Abstract
Vein graft failure caused by neointimal hyperplasia (IH) after coronary artery bypass grafting with saphenous veins is a major clinical problem. The lack of safe and efficient vectors for vascular gene transfer has significantly hindered progress in this field. We have developed a Receptor-Targeted Nanocomplex (RTN) vector system for this purpose and assessed its therapeutic efficacy in a rabbit vein graft model of bypass grafting. Adventitial delivery of β-Galactosidase showed widespread transfection throughout the vein wall on day 7, estimated at about 10% of cells in the adventitia and media. Vein grafts were then transfected with a plasmid encoding inducible nitric oxide synthase (iNOS) and engrafted into the carotid artery. Fluorescent immunohistochemistry analysis of samples from rabbits killed at 7 days after surgery showed that mostly endothelial cells and macrophages were transfected. Morphometric analysis of vein graft samples from the 28-day groups showed approximately a 50% reduction of neointimal thickness and 64% reduction of neointimal area in the iNOS-treated group compared with the surgery control groups. This study demonstrates efficacy of iNOS gene delivery by the RTN formulation in reducing IH in the rabbit model of vein graft disease.
Similar content being viewed by others
Introduction
Although annual mortality rates continue to fall, coronary heart disease remains a major killer with >88 000 deaths in 2008.1 Coronary artery bypass grafting (CABG) is an effective surgical procedure for the treatment of atheromatous narrowing of arteries with almost 23 000 CABG procedures performed in the United Kingdom in 2008.1 The long saphenous vein is the most frequently used bypass conduit in CABG procedures owing to its ability to reach distally placed coronary branches and its easy accessibility.2
Although percutaneous coronary interventions (PCI) are now used in patients with focal narrowing in one or two coronary arteries, bypass grafting remains a mainstay of therapy for severe, diffuse disease, particularly in the elderly and patients with diabetes, two rapidly growing population groups.3 For patients with multi-vessel disease, CABG was associated with lower rates of major adverse cardiac events at 1 year than occurred after PCI with drug-eluting stents.4 However, 15% of vein grafts fail within 1 year, probably due to thrombotic occlusion, and 50% fail within 10 years of surgery.3, 5 Late vein graft failure is associated with neointimal hyperplasia (IH) and accelerated atherosclerosis. IH is associated with graft damage that occurs during vein harvesting and includes vein ischaemia and the acute marked increase in wall stress of arterialised vein grafts.5 Loss of the growth-regulating effects of intact endothelium combined with the release of growth factors and cytokines from activated platelets and macrophages leads to proliferation and migration of medial smooth muscle cells into the intima. Extracellular matrix synthesis and deposition follow, leading to progressive fibrosis and IH, a substrate for accelerated graft atherosclerosis.6 Pharmacological treatments for vein graft failure have been tested in a number of clinical trials, including aggressive treatment with statins to lower cholesterol, which delayed vein graft diseases but did not abolish vein graft atherosclerosis,7 but most other drug treatments have had poor results and so novel therapies, including gene therapy, are under investigation.
