcDNA3-CRT/E7 via intramuscular or intravaginal injection followed by electroporation on day 3. The mice were boosted with the same regimen 1 week later. The luciferase activity was measured with a Xenogen IVIS 100 imager at the indicated times and the survival of the mice was recorded. (a) Representative bioluminescence images of the vaginal TC1-luc tumors. (b) Bar graph summary of the bioluminescence of the tumors. (c) Survival of the cervicovaginal TC1-luc tumor-bearing mice. *P<0.05, **P<0.01.
Potent systemic and local antigen-specific IFN-γ+ CD8+ T-cell responses are induced by vaginal submucosal vaccination with electroporation
We next examined the effect of DNA vaccination through different routes followed by electroporation on the production of IFN-γ-secreting antigen-specific CD8+ T cells systemically and locally in mice with cervicovaginal tumors. TC-1 tumor-bearing mice were vaccinated with pcDNA3-CRT/E7 via intramuscular or intravaginal injection followed by electroporation on day 3. The vaccinated mice were boosted with the same regimen 1 week later. Seven days after the last vaccination, the mice were sacrificed in order to harvest splenocytes and cervicovaginal cells. The cells were then stimulated with HPV16 E7 peptide and IFN-γ-secreting E7-specific CD8+ T cells were detected by intracellular cytokine staining followed by a flow cytometry analysis. As shown in Figures 4a and b, mice vaccinated intramuscularly followed by electroporation and mice vaccinated intravaginally followed by electroporation generated a significantly greater number of IFN-γ+ E7-specific CD8+ T cells among the splenocytes compared with control mice. However, mice vaccinated intravaginally followed by electroporation had signifcantly greater IFN-γ+ E7-specific CD8+ T cells among cervicovaginal cells compared with both control mice and mice vaccinated intramuscularly followed by electroporation (Figures 4c and d). Of note, substantial number of non-reactive CD8+ T cells collected were also collected. Nevertheless, these data suggest that intravaginal HPV DNA vaccination followed by electroporation can increase the population of activated CD8+ T cells in cervicovaginal tract of TC-1 tumor-bearing mice.
Intravaginal submucosal injection of HPV DNA vaccine followed by electroporation generated significantly more infiltrating IFN-γ-secreting CD8+ T cells in the tumor tissue. Female C57BL/6 mice (5–8-week old) were injected with 2 × 104 TC1-luc cells submucosally. The mice were then vaccinated with pcDNA3-CRT/E7 via intramuscular or intravaginal injection followed by electroporation on day 3. The mice were boosted with the same regimen 1 week later. Seven days after the last vaccination, the mice were sacrificed in order to harvest splenocytes and cervicovaginal cells. The cells were then stimulated with HPV16 E7aa49-57 peptide in the presence of GolgiPlug and IFN-γ-secreting CD8+ T cells were detected by intracellular cytokine staining followed by a flow cytometry analysis. (a) Representative flow cytometry images of intracellular IFN-γ staining of splenocytes. (b) Bar graph summary of flow cytometry analysis of splenocytes. (c) Representative flow cytometry images of intracellular IFN-γ staining of cervicovaginal cells. (d) Bar graph summary of flow cytometry analysis cervicovaginal cells. *P<0.05, **P<0.01.
Intravaginal injection of HPV DNA vaccine followed by electroporation generates α4β7 expressing E7-specific CD8+ T cells in the cervicovaginal tract
Finally, we examined the expression of tissue resident T-cell markers α4β7 and CD49a on the E7-specific CD8+ T cells elicted by the vaccination with pcDNA3-CRT/E7 through different routes. α4β7 is a mucosa-associated homing integrin that functions by interacting with the mucosal addressin cell adhesion molecule-1 (MAdCAM-1) (for review see Gorfu et al.).15 CD49a is a mucosal integrin that is important for intratumoral CD8+ T-cell infiltration.11 Mice were vaccinated with pcDNA3-CRT/E7 through either intravaginal or intramuscular injection followed by electroporation and boosted with the same dose and regimen 1 week later. Cervicovaginal cells were isolated 1 week after the last immunization and analyzed for the expression of α4β7 and CD49a by flow cytometry. Mice vaccinated intravaginally with pcDNA3-CRT/E7 generated a significantly higher percentage of α4β7+ E7-specific CD8+ T cells among all cervicovaginal cells compared with mice vaccinated intramuscularly (Figures 5a and b). However, no difference was observed in the percentage of CD49+ E7-specific CD8+ T cells among all cervicovaginal cells between mice vaccinated intravaginally and intramuscularly with pcDNA3-CRT/E7 followed by electroporation (Figures 5c and d). These data imply that intravaginal vaccination with CRT/E7 DNA followed by electroporation may enhance the population of α4β7+ tissue resident CD8+ T cells in the cervicovaginal tract.
