Abstract
Lung cancer still remains to be challenged by novel treatment modalities. Novel locally targeted routes of administration are a methodology to enhance treatment and reduce side effects. Intratumoral gene therapy is a method for local treatment and could be used either in early-stage lung cancer before surgery or at advanced stages as palliative care. Novel non-viral vectors are also in demand for efficient gene transfection to target local cancer tissue and at the same time protect the normal tissue. In the current study, C57BL/6 mice were divided into three groups: (a) control, (b) intravenous and (c) intatumoral gene therapy. The novel 2-Diethylaminoethyl-Dextran Methyl Methacrylate Copolymer Non-Viral Vector (Ryujyu Science Corporation) was conjugated with plasmid pSicop53 from the company Addgene for the first time. The aim of the study was to evaluate the safety and efficacy of targeted gene therapy in a Lewis lung cancer model. Indeed, although the pharmacokinetics of the different administration modalities differs, the intratumoral administration presented increased survival and decreased distant metastasis. Intratumoral gene therapy could be considered as an efficient local therapy for lung cancer.
Similar content being viewed by others
Introduction
Lung cancer treatment in an evolving field as novel pathways and gene mutations are being discovered.1 Until recently, non-specific cytotoxic drugs were administered as first-line treatment; however, with the evolving science of pharcogenomics, agents targeting the mutations of lung cancer were introduced in the market as first-line treatment.2, 3, 4 Several new pathways are being investigated as possible targets for inhibition, and lung cancer treatment is directed to being personalized.5, 6, 7 Administering non-specific cytotoxic agents by intravenous route or oral targeting agents has, for many patients, adverse effects that can potentially postpone their treatment.8, 9, 10 Therefore the concept of delivering the necessary dose of treatment directly to the target tissue has been investigated with (a) gene therapy, (b) immunotherapy and (c) chemotherapy or combinations of the above methods.11, 12, 13, 14, 15, 16, 17 The following methods for intratumoral treatment have been used: (a) brachytherapy, (b) photodynamic therapy, (c) thermal and non-thermal ablative therapies, (d) chemotherapy, and (e) gene therapy.16, 18, 19, 20 Gene therapy has been used for lung cancer to sensitize cells to radiotherapy and chemotherapy.21, 22, 23 Gene therapy is used to insert genetic material into a cell. There are currently two vehicles that are used for efficient gene transportation: the viral and the non-viral vectors. There are advantages and disadvantages for each vehicle. The viral vectors tend to induce neutralizing antibodies known as NABs within 3–7 days, and several non-viral vectors have a low DNA uptake capability and have been observed to be toxic for certain normal cells, such as the airway epithelium.24, 25, 26, 27, 28 The intratumoral treatment efficiency depends on the following factors: (a) interstitial fluid pressure (IFP) within the tumor, (b) local hypoxia, (c) structural abnormalities within the tumor, (d) heterogenous distribution due to abnormal vessel formation within the tumor, and (e) extracellular matrix (ECM), which consists of collagen, fibroblasts, tumor cells and elastin.29 Before designing a drug for intratumoral administration, we should consider first the method of diffusion that we want to use. The passive transportation, which is based on the physicochemical properties of the injected compound, and active transportation, which is based on the concept of antigen–antibody connection.30 In addition, within the process of drug administration, heating and cooling techniques have been additionally used to enhance the drug diffusion.31, 32 The time release effect has a major role in this kind of treatment as it prolongs the local deposition to the target tissue and increases apoptosis. Additionally, and at the same time, it will postpone any unnecessary toxic drug concentration to diffuse within normal tissue. Carriers have been investigated in order to create a local sustain release effect.33, 34 Nanocarriers have displayed the enhanced permeability and retention (EPR) effect where a drug has increased local deposition and diffusion.29, 35 Surface modification on nanoparticles (NPs) with didodecyldimethylammoniumbromide is an example where the NPs presented greater interaction with the membrane lipids of cancer cells and improved local retention of the administered compound.36 The EPR effect has been observed to be controlled by heat-shock protein 32 and carbon monoxide.37 Moreover, the addition of polyethylene glycol (PEG) has been observed to enhance the EPR effect and sustain release as it cannot be recognized by the macrophages.38 Novel techniques of intratumoral inflammation imaging have been investigated with19F-magnetic resonance.39 Currently, there has been extensive research on intratumoral gene therapy in pancreatic cancer, and most of our knowledge regarding this treatment is due to this type of cancer treatment experimentation.40, 41 11Intratumoral chemotherapy has been also used for prostate cancer, glioblastoma, melanoma, breast cancer, neuroblastoma and hepatocellular carcinoma42, 43, 44, 45, 46, 47, 48, 49, 50 (Table 1). Several vectors have been used in these different studies, with different intratumoral therapeutic strategies (Table 2). In the current study, we will present our data from the administration of the 2-Diethylaminoethyl-Dextran Methyl Methacrylate Copolymer Non-Viral Vector (DDMC, Ryujyu science corporation, Seto-City, Japan) conjugated with plasmid p53 in C57BL/6 mice in three different groups: (a) control, (b) intravenous, and (c) intratumoral in an effort to identify which methodology could efficiently present local tumor control and distant metastasis control.