Gene therapy strategies for vein graft disease include altering the vein response to injury by retarding the proliferation and migration of the smooth muscle cells and reducing IH.8 Previous approaches have investigated the potential of antisense oligonucleotides to inhibit genes associated with cell division9, 10, 11, 12 and oligonucleotide promoter decoys, which block the pivotal transcription factor E2F.13 Gene transfer in animal models of vein graft disease has also been evaluated for prevention of IH using genes for nitric oxide synthase (NOS), tissue inhibitors of metalloproteinases (TIMP-1, -2 and -3), and vascular endothelial growth factor.9 More recently, other genes have been tested, including genes for NogoB in a pig vein graft model14 and Cox-1 in a rabbit model.15
Adenoviral vectors demonstrate high efficiency of gene transfer and expression in vein grafts but were shown to induce a strong host immuno/inflammatory response in rabbit vein grafts, which exacerbates neointimal formation, limits the duration of transgene expression and the efficacy of vector re-administration.16, 17 Non-viral liposomes have been investigated as alternatives to adenoviral vectors, but they displayed poor transfection efficiency in vessel walls with typical reports of 0.05% for Lipofectin relative to 10% for adenoviral vectors.18 We have recently described a novel non-viral vector formulation termed a Receptor-Targeted Nanocomplex (RTN), which displayed efficient transfection of vascular tissues, with extended duration of expression.19
In this study, we have now investigated the potential of this delivery formulation for gene therapy of IH in a surgical model of vein graft disease in rabbits. Jugular vein segments were transfected by adventitial treatment of vein grafts with RTN formulations ex vivo with a β-galactosidase reporter gene or the cDNA for inducible nitric oxide synthase (iNOS), a treatment that was effective in previous studies for this purpose using adenoviral vectors.20 Adventitial, rather than luminal delivery, was adopted to minimise damage to the luminal surfaces during the transfection procedure, reducing the risks of thrombosis and of distribution to other tissues via the circulation through either vector or cell shedding. In addition, luminal delivery leads to endothelial transfection, and it is well established that endothelial cells are lost due to damage in the first days after surgery, thus limiting the potential for therapeutic gene expression. Transfected vein grafts were analysed at 7 days for evidence of transgene expression and to identify cell types transfected by RTNs by co-localisation with cell surface markers. In the 28-day vein graft samples, morphometric analysis was performed to assess effects of iNOS transfection on the development of IH.
Results
Efficiency of vein graft transfection with the reporter gene, β-galactosidase
Rabbit vein segments were transfected with a nuclear-localising β-Galactosidase reporter gene before engraftment. Seven days after surgery, the rabbits were killed and veins retrieved for X-gal staining. Regions of transfected vein grafts displayed the blue pigment in contrast to the pale untransfected adjacent arterial parts at both ends (Figure 1a). Microscopically, there were extensive areas of transfection with most transfected cells located in the adventitial and medial regions, which were difficult to differentiate due to loss of the external elastic lamina, but also some scattered cells in the intima (Figure 1b), on the luminal side of the inner elastic lamina (IEL). Under higher magnification, specific cell association of X-Gal staining was observed (Figure 1c). By contrast, the control plasmid (pCI) transfected vein grafts showed no X-Gal staining (Figure 1d).
X-Gal staining of 7-day vein graft samples. (a) Gross sample of vein graft transfected with β-Gal. The portion between the outer black sutures (arrowed) is the vein graft. The inner arrow points to the suture for the branch off the jugular vein. Positive (blue) X-Gal staining was contrasted with the pale colour of adjacent untransfected arterial portions at both ends. (b) X-Gal staining of β-Gal-transfected 7-day vein graft section. Blue, X-Gal-positive cells were abundant across the adventitia with some in the intima. (c) View of higher magnification of the highlighted area in (b). (d) X-Gal staining on control plasmid pCI-transfected vein graft. Images are representatives of three samples in each group. A, adventitia and peri-adventitia; I, intimal layer; Lu, lumen; M, medial layer. Bars=100 μm.
Expression of therapeutic genes
Vein grafts were transfected with RTN-iNOS formulations ex vivo, then examined 7 days later by immunohistochemistry of tissue sections for iNOS protein and by reverse transcriptase–PCR (RT-PCR) for mRNA. iNOS (Figure 2a) expression was observed in sections in the same regions as the transfected β-galactosidase expression, that is, predominantly in the adventitial and medial region with a few cells in the intimal layers, while negative controls transfected with pCI were predominantly negative for staining (Figure 2b). Human iNOS expression was detected by RT-PCR in the vein graft samples by ethidium bromide-stained agarose gel electrophoresis of mRNA-derived cDNA, whereas no iNOS cDNA was detected in samples derived from the liver, lung, kidney and testis of the same animal (Figure 2c).
Transfected iNOS activity in vein graft samples 7 days after transfection. (a) Immunoreactivity for iNOS, in brown colour, was detected abundantly in adventitia (A) and in scattered cells in the media (M) and intima (I) either side of the IEL of iNOS-transfected samples. (b) The same antibody did not reveal any positive cells in pCI-transfected samples. Bars=100 μm. (c) RT-PCR detection of the expression of transgene iNOS from 7-day vein graft samples as well as samples of liver, lung, kidney and testis collected from the same rabbit. Bands for iNOS were detected in vein graft samples (arrowed) but not in the organ samples. Bands were observed for the control gene GAPDH from each sample.