Intravaginal submucosal injection of HPV E7 DNA vaccine followed by electroporation generated significantly more E7-specific CD8+ T cells expressing α4β7. Female C57BL/6 mice (5–8-week old) were vaccinated with 20 μg of pcDNA3-CRT/E7 through either intravaginal or intramuscular injection followed by electroporation. The mice were boosted with the same regimen after 1 week. Seven days after the last vaccination, the mice were sacrificed to harvest cervicovaginal cells. The cells were stained with anti-mouse CD8, HPV16 E7aa49-57 peptide-loaded H-2Db tetramer and anti-mouse α4β7 (a and b) or CD49a (c and d) followed by flow cytometry analysis. (a) Representative flow cytometry image of α4β7 expression in cervicovaginal cells. (b) Summary of α4β7 expression in cervicovaginal cells. (c) Representative flow cytometry image of CD49a expression in cervicovaginal cells. (d) Summary of CD49a expression in cervicovaginal cells. *P<0.05.
Discussion
In the current study, we demonstrated that intravaginal delivery of DNA construct followed by electroporation increased the expression of the protein encoded by the DNA plasmid compared with delivery without electroporation. Additionally, CRT/E7 DNA vaccination intravaginally followed by electroporation induces increased E7-specific CD8+ T cells systemically and locally. Using a tumor treatment model, intravaginal vaccination with CRT/E7 followed by electroporation generated significantly improved antitumor effects and prolonged survival compared with intramuscular vaccination with electroporation. Furthermore, intravaginal vaccination generated significantly more potent local IFN-γ E7-specific CD8+ T-cell immune responses as well as α4β7-expressing E7-specific CD8+ T cells in the cervicovaginal tract than intramuscular vaccination with electroporation. Taken together, these data suggest that intravaginal vaccination with CRT/E7 DNA vaccine followed by electroporation generates potent local and systemic E7-specific cell-mediated immune responses and antitumor effects against an orthotopic cervicovaginal tract.
Here we found that intravaginal administration of CRT/E7 DNA vaccine followed by electroporation elicited high local and systemic immune responses, whereas intramuscular vaccination with electroporation generated substantial systemic immune responses only. We further assessed whether electroporation contributes to the observed antitumor effects. As shown in Supplementary Figure 1, we found that vaccination with naked backbone DNA construct, pcDNA3 followed by electroporation alone did not generate any appreciable antitumor effects compared with non-treated tumor-bearing mice. This suggests that the observed therapeutic effect is the outcome of local antigen-specific CD8+ T-cell immune response elicited by DNA vaccination that is enhanced by electroporation rather than the accidental electrocuting of tumor cells as a result of local electroporation. We further found that intravaginal vaccination with CRT/E7 DNA with electroporation elicited a high percentage of α4β7-expressing E7-specific CD8+ T cells in the cervicovaginal tract. These data suggest that local vaccination may better at generating a local CD8+ T-cell-mediated response than vaccination at a distant administration site. Indeed, investigators have shown that that intravaginal immunization with HPV pseudoviruses carrying DNA encoding antigens induced potent antigen-specific intraepithelial CD103+ CD8+ T-cell responses in the cervicovaginal mucosa.14 This local vaccination regimen promoted local proliferation and retention of primed antigen-specific CD8+ T cells.14 Furthermore, Sandoval et al.11 demonstrated that mucosal vaccination generated better CD8+ T-cell responses at the site of mucosal TC-1 tumors in mice. Additionally, the generation of effector memory T cells that home to epithelium of the cervicovaginal tract may be particularly important in the induction of an effective immune response against HPV-associated cervical tumors.12 In the future, it will be important to determine the mechanism of this process.
The CRT/E7 DNA vaccine employed in the current study is being tested in clinical trials. An ongoing Phase I clinical trial is examining three routes of pNGVL4a-CRT/E7(detox) vaccine administration (intradermal administration via gene gun, intramuscular administration and intralesional delivery) to treat CIN 2/3 lesions in HPV16 positive patients (NCT00988559).16 Furthermore, pNGVL4a-CRT/E7(detox) has been explored in a phase I trial in combination with cyclophsosphamide in HPV16-associated head and neck cancer patients (NCT01493154). Thus, the current study has a significant potential for translation to the clinic.