Results
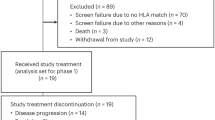
Tumor growth rate was controlled in the intravenous and intratumoral group, in comparison to the control group. (Tables 3, 4, 5) Our results indicate that distant metastasis in the lung was controlled in a higher degree in the intratumoral group (group 2); in two subjects there were no lung metastasis after 21 days and 6 administrations. In Figure 1, macroscopical findings indicate that only in the control group lung metastasis were visible. In Figure 2, the gene complex is clearly demonstrated within lung micrometastasis for both the intravenous and intratumoral group, therefore it is clear that with both modalities the therapy is efficiently delivered in the lung. However; a higher degree of apoptosis is observed with the intratumoral group as there are clear regions surrounding the gene complex. Also, it has to be stated that in the intravenous group two mice died after administration probably due to the gene complex. The mean survival can be displayed as follows in terms of efficiency: intratumoral (17.4 days)>intravenous (12.6 days)>control (12.6 days). Additionally, Ki-67 and TTF-1 were positively expressed (Figure 3). There was no difference in the survival between the intravenous and control group; however, distant lung metastasis was controlled up to a degree.
(a) Lung micrometastasis control group; (b) yellow arrow indicates root of intratumoral injection and gene-complex release, white arrow indicates tumor necrosis and black arrow indicates the gene-complex (c) black arrow indicates the gene complex and white arrow tumor necrosis; (d) primary tumor cells (back inoculated tumor).
Discussion
Previously, it has been observed that local administration of intratumoral chemotherapy is safe and efficient. It was observed that adverse effects were minimal and even complete lung atelectasis was re-expanded.16 However; the ideal methodology still has to be investigated as several parameters have to be improved. An algorithm has to be built identifying the proper molecules that will efficiently diffuse within the tumor. There are several factors influencing the distribution as previously stated (for example, ECM, IFP, vessel structure) that differ among different tumor types (for example, cavitation-squamus versus no cavitation-non-squamus).51 The proper volume/concentration that induces cell apoptosis has to be identified for each drug before study initiation. One of the methods that could be used towards this direction is the ITASSER (http://zhanglab.ccmb.med.umich.edu, Ann Arbor, MI, USA), which has already been used in previous studies.52, 53 The same principals of local intratumoral therapy design apply for gene therapy. We would like to have a vector–gene complex that will efficiently distribute within the tissue and if possible through local vessels and lymphnodes throughout the systematic circulation.54 This observation has been done with aerosol local chemotherapy administration where distribution of the administered drug was observed in the local lymph nodes and local cisplatin concentration was correlated with systematic.54, 55 It has been previously stated that rapid tumor cell proliferation and weakly developed lymphatics cause high IFP and blood vessel remodeling by intus-susception or compression.51 Therefore high interstitial pressure is observed in the center of the tumor, which blocks the efficient distribution of the drug, whereas this effect is diminished while moving from the center of the tumor to the periphery. The ECM differs between normal tissue and cancer tissue. The following collagen types I, II, III, V and IX, tenasin C, fibronectin and proteoglycans exhibit increased accumulation and generate a dense network in tumor tissues. Moreover, excessive deposition of ECM components decrease the distance between neighboring ECM components and diminish the pore size of the tumor matrix. Increased ‘stiffness’ of the ECM in cancer tissue is observed and therefore the efficient distribution is again blocked for various molecules such as; anti-tumor immune cells, chemotherapeutic agents, therapeutic viruses, immunotoxins, interferons, monoclonal antibodies and complement.51 First, ECM influences the IFP. Furthermore, the abnormal architecture of vessels and lymphatics are responsible for blocking the defense mechanisms of the body, such the M2 macrophages. The intravenous-administered drugs once administered reach the tumor sites and exit the tumor vasculature and translocate through the interstitial space in order to reach their target cells. Trans-endothelial transport of macromolecular drugs involves a phenomenon known as the EPR effect in solid tumors.51 We need the EPR effect for the leaky abnormal vessels within the tumor to enhance the different macromolecule distribution. The EPR effect is enhanced with novel nanocarriers.33, 38, 48, 56, 57, 58 It has been previously observed that the hyper-permeability of the tumor vessels in combination with the absence of functional lymphatics induce a prolonged deposition of several drugs. The hyper-permeability (>10 nm) allows drug molecule’s transportation within the tumor tissue; however, not in the normal tissue where particles >10 nm cannot be transported. Therefore this effect can be used as a method of normal tissue protection. It has to be stated that the EPR effect differs between cancer types and within the tumor from one region to another.59 The tumor tissue matrix is a very important parameter; dense extracellular fibers and matrix within the tumor will block large NPs to efficiently penetrate the tumor and diffuse.60, 61 Renal clearance is more rapid in smaller NPs (<6 nm), while reticuloendothelial clearance is usually avoided with PEGylated drug, like in the case of pegylated liposomal doxorubicin.62, 63 Moreover, the shape and charge of NPs have an important role in the diffusion efficiency. Elongated NPs penetrate the vascular flux more efficiently when compared with spherical particles.64 Cationic NPs transported more efficiently when compared with neutral or anionic.65, 66 Novel nanoparticles are designed to decrease their size upon acidic pH and matrix metalloproteinases (MMPs), however; further experimentation