Biodistribution of the vector
DNA was extracted from samples of the lung, kidney, liver and testis, as well as vein grafts collected 7 days after transfection with the RTN vector formulation to assess the biodistribution of the vector DNA component. Organ samples were subjected to analysis by PCR amplification of plasmid DNA to assess the distribution of the iNOS gene construct. On agarose gels, a clear band for PCR-amplified iNOS was observed from vein graft samples but no iNOS band was detected in any of the four organ samples analysed under the same conditions, supporting the proposal that plasmid would only be present at very low levels in other organs (Figure 3).
PCR assessment of distribution of plasmid DNA containing the iNOS gene in the organ samples collected 7 days after transfection from liver, lung, kidney and testis displayed in parallel with reaction product for the GAPDH gene. The 7-day vein graft sample (V-graft) and iNOS plasmid (+ve) were used as positive controls. Reaction with no DNA template was included as a negative control (−).
Histomorphometry analysis
Morphometric analysis was performed on transverse vein graft sections from surgery control, plasmid control and iNOS-transfected rabbits stained by the Elastic van Gieson method, with the neointima detected as a grey layer inside the IEL (Supplementary Figure S1). Measurements were performed to determine both the thickness of the neointima (I) relative to the medial (M) thickness of each vein graft (I/M) (Figure 4a) and the neointimal area (mm2) (Figure 4b).
Morphological comparison of neointima formation in the different groups, including surgery control, pCI plasmid control and iNOS treated. (a) Chart showing the values for the ratio of thickness of the neointima (I) to medial layer (M) for each group (I/M). (b) Chart showing the values for area (mm2) of the neointimal layer.
The mean I/M ratio in the iNOS-treated group was reduced by 49% (P<0.05) compared with the surgery group and by 58% (P<0.001) compared with the pCI plasmid control group (Table 1). The mean neointimal area for the iNOS-treated group was 64% (P<0.05) less than that for the surgery group and 74% (P<0.001) lower than the pCI group. Differences between the surgery and plasmid control groups for both I/M and neointimal area values were not statistically significant.
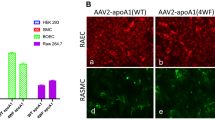
Characterisation of iNOS-positive cells
As iNOS transfection induced a significant inhibitory effect on IH, iNOS-positive cells were then characterised by double immunofluorescent and DAPI (4,6-diamidino-2-phenylindole) staining to identify transfected cell types and localisation within the vein graft. Following immunostaining with monoclonal anti-iNOS, vein graft sections were labelled with DAPI and one of the three other antibodies, including CD31 (endothelial cells, Figure 5a), RAM11 (macrophage, Figure 5b) and HHF35 (anti-smooth muscle actin, Figure 5c). Cells staining for iNOS were located in both adventitial, medial and intimal layers (Figures 5a–c), as also shown in Figure 2, and were co-stained predominantly with anti-CD31 (Figure 5a), with less extensive colocalisation with RAM11 (Figure 5b) and rarely with the anti-smooth muscle actin marker (Figure 5c). Further characterisation of the endothelial nature of transfected cells was performed by staining with anti-CD34 (Supplementary Figure S2), which stains endothelial progenitor cells,21 reported previously to be abundant in the adventitia of mouse vein grafts.22 Here it was shown that CD34 immuno-reactivity also co-localised with iNOS in adventitial, medial and intimal cells (Supplementary Figure S2A), with a similar distribution to CD31-positive cells. In addition, staining for CD31 and CD34 (Supplementary Figure S2B) showed that these endothelial cells expressed simultaneously both CD31 and CD34.