In order for this treatment regimen to be translated to the clinic, creation of an appropriate electroporation device will be required. Currently, the electroporation devices used in the clinic for enhancing the efficiency of DNA vaccination are used in conjunction with intramuscular injection of the vaccine. For example, a Phase 2 trial is being conducted in CIN 2/3 patients to test the VGX-3100 DNA vaccine administered intramuscularly followed by electroporation with the CELLECTRA constant current device by Inovio Pharmaceuticals (NCT01304524). The Phase I trial in head and neck cancer patients mentioned above uses the Ichor Medical Systems TriGrid Delivery System for electroporation following intramuscular vaccination with pNGVL4a-CRT/E7(detox) (NCT01493154). The TriGrid Delivery System has also been tested in combination with a therapeutic HPV DNA vaccine (GX-188E) in CIN 3 patients (NCT01634504). Thus, the current study provides substantial motivation for the development of a modified electroporation device that can be applied to the to the cervicovaginal area.
In summary, the current study we demonstrate that submucosal intravaginal vaccination followed by electroporation generates potent mucosal and systemic CD8+ T-cell immune responses and antitumor effects against orthotopic TC-1 tumors. Because local cell-mediated immune responses are important for the clearance of HPV-associated tumor cells, the approach described in the current study may likely be applied for the control of HPV-associated lesions in the cervicovaginal tract.
Materials and methods
Mice
6–8 week-old female C57BL/6 mice were purchased from the National Cancer Institute and housed in the Johns Hopkins Oncology Center Animal Facility. All animal procedures were performed according to approved protocols and in accordance with recommendations for the proper use and care of laboratory animals.
Cells
TC-1 cells that express luciferase (TC-1/luc) were generated and cultured by the using methods that has been described previously17 and cultured as described.18
Antibodies, peptide and HPV16 E7 tetramer
FITC and PE-conjugated anti-mouse CD8a (clone 53.6.7), FITC-conjugated anti-mouse IFN-γ (clone XMG1.2), AF647-conjugated anti-mouse CD49a (clone Ha31/8) antibodies, and purified anti-mouse CD16/32 (Fc Block) were purchased from BD Pharmingen (San Diego, CA, USA). APC-conjugated anti-mouse α4β7 (clone DATK32) was purchased from eBioscience (San Diego, CA, USA). The H-2Db-restricted HPV16 E7aa49-57 peptide, RAHYNIVTF, was synthesized by Macromolecular Resources (Denver, CO, USA) at a purity of⩾80%. PE-conjugated, HPV16 E7aa49-57 peptide-loaded H-2Db tetramer was provided by NIH Tetramer Core Facility and has been used in our previous studies.17, 19
DNA vaccines
The construction of the pcDNA3-CRT/E7 plasmid DNA vaccine used in this study has been described previously.8 pcDNA3-luciferase DNA plasmid was a generous gift from Dr Hyam I Levitsky (Johns Hopkins Medical Institutions, Baltimore, MD, USA).
DNA vaccination
Mice were anesthetized before vaccination. Based on our previous experience, 20 μg per mouse of plasmid DNA is effective in generating potent antigen-specific CD8+ T-cell response,17 and is thus chosen as the dose for DNA vaccine in this study. For vaginal vaccination, 20 μg of pcDNA3-CRT/E7 DNA vaccine was submucosally injected into the lateral vaginal wall of the mice and either followed immediately by electroporation or left untreated. For intramuscular vaccination, 20-μg pcDNA3-CRT/E7 plasmid was injected into quadriceps femoris muscle of mice and either followed immediately by electroporation or left untreated. The mice were boosted with the same regimen one week later.
Electroporation
For vaginal vaccination, pcDNA3-luciferase or pcDNA3-CRT/E7 plasmid was submucosally injected into the lateral vaginal wall of the mice. This was followed by electroporation with an ECM830 Square Wave Electroporation System (BTX Harvard Apparatus company, Holliston, MA, USA). The electroporation was performed at the injection site using a tweezertrode with one plate inside the vagina and the other on the ipsilateral vulva. Eight pulses of 72 V each were delivered for 20-ms pulse duration at 200 ms intervals. For intramuscular vaccination, pcDNA3-CRT/E7 plasmid was injected into quadriceps femoris muscle of mice and immediately followed by electroporation with two-needle array electrodes and fifteen pulses of 72 V each were delivered for 20-ms pulse duration at 200 ms intervals.