is needed in order to draw a clear conclusion how these parameters interact with the tumor microenvironment.67, 68 The IFP is high within solid tumors and inhibits the penetration of drugs.69 Increased IFP is also due to a dense ECM and inadequate lymphatic drainage.70 Again increased IFP inhibits drug penetration within solid tumors. High levels of hyaluronic acid (HA) have been found in the ECM of solid tumors and are collated with increased IFP. Administration of HA-targeting enzyme (PEGPH20) was able to diminish the HA levels and therefore vessels were patent and drug penetration was efficient.71 Furthermore, upon designing the study we should know how the administered solution will be diffused throughout the target tissue. Positron emission tomography is one method previously used to identify the optimal volume/concentration for intratumoral administration.72 There are two major methods of transportation: the passive and active targeting. The active transportation is based on the ligand–receptor interaction, while in the passive transportation the diffusion of a compound within the tissue is based on its physical properties.30 Gene therapy has been previously investigated targeting epidermal growth factor, vascular endothelial growth factor, KRAS, immunotherapy, ECM factors and tumor microenvironment.42, 48, 49, 73, 74, 75, 76 Additional methods of enhancing the intratumoral gene therapy have been previously performed with the addition of radiotherapy, chemotherapy, thermal ablation, sorafenib, imatinib, use of ultrasound system, rituximab and dendritic cells to gene therapy administration alone.34, 77, 78, 79, 80, 81, 82 In our current study, we used the novel non-viral vector DDMC as the vehicle for the local intratumoral administration of pSicop53. The DDMC was synthesized by graft polymerization of methyl methacrylate (MMA) onto 2-Diethylaminoethyl-Dextran Methyl Methacrylate Copolymer (DAEX). These copolymers have hydrophobic and hydrophilic regions and have high transfection efficiency and they can also be sterilized by autoclavation.83 Investigation with DDMC/DNA presented in vitro higher transfection efficiency in COS-7 cell lines84 when it compared with DAEX/DNA in HEK293 cell lines.85 DDMC has efficient absorption capability both for RNA and DNA. This is due to their cationic property and has been found to be influenced by pH and ionic strengths.86 Furthermore, the DDMC/DNA formation reaction is influenced by the Coulomb forces. The hydrophobic bonding strength as well as the hydrogen bonding strength have a role due to the hydrophobicity of the grafted MMA sections. Optimal cell affinity was also previously observed.87 The DDMC/DNA and gene transfection are still under investigation.83
Conclusions
Intratumoral gene therapy can be used alone or in combination with additional methods, such as radiotherapy and/or chemotherapy. Gene therapy could be used to sensitize chemo-resistant or radio-resistant tumors during the treatment course. The application currently can be done in lesions visible within the respiratory tract or using the endobronchial ultrasound bronchoscope. It is an efficient method of treatment; however, current studies indicate that a combination with additional modalities as previously stated offer improved disease control. Intratumoral gene therapy for lung cancer still has to find its place in the algorithm of treatment either as neo-adjuvant in early-stage disease or as a palliative in advanced stages.
Materials and methods
Non-viral vector and p53
The non-viral vector was purchased from Ryujyu science corporation, Seto-City, Japan by PZ and AB under the contract EG179806487JP (A18503015(121223b1), A18503016(121227b3), A18503017(121227b4), A18503018(121227b5), A18503019(130228b8) and A18503020(130228b10)). The non-viral vector has the following characteristics: fast and easy procedure, stable for autoclaving sterilization at 121 °C for 15 min, broad peak performance, applicable in high-throughput screening, no serum inhibition, broad cell line range, best results with siRNA applications, excellent reproducibility, low toxicity in comparison with DEAE-dextran, high efficiency by use of low DNA amounts, a high DNase protection facility by DNase degradation, and best price/value ratio. The plasmid p53 was purchased from Addgene (Cambridge, MA, USA) as ‘Addgene plasmid 123519, 124665, 125156,125157’. Enhanced green fluorescent protein is expressed from this plasmid as a marker, but it is not a fusion protein. Cre causes enhanced green fluorescent protein to be recombined out of the construct, activating shRNA expression (Vector backbone: pSico, Vector type: Mammalian Expression, Lentiviral, RNAi, Cre/Lox).88 The preparation of the complex (non-viral vector-p53) has been previously described, and 0.2 ml was chosen to be the injected volume for both the investigated groups.89, 90
Mice
Thirty C57BL/6 mice aged 7–8 weeks were purchased from the Hellenic Institute (Athens, Greece) PASTEUR (code 000.2481) with purchase code A-ΔA00000399 and were divided into three groups. The Institute has the following authorization for production and experimentation of mice EL 25 BIO 011 and EL 25 BIO 013. The mice included were isolated (one per cage) in a temperature-controlled room on 12-h light–dark cycle and were allowed free access to food and water. The Lewis lung carcinoma cell line was obtained from ATCC (LGC Standards GmbH, Wesel, Germany) (CRL-1642). The cells were routinely cultured in 25-cm2 tissue culture flasks containing RPMI (ATCC, 30-2002) supplemented with 10% fetal bovine serum (Biochrom, Thessaloniki, Greece) according to the supplier’s instruction. The cell line was incubated at 37 °C in 5% CO2. The doubling time of the cell line was 21 h.91 At confluence, cells were harvested with 0.25% trypsin and then were resuspended at 1.5 × 106 cells in 0.15 ml phosphate-buffered saline, Dulbecco, Biochrom), which was injected in mice. The back was inoculated subcutaneously (27-guage needle). The tumor volume was measured once weekly using bidimensional diameters (caliper) with the equation V=1/2ab2, where the a represents the length and b the width (mm3). The tumor was grown on the back of the mice (Figure 4).