Double immunofluorescent characterisation of iNOS-positive cells in 7-day vein graft samples. Immunostaining using first-layer antibodies is shown in green for iNOS (a–c). Second-layer antibodies were labelled in red for CD31 on endothelial cells (a), RAM11 for macrophages (b) and HHF35 for smooth muscle actin (c). Overlapping staining was revealed by yellow fluorescence. DAPI staining (blue) was performed to detect cell nuclei (a–c). L, lumen. Bars=46.54 μm in (a) and (b), =47.62 μm in (c).
Further immunohistochemical analysis of the 7-day iNOS-transfected vein grafts revealed that the endothelial marker, CD31, stained strongly in the vasa vasorum in the periadventitial area as well as cells on either side of the IEL in the medial layer and basal area of the intima (Figure 6a). Apparent staining of the IEL is probably due to accumulated CD31+ve cells on either side of the IEL. Very little intimal CD31 staining at the luminal boundary was observed in 7-day samples, typical of the early stage loss of endothelium in this vein graft model. The 28-day samples, however, showed strong CD31 immunostaining along the endothelial surface on iNOS-transfected vein grafts (Figure 6b), indicating the endothelial regrowth typical of the process of vein graft recovery and adaptation. CD31 staining of cells in the medial and basal intimal areas staining was also much lower at day 28 than at day 7 and consequently the apparent staining of the IEL itself was also reduced.
Discussion
Gene therapy is an attractive therapeutic strategy to prolong the survival of saphenous grafts by administering genes that reduce the IH that occurs in vein grafts in the weeks following surgery.23 The key events leading to IH and remodelling are the proliferation and migration of vascular smooth muscle cells and excessive connective tissue metabolism.24 Gene therapy is under investigation for prevention of IH following post-vein graft surgery, and most strategies target one or more of these key pathological processes.23 Gene delivery to vein grafts remains a major challenge to the development of gene therapy for CABG.
Although adenoviral vectors have shown promise in a number of preclinical vascular gene therapy studies, non-viral vectors offer an alternative approach with beneficial properties relating to vector immunogenicity, safety and simplicity. We are developing novelRTN formulations of cationic liposomes and targeting peptides for vascular gene transfer. One RTN formulation was used to deliver the gene for TIMP-1 adventitially to carotid artery segments after angioplasty in a rat model of restenosis, demonstrating efficient transfection and a reduction of IH by approximately 40% at 28 days after treatment.25 A second generation RTN vector was then developed containing an optimised targeting peptide and lipid components, which substantially increased the transfection efficiency of rabbit vascular tissue ex vivo.19 The aim of the present study was to investigate the therapeutic potential of the RTN formulation for IH by delivering the iNOS gene to vein segments in a rabbit model of vein graft disease.
Adenoviral vectors delivering iNOS was reported previously to be effective in the rabbit vein graft model after delivery.26 Nitric oxide (NO), produced by iNOS, and other nitric oxide synthases, in a reaction involving arginine, oxygen and NADPH, is a powerful intracellular and extracellular signalling molecule and it can diffuse out of the cells where it is produced, potentially spreading the effects of iNOS beyond the cells that are directly transfected. Increased NO levels in vein graft tissues would help to restrict the development of IH by promoting endothelial cell growth and survival, inhibition of vascular smooth muscle cell proliferation and migration, inhibition of platelet adherence and leukocyte chemotaxis.20, 27 All three NOS isoforms have been transferred into blood vessels for various vascular disorders but iNOS is often preferred as it generates >100-fold higher levels of NO than the constitutive isoforms, endothelial NOS and neuronal NOS.27 Clinical gene therapy trials are in progress for in-stent restenosis, with the iNOS gene delivered by a lipoplex.28, 29
Vein graft transfection during bypass grafting surgery offers the advantage of tissue accessibility as there is a period, typically of up to 30 min, where the extracted saphenous vein segment is awaiting engraftment, which provides a window of opportunity for transfection incubations under controlled conditions for optimal efficiency, while seamlessly integrating with the surgical procedure. Further, it has been shown that even transient gene expression lasting a few days can have long-term, persistent beneficial effects in reducing IH, for at least 3 months in a porcine vein graft model30 and probably longer. This can be explained by the endothelial regrowth that usually occurs within 7–14 days after surgery stabilising the graft. One of the key underlying principles of vascular gene therapy is that transient gene expression correlates conveniently with the kinetics of graft self-repair processes, and by its transient nature, once expression of the therapeutic transgene has decayed, longer term remodelling processes may proceed enabling the thin-walled vein graft to adapt to the higher arterial blood pressure.