Splenocyte and cervicovaginal cell preparation
Seven days after the last vaccination, spleen and cervicovaginal tissues were harvested from the mice. Vaginal tissues were surgically excised by using a sterile technique, placed in RPMI-1640 medium containing 100 U ml−1 penicillin and 100 μg ml−1 streptomycin and washed with phosphate-buffered saline. The tissues were then minced into 1–2-mm pieces and immersed in serum-free RPMI-1640 medium containing 0.05 mg ml−1 collagenase I, 0.05 mg ml−1 collagenase IV, 0.025 mg ml−1 hyaluronidase IV, 0.25 mg ml−1 DNase I, 100 U ml−1 penicillin and 100 μg ml−1 streptomycin and incubated at 37 °C with periodic agitation for 1 h. The vaginal digest was then filtered through a 70-μm nylon filter mesh to remove undigested tissue fragments. The resultant single cervicovaginal cells were washed twice in phosphate-buffered saline, and viable cells were identified using trypan blue dye exclusion. For the preparation of splenocytes, the spleen was meshed through a 70-μm nylon filter mesh. After the lysis of red blood cells with ACK lysis buffer, the cells were washed and viable cells were identified using trypan blue dye exclusion.
Flow cytometry analysis
For the analysis of HPV16 E7-specific CD8+ T-cell responses with tetramer, splenocytes (1 × 106) and cervicovaginal cells (3–5 × 105) were washed once with FACS wash buffer (phosphate-buffered saline+0.5 BSA). To avoid nonspecific antibody binding through surface Fc receptor, all cells were preincubated with BD Fc Block. The cells were then stained with FITC-conjugated anti-mouse CD8a and PE-conjugated HPV16 E7aa49-57 peptide-loaded H-2Db E-7 tetramer. After being washed, the cells were acquired with FACSCalibur flow cytometer (BD Biosciences, Mountain View, CA, USA) and analyzed with FlowJo software (TreeStar Inc., Ashland, OR, USA).
For the analysis of HPV16 E7-specific CD8+ T-cell responses with intracellular IFN-γ staining, splenocytes (5 × 106) and cervicovaginal cells (5 × 105) were stimulated overnight with 1 μg ml−1 HPV16 E7aa49-57 peptide in the presence of 1 μl ml−1 GolgiPlug (BD Pharmingen). The stimulated cells were washed once with FACS wash buffer and stained with PE-conjugated anti-mouse CD8a antibody. Cells were then permeabilized and fixed using the Cytofix/Cytoperm kit according to the manufacture’s instruction (BD Pharmingen). Intracellular IFN-γ was stained with FITC-conjugated anti-mouse IFN-γ antibody. After being washed, the cells were acquired with FACSCalibur flow cytometer and analyzed with FlowJo software.
In vivo tumor treatment experiments
2 × 104 TC-1 per luc cells were submucosally injected at the lateral vaginal wall of the mice by using methods described previously.20 It has been shown that this number of tumor cells can lead to a tumor growth success rate of 82%.21 Three days later, mice were vaccinated with 20 μg of pcDNA3-CRT/E7 as indicated. The mice were boosted once with the same regimen 1 week later. Cervicovaginal tumor growth was monitored by bioluminescence using a Xenogen IVIS 100 imager (Calioer Life Science, Hopkinton, MA, USA) at indicated time.
Statistical analysis
All data are expressed as mean±s.d. Comparisons between individual data points were made using Student’s t-test. The non-parametric Mann–Whitney test was used for comparing two different groups. Results for tumor treatment experiments were evaluated by Kaplan–Meier analysis. All P-values <0.05 were considered significant.
References
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999; 189: 12–19.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D . Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
Tran NP, Hung CF, Roden R, Wu TC . Control of HPV infection and related cancer through vaccination. Recent Results Cancer Res 2014; 193: 149–171.
Lin K, Doolan K, Hung CF, Wu TC . Perspectives for preventive and therapeutic HPV vaccines. J Formos Med Assoc 2010; 109: 4–24.
Lin K, Roosinovich E, Ma B, Hung CF, Wu TC . Therapeutic HPV DNA vaccines. Immunol Res 2010; 47: 86–112.
Yugawa T, Kiyono T . Molecular mechanisms of cervical carcinogenesis by high-risk human papillomaviruses: novel functions of E6 and E7 oncoproteins. Rev Med Virol 2009; 19: 97–113.
zur Hausen H . Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer 2002; 2: 342–350.