References
Rosell R, Bivona TG, Karachaliou N . Genetics and biomarkers in personalisation of lung cancer treatment. Lancet 2013; 382: 720–731.
Lee SY, Kang HG, Yoo SS, Kang YR, Choi YY, Lee WK et al. Polymorphisms in DNA repair and apoptosis-related genes and clinical outcomes of patients with non-small cell lung cancer treated with first-line paclitaxel-cisplatin chemotherapy. Lung Cancer 2013; 82: 330–339.
Gridelli C, De Marinis F, Di Maio M, Cortinovis D, Cappuzzo F, Mok T . Gefitinib as first-line treatment for patients with advanced non-small-cell lung cancer with activating epidermal growth factor receptor mutation: implications for clinical practice and open issues. Lung Cancer 2011; 72: 3–8.
Li T, Kung HJ, Mack PC, Gandara DR . Genotyping and genomic profiling of non-small-cell lung cancer: implications for current and future therapies. J Clin Oncol 2013; 31: 1039–1049.
Nelson V, Ziehr J, Agulnik M, Johnson M . Afatinib: emerging next-generation tyrosine kinase inhibitor for NSCLC. Oncol Targets Ther 2013; 6: 135–143.
Gadgeel SM, Wozniak A . Preclinical rationale for PI3K/Akt/mTOR pathway inhibitors as therapy for epidermal growth factor receptor inhibitor-resistant non-small-cell lung cancer. Clin Lung Cancer 2013; 14: 322–332.
Darwiche K, Zarogoulidis P, Baehner K, Welter S, Tetzner R, Wohlschlaeger J et al. Assessment of SHOX2 methylation in EBUS-TBNA specimen improves accuracy in lung cancer staging. Ann Oncol 2013; 24: 2866–2870.
Zarogoulidis K, Papagiannis A, Ziogas E, Fahantidou E, Dermitzakis G, Gioulekas D et al. Management of chemotherapy-related anaemia with low-dose recombinant human erythropoietin in patients with small cell lung cancer. Eur J Cancer 1997; 33: 2428–2431.
Ihbe-Heffinger A, Paessens B, Berger K, Shlaen M, Bernard R, von Schilling C et al. The impact of chemotherapy-induced side effects on medical care usage and cost in German hospital care—an observational analysis on non-small-cell lung cancer patients. Support Care Cancer 2013; 21: 1665–1675.
Ong CK, Tan WC, Chan LC, Abdul Razak M . Cutaneous side-effects of epidermal growth factor receptor-tyrosine kinase inhibitor (TKI) in the treatment of lung cancer: description and its management. Med J Malaysia 2012; 67: 222–223.
Xie FJ, Zhao P, Zhang YP, Liu FY, Nie XL, Zhu YH et al. Adenovirus-mediated interferon-gamma gene therapy induced human pancreatic carcinoma Capan-2 cell apoptosis in vitro and in vivo. Anat Rec (Hoboken) 2013; 296: 604–610.
Zarogoulidis P, Chatzaki E, Hohenforst-Schmidt W, Goldberg EP, Galaktidou G, Kontakiotis T et al. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: a case series and literature review. Cancer Gene Ther 2012; 19: 593–600s.
Celikoglu F, Celikoglu SI, Goldberg EP . Bronchoscopic intratumoral chemotherapy of lung cancer. Lung Cancer 2008; 61: 1–12.
Zarogoulidis P, Hohenforst-Schmidt W, Darwiche K, Krauss L, Sparopoulou D, Sakkas L et al. 2-Diethylaminoethyl-dextran methyl methacrylate copolymer nonviral vector: still a long way toward the safety of aerosol gene therapy. Gene Therapy 2013; 20: 1022–8s.
Zarogoulidis K, Ziogas E, Boutsikou E, Zarogoulidis P, Darwiche K, Kontakiotis T et al. Immunomodifiers in combination with conventional chemotherapy in small cell lung cancer: a phase II, randomized study. Drug Des Dev Ther 2013; 7: 611–617.
Hohenforst-Schmidt W, Zarogoulidis P, Darwiche K, Vogl T, Goldberg EP, Huang H et al. Intratumoral chemotherapy for lung cancer: re-challenge current targeted therapies. Drug Des Dev Ther 2013; 7: 571–583.
Geletneky K, Huesing J, Rommelaere J, Schlehofer JR, Leuchs B, Dahm M et al. Phase I/IIa study of intratumoral/intracerebral or intravenous/intracerebral administration of Parvovirus H-1 (ParvOryx) in patients with progressive primary or recurrent glioblastoma multiforme: ParvOryx01 protocol. BMC Cancer 2012; 12: 99.
Zheng X, Zhou F, Wu B, Chen WR, Xing D . Enhanced tumor treatment using biofunctional indocyanine green-containing nanostructure by intratumoral or intravenous injection. Mol Pharm 2012; 9: 514–522.
Macha HN, Freitag L . The role of brachytherapy in the treatment and control of central bronchial carcinoma. Monaldi Arch Chest Dis 1996; 51: 325–328.
Freitag L, Ernst A, Thomas M, Prenzel R, Wahlers B, Macha HN . Sequential photodynamic therapy (PDT) and high dose brachytherapy for endobronchial tumour control in patients with limited bronchogenic carcinoma. Thorax 2004; 59: 790–793.
Li B, He H, Tao BB, Zhao ZY, Hu GH, Luo C et al. Knockdown of CDK6 enhances glioma sensitivity to chemotherapy. Oncol Rep 2012; 28: 909–914.
Xu Y, Zheng W, Wang T, Wang P, Zhu L, Ma X . Genetic protein TmSm(T34A) enhances sensitivity of chemotherapy to breast cancer cell lines as a synergistic drug to doxorubicin. Biomed Pharmacother 2012; 66: 368–372.
Xiong J, Sun WJ, Wang WF, Liao ZK, Zhou FX, Kong HY et al. Novel, chimeric, cancer-specific, and radiation-inducible gene promoters for suicide gene therapy of cancer. Cancer 2012; 118: 536–548.
Zarogoulidis P, Kontakiotis T, Zarogoulidis K . Inhaled gene therapy in lung cancer: ‘as for the future, our task is not to foresee it, but to enable it’. Ther Deliv 2012; 3: 919–921.
Darwiche K, Zarogoulidis P, Karamanos NK, Domvri K, Chatzaki E, Constantinidis TC et al. Efficacy versus safety concerns for aerosol chemotherapy in non-small-cell lung cancer: a future dilemma for micro-oncology. Future Oncol 2013; 9: 505–525.
Zarogoulidis P, Darwiche K, Hohenforst-Schmidt W, Huang H, Li Q, Freitag L et al. Inhaled gene therapy in lung cancer: proof-of-concept for nano-oncology and nanobiotechnology in the management of lung cancer. Future Oncol 2013; 9: 1171–1194.
Chirmule N, Hughes JV, Gao GP, Raper SE, Wilson JM . Role of E4 in eliciting CD4 T-cell and B-cell responses to adenovirus vectors delivered to murine and nonhuman primate lungs. J Virol 1998; 72: 6138–6145.
Zarogoulidis P, Giraleli C, Karamanos NK . Inhaled chemotherapy in lung cancer: safety concerns of nanocomplexes delivered. Ther Deliv 2012; 3: 1021–1023.
Stylianopoulos T . EPR-effect: utilizing size-dependent nanoparticle delivery to solid tumors. Ther Deliv 2013; 4: 421–423.
Bae YH . Interview with Dr You Han Bae: ligand-mediated versus 'passive' targeting approaches in nanoparticle oncology research. Ther Deliv 2012; 3: 933–936.
Yang W, Ahmed M, Elian M, Hady el SA, Levchenko TS, Sawant RR et al. Do liposomal apoptotic enhancers increase tumor coagulation and end-point survival in percutaneous radiofrequency ablation of tumors in a rat tumor model? Radiology 2010; 257: 685–696.
Le Pivert PJ, Morrison DR, Haddad RS, Renard M, Aller A, Titus K et al. Percutaneous tumor ablation: microencapsulated echo-guided interstitial chemotherapy combined with cryosurgery increases necrosis in prostate cancer. Technol Cancer Res Treat 2009; 8: 207–216.
Lin X, Gao R, Zhang Y, Qi N, Zhang K, He H et al. Lipid nanoparticles for chemotherapeutic applications: strategies to improve anticancer efficacy. Expert Opin Drug Deliv 2012; 9: 767–781.
Xie H, Goins B, Bao A, Wang ZJ, Phillips WT . Effect of intratumoral administration on biodistribution of 64Cu-labeled nanoshells. Int J Nanomedicine 2012; 7: 2227–2238.