Cheng WF, Hung CF, Chai CY, Hsu KF, He L, Ling M et al. Tumor-specific immunity and antiangiogenesis generated by a DNA vaccine encoding calreticulin linked to a tumor antigen. J Clin Invest 2001; 108: 669–678.
Kim JW, Hung CF, Juang J, He L, Kim TW, Armstrong DK et al. Comparison of HPV DNA vaccines employing intracellular targeting strategies. Gene Therapy 2004; 11: 1011–1018.
Best SR, Peng S, Juang CM, Hung CF, Hannaman D, Saunders JR et al. Administration of HPV DNA vaccine via electroporation elicits the strongest CD8+ T cell immune responses compared to intramuscular injection and intradermal gene gun delivery. Vaccine 2009; 27: 5450–5459.
Sandoval F, Terme M, Nizard M, Badoual C, Bureau MF, Freyburger L et al. Mucosal imprinting of vaccine-induced CD8(+) T cells is crucial to inhibit the growth of mucosal tumors. Sci Transl Med 2013; 5: 172ra20.
Trimble CL, Clark RA, Thoburn C, Hanson NC, Tassello J, Frosina D et al. Human papillomavirus 16-associated cervical intraepithelial neoplasia in humans excludes CD8 T cells from dysplastic epithelium. J Immunol 2010; 185: 7107–7114.
Soong RS, Song L, Trieu J, Knoff J, He L, Tsai YC et al. Toll-like receptor agonist imiquimod facilitates antigen-specific CD8+ T-cell accumulation in the genital tract leading to tumor control through IFNgamma. Clin Cancer Res 2014; 20: 5456–5467.
Cuburu N, Graham BS, Buck CB, Kines RC, Pang YY, Day PM et al. Intravaginal immunization with HPV vectors induces tissue-resident CD8+ T cell responses. J Clin Invest 2012; 122: 4606–4620.
Gorfu G, Rivera-Nieves J, Ley K . Role of beta7 integrins in intestinal lymphocyte homing and retention. Curr Mol Med 2009; 9: 836–850.
Center SKCC. A Pilot Study of pnGVL4a-CRT/E7 (Detox) for the Treatment of Patients With HPV16+ Cervical Intraepithelial Neoplasia 2/3 (CIN2/3). In: ClinicalTrials.gov [Internet]. National Library of Medicine (US): Bethesda (MD), 2009.
Peng S, Song L, Knoff J, Wang JW, Chang YN, Hannaman D et al. Control of HPV-associated tumors by innovative therapeutic HPV DNA vaccine in the absence of CD4+ T cells. Cell Biosci 2014; 4: 11.
Lin KY, Guarnieri FG, Staveley-O'Carroll KF, Levitsky HI, August JT, Pardoll DM et al. Treatment of established tumors with a novel vaccine that enhances major histocompatibility class II presentation of tumor antigen. Cancer Res 1996; 56: 21–26.
Wu CY, Yang LH, Yang HY, Knoff J, Peng S, Lin YH et al. Enhanced cancer radiotherapy through immunosuppressive stromal cell destruction in tumors. Clin Cancer Res 2014; 20: 644–657.
Zeng Q, Peng S, Monie A, Yang M, Pang X, Hung CF et al. Control of cervicovaginal HPV-16 E7-expressing tumors by the combination of therapeutic HPV vaccination and vascular disrupting agents. Hum Gene Ther 2011; 22: 809–819.
Decrausaz L, Goncalves AR, Domingos-Pereira S, Pythoud C, Stehle JC, Schiller J et al. A novel mucosal orthotopic murine model of human papillomavirus-associated genital cancers. International journal of cancer. Int J Cancer 2011; 128: 2105–2113.
Acknowledgements
This work was supported by the National Institutes of Health/National Cancer Institute Cervical Cancer SPORE P50CA098252, 2R01CA114425-06, and 5R21CA178255-02 grants.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
TC Wu holds equity in Papivax LLC and serves as a scientific advisor of Papivax Biotech Inc. The terms of these arrangements are managed by Johns Hopkins University in accordance with its conflict of interest policies.
Additional information
Supplementary Information accompanies this paper on Gene Therapy website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Sun, Y., Peng, S., Qiu, J. et al. Intravaginal HPV DNA vaccination with electroporation induces local CD8+ T-cell immune responses and antitumor effects against cervicovaginal tumors. Gene Ther 22, 528–535 (2015). https://doi.org/10.1038/gt.2015.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2015.17