Sim H, Bibee K, Wickline S, Sept D . Pharmacokinetic modeling of tumor bioluminescence implicates efflux, and not influx, as the bigger hurdle in cancer drug therapy. Cancer Res 2011; 71: 686–692.
Sharma B, Peetla C, Adjei IM, Labhasetwar V . Selective biophysical interactions of surface modified nanoparticles with cancer cell lipids improve tumor targeting and gene therapy. Cancer Lett 2013; 334: 228–236.
Fang J, Qin H, Nakamura H, Tsukigawa K, Shin T, Maeda H . Carbon monoxide, generated by heme oxygenase-1, mediates the enhanced permeability and retention effect in solid tumors. Cancer Sci 2012; 103: 535–541.
Zhao W, Zhuang S, Qi XR . Comparative study of the in vitro and in vivo characteristics of cationic and neutral liposomes. Int J Nanomedicine 2011; 6: 3087–3098.
Weibel S, Basse-Luesebrink TC, Hess M, Hofmann E, Seubert C, Langbein-Laugwitz J et al. Imaging of intratumoral inflammation during oncolytic virotherapy of tumors by 19F-magnetic resonance imaging (MRI). PLoS One 2013; 8: e56317.
Hecht JR, Farrell JJ, Senzer N, Nemunaitis J, Rosemurgy A, Chung T et al. EUS or percutaneously guided intratumoral TNFerade biologic with 5-fluorouracil and radiotherapy for first-line treatment of locally advanced pancreatic cancer: a phase I/II study. Gastrointest Endosc 2012; 75: 332–338.
Hanna N, Ohana P, Konikoff FM, Leichtmann G, Hubert A, Appelbaum L et al. Phase 1/2a, dose-escalation, safety, pharmacokinetic and preliminary efficacy study of intratumoral administration of BC-819 in patients with unresectable pancreatic cancer. Cancer Gene Ther 2012; 19: 374–381.
Leifler KS, Svensson S, Abrahamsson A, Bendrik C, Robertson J, Gauldie J et al. Inflammation induced by MMP-9 enhances tumor regression of experimental breast cancer. J Immunol 2013; 190: 4420–4430.
Peng YF, Shi YH, Ding ZB, Zhou J, Qiu SJ, Hui B et al. Alpha-fetoprotein promoter-driven Cre/LoxP-switched RNA interference for hepatocellular carcinoma tissue-specific target therapy. PLoS One 2013; 8: e53072.
Chen Q, Cheng P, Song N, Yin T, He H, Yang L et al. Antitumor activity of placenta-derived mesenchymal stem cells producing pigment epithelium-derived factor in a mouse melanoma model. Oncol Lett 2012; 4: 413–418.
Li H, Nakashima H, Decklever TD, Nace RA, Russell SJ . HSV-NIS an oncolytic herpes simplex virus type 1 encoding human sodium iodide symporter for preclinical prostate cancer radiovirotherapy. Cancer Gene Ther 2013; 20: 478–485.
Hallett MA, Teng B, Hasegawa H, Schwab LP, Seagroves TN, Pourmotabbed T . Anti-matrix metalloproteinase-9 DNAzyme decreases tumor growth in the MMTV-PyMT mouse model of breast cancer. Breast Cancer Res 2013; 15: R12.
Puntel M, AKM GM, Farrokhi C, Vanderveen N, Paran C, Appelhans A et al. Safety profile, efficacy, and biodistribution of a bicistronic high-capacity adenovirus vector encoding a combined immunostimulation and cytotoxic gene therapy as a prelude to a phase I clinical trial for glioblastoma. Toxicol Appl Pharmacol 2013; 268: 318–330.
Huang S, Shao K, Kuang Y, Liu Y, Li J, An S et al. Tumor targeting and microenvironment-responsive nanoparticles for gene delivery. Biomaterials 2013; 34: 5294–5302.
Ramachandran M, Yu D, Wanders A, Essand M, Eriksson F . An infection-enhanced oncolytic adenovirus secreting H. pylori neutrophil-activating protein with therapeutic effects on neuroendocrine tumors. Mol Ther 2013; 21: 2008–2018.
Kasai K, Nakashima H, Liu F, Kerr S, Wang J, Phelps M et al. Toxicology and biodistribution studies for MGH2.1, an oncolytic virus that expresses two prodrug-activating genes, in combination with prodrugs. Mol Ther Nucleic Acids 2013; 2: e113.
Choi IK, Strauss R, Richter M, Yun CO, Lieber A . Strategies to increase drug penetration in solid tumors. Front Oncol 2013; 3: 193.
Govindarajan S, Sivakumar J, Garimidi P, Rangaraj N, Kumar JM, Rao NM et al. Targeting human epidermal growth factor receptor 2 by a cell-penetrating peptide-affibody bioconjugate. Biomaterials 2012; 33: 2570–2582.
Gopal V, Guruprasad K . Structure prediction and validation of an affibody engineered for cell-specific nucleic acid targeting. Syst Synth Biol 2010; 4: 293–297.
Zarogoulidis P, Darwiche K, Krauss L, Huang H, Zachariadis GA, Katsavou A et al. Inhaled cisplatin deposition and distribution in lymph nodes in stage II lung cancer patients. Future Oncol 2013; 9: 1307–1313.
Zarogoulidis P, Petridis D, Ritzoulis C, Darwiche K, Spyratos D, Huang H et al. Establishing the optimal nebulization system for paclitaxel, docetaxel, cisplatin, carboplatin and gemcitabine: back to drawing the residual cup. Int J Pharm 2013; 453: 480–487.
Peiris PM, Bauer L, Toy R, Tran E, Pansky J, Doolittle E et al. Enhanced delivery of chemotherapy to tumors using a multicomponent nanochain with radio-frequency-tunable drug release. ACS Nano 2012; 6: 4157–4168.
Liu Q, Li R, Zhu Z, Qian X, Guan W, Yu L et al. Enhanced antitumor efficacy, biodistribution and penetration of docetaxel-loaded biodegradable nanoparticles. Int J Pharm 2012; 430: 350–358.
Luo X, Xu G, Song H, Yang S, Yan S, Jia G et al. Promoted antitumor activities of acid-labile electrospun fibers loaded with hydroxycamptothecin via intratumoral implantation. Eur J Pharm Biopharm 2012; 82: 545–553.
Hobbs SK, Monsky WL, Yuan F, Roberts WG, Griffith L, Torchilin VP et al. Regulation of transport pathways in tumor vessels: role of tumor type and microenvironment. Proc Natl Acad Sci USA 1998; 95: 4607–4612.
Chauhan VP, Stylianopoulos T, Boucher Y, Jain RK . Delivery of molecular and nanoscale medicine to tumors: transport barriers and strategies. Annu Rev Chem Biomol Eng 2011; 2: 281–298.
Pluen A, Boucher Y, Ramanujan S, McKee TD, Gohongi T, di Tomaso E et al. Role of tumor-host interactions in interstitial diffusion of macromolecules: cranial vs. subcutaneous tumors. Proc Natl Acad Sci USA 2001; 98: 4628–4633.
Peracchia MT, Fattal E, Desmaele D, Besnard M, Noel JP, Gomis JM et al. Stealth PEGylated polycyanoacrylate nanoparticles for intravenous administration and splenic targeting. J Control Release 1999; 60: 121–128.
Choi HS, Liu W, Misra P, Tanaka E, Zimmer JP, Itty Ipe B et al. Renal clearance of quantum dots. Nat Biotechnol 2007; 25: 1165–1170.
Chauhan VP, Popovic Z, Chen O, Cui J, Fukumura D, Bawendi MG et al. Fluorescent nanorods and nanospheres for real-time in vivo probing of nanoparticle shape-dependent tumor penetration. Angew Chem Int Ed Engl 2011; 50: 11417–11420.
Dellian M, Yuan F, Trubetskoy VS, Torchilin VP, Jain RK . Vascular permeability in a human tumour xenograft: molecular charge dependence. Br J Cancer 2000; 82: 1513–1518.
Stylianopoulos T, Soteriou K, Fukumura D, Jain RK . Cationic nanoparticles have superior transvascular flux into solid tumors: insights from a mathematical model. Ann Biomed Eng 2013; 41: 68–77.
Kale AA, Torchilin VP . Environment-responsive multifunctional liposomes. Methods Mol Biol 2010; 605: 213–242.
Wong C, Stylianopoulos T, Cui J, Martin J, Chauhan VP, Jiang W et al. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc Natl Acad Sci USA 2011; 108: 2426–2431.
Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science 2009; 324: 1457–1461.
Ferretti S, Allegrini PR, Becquet MM, McSheehy PM . Tumor interstitial fluid pressure as an early-response marker for anticancer therapeutics. Neoplasia 2009; 11: 874–881.
Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR . Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell 2012; 21: 418–429.
van der Veldt AA, Smit EF, Lammertsma AA . Positron emission tomography as a method for measuring drug delivery to tumors in vivo: the example of [(11)C]docetaxel. Front Oncol 2013; 3: 208.
Zou Y, Tornos C, Qiu X, Lia M, Perez-Soler R . p53 aerosol formulation with low toxicity and high efficiency for early lung cancer treatment. Clin Cancer Res 2007; 13: 4900–4908.
Frederiksen KS, Abrahamsen N, Cristiano RJ, Damstrup L, Poulsen HS . Gene delivery by an epidermal growth factor/DNA polyplex to small cell lung cancer cell lines expressing low levels of epidermal growth factor receptor. Cancer Gene Ther 2000; 7: 262–268.
Kim HW, Park IK, Cho CS, Lee KH, Beck GR Jr, Colburn NH et al. Aerosol delivery of glucosylated polyethylenimine/phosphatase and tensin homologue deleted on chromosome 10 complex suppresses Akt downstream pathways in the lung of K-ras null mice. Cancer Res 2004; 64: 7971–7976.
Gautam A, Densmore CL, Melton S, Golunski E, Waldrep JC . Aerosol delivery of PEI-p53 complexes inhibits B16-F10 lung metastases through regulation of angiogenesis. Cancer Gene Ther 2002; 9: 28–36.
Horev-Drori G, Cooks T, Bittan H, Lazarov E, Schmidt M, Arazi L et al. Local control of experimental malignant pancreatic tumors by treatment with a combination of chemotherapy and intratumoral 224radium-loaded wires releasing alpha-emitting atoms. Transl Res 2012; 159: 32–41.
Ahmed M, Moussa M, Goldberg SN . Synergy in cancer treatment between liposomal chemotherapeutics and thermal ablation. Chem Phys Lipids 2012; 165: 424–437.
Son CH, Shin DY, Kim SD, Park HS, Jung MH, Bae JH et al. Improvement of antitumor effect of intratumoral injection of immature dendritic cells into irradiated tumor by cyclophosphamide in mouse colon cancer model. J Immunother 2012; 35: 607–614.
Raut CP, Boucher Y, Duda DG, Morgan JA, Quek R, Ancukiewicz M et al. Effects of sorafenib on intra-tumoral interstitial fluid pressure and circulating biomarkers in patients with refractory sarcomas (NCI protocol 6948). PLoS One 2012; 7: e26331.
Betting DJ, Hurvitz SA, Steward KK, Yamada RE, Kafi K, van Rooijen N et al. Combination of cyclophosphamide, rituximab, and intratumoral CpG oligodeoxynucleotide successfully eradicates established B cell lymphoma. J Immunother 2012; 35: 534–543.
Lai CY, Fite BZ, Ferrara KW . Ultrasonic enhancement of drug penetration in solid tumors. Front Oncol 2013; 3: 204.
Zhao N, Yang B, Duan YC, Lei R . [Comparative study on five pretreatment methods for ICP-OES determination of mineral elements in Rosa rugosa]. Guang Pu Xue Yu Guang Pu Fen Xi 2011; 31: 2256–2258.
Correa AH, Choi MR, Gironacci M, Aprile F, Fernandez BE . Atrial natriuretic factor decreases renal dopamine turnover and catabolism without modifying its release. Regul Pept 2008; 146: 238–242.
Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Volberding PA, O'Hare AM . Racial differences in end-stage renal disease rates in HIV infection versus diabetes. J Am Soc Nephrol 2007; 18: 2968–2974.
Kim JH, Lee Y, Bae YS, Kim WS, Kim K, Im HY et al. Phase I/II study of immunotherapy using autologous tumor lysate-pulsed dendritic cells in patients with metastatic renal cell carcinoma. Clin Immunol 2007; 125: 257–267.
Jang EY, Lee SO, Choi SH, Sung H, Kim MN, Kim BJ et al. Case of pyomyositis due to Mycobacterium haemophilum in a renal transplant recipient. J Clin Microbiol 2007; 45: 3847–3849.
Ventura A, Meissner A, Dillon CP, McManus M, Sharp PA, Van Parijs L et al. Cre-lox-regulated conditional RNA interference from transgenes. Proc Natl Acad Sci USA 2004; 101: 10380–10385.
Eshita Y, Higashihara J, Onishi M, Mizuno M, Yoshida J, Takasaki T et al. Mechanism of introduction of exogenous genes into cultured cells using DEAE-dextran-MMA graft copolymer as non-viral gene carrier. Molecules 2009; 14: 2669–2683.
Onishi Y, Eshita Y, Murashita A, Mizuno M, Yoshida J . Synthesis and characterization of 2-diethyl-aminoethyl–dextran–methyl methacrylate graft copolymer for nonviral gene delivery vector. J Appl Polym Sci 2005; 98: 9–14.
Bertram JS, Janik P . Establishment of a cloned line of Lewis lung carcinoma cells adapted to cell culture. Cancer Lett 1980; 11: 63–73.
Acknowledgements
PZ would like to thank Kevin Barnard, Medical Isotopes, Inc. for his valuable information throughout the design of the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Baliaka, A., Zarogoulidis, P., Domvri, K. et al. Intratumoral gene therapy versus intravenous gene therapy for distant metastasis control with 2-Diethylaminoethyl-Dextran Methyl Methacrylate Copolymer Non-Viral Vector–p53. Gene Ther 21, 158–167 (2014). https://doi.org/10.1038/gt.2013.68
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2013.68
Keywords
This article is cited by
-
Consideration with “Intratumoral gene therapy versus intravenous gene therapy for distant metastasis control with DDMC non-viral vector–p53”
Gene Therapy (2022)
-
Medicinal facilities to B16F10 melanoma cells for distant metastasis control with a supramolecular complex by DEAE-dextran-MMA copolymer/paclitaxel
Drug Delivery and Translational Research (2015)