We have shown previously that the RTN formulation transfects rabbit arterial explants efficiently, with transgene expression peaking at 5 days but persisting for at least 10 days, which, therefore, is within the required therapeutic window.19 Here we have shown that both β-galactosidase and iNOS gene activity was readily detectable for at least 7 days after transfection. We would not expect to detect significant levels of transgene expression at 28 days, and so that was not tested in these studies with either β-galactosidase or iNOS. In future studies, it will be interesting to investigate gene expression kinetics in engrafted vein segments and possible benefits of prolonging expression.
The choice of vector is likely to be critical for the efficacy of gene therapy for CABG. Adenoviral vectors have displayed high efficiencies of gene transfer in rabbit vein grafts but studies have also revealed the induction of inflammatory responses, with recruitment of white cells and expression of endothelial adhesion molecules leading to rapid loss of transgene expression within 2 weeks of transduction31, 32 and stimulation of IH.16 In addition, adenoviral immunogenicity may limit efficacy of treatment in patients pre-exposed to adenovirus, and of re-administered vector, should it be required. Although an adenoviral study in pigs did not reveal inflammation at 3 months after saphenous vein transduction and engraftment,30 the potential for adenoviral induction of inflammation remains a cause for concern in clinical applications.
Non-viral vectors offer potential advantages of safety and ease of use over adenoviral vectors. Although a number of liposomal vectors have only displayed low levels of transfection,33 other non-viral approaches have shown more promise in preclinical studies of vascular gene transfer. For example, a fractured dendrimer formulation achieved a transfection efficiency of about 4% in adventitial and medial cells by adventitial delivery, similar to adenoviral levels of transduction in the same study.34 Delivery of TIMP3 plasmid by ultrasonic exposure of porcine vein grafts led to increased luminal capacity at 28 days after surgery.35 Adventitial delivery of endothelial NOS by electroporation of rabbit vein grafts successfully limited IH 28 days after grafting.36 Thus, non-viral transfection methods remain a promising area of research for vascular gene therapy.
Histological and morphometric analysis of vein grafts transfected with the RTN iNOS formulation was performed 28 days after transfection and engraftment. The iNOS-treated group displayed a 49% reduction in the thickness of the neointima relative to the media (I/M ratio) and 64% reduction of neointimal area compared with the untreated surgery control. Other studies using adenovirus-expressing neuronal NOS showed a similar reduction of the I/M ratio of 50% in 28-day vein grafts,37 while an adenovirus-expressing human iNOS produced a 40% reduction of the I/M ratio at 21 days in a porcine vein graft model.26 Thus, the effect on neointimal development of treatment with the RTN expressing iNOS was comparable to that of adenoviral vectors expressing NOS genes, supporting the proposal that the RTN formulation described in this paper may offer an effective, non-viral alternative to adenoviral vectors.
The vein grafts treated with control plasmids showed no significant increase in neointimal thickness, which contrasts with control adenoviral vectors that enhance neointimal development, but more detailed future studies will be required to investigate in more detail the immuno-inflammatory responses to RTN administration. The RTN vector formulation may be improved in this regard by using plasmid DNA constructs in which cytidine-phosphate-guanosine motifs have been removed as they are known to activate antigen-presenting cells via the Toll-like receptor-9.38
In this study, we elected to transfect the adventitial surface of the vein graft rather than the luminal surface as endothelial intimal cells are shed rapidly from vein grafts after surgical engraftment, leading to loss of transgene expression along with the cells. β-galactosidase and iNOS gene expression were observed abundantly on either side of the IEL, in the adventitial, medial and intimal regions of the vein segments. This was consistent with previous studies using viral and non-viral vectors to transduce rabbit carotid artery samples from a silastic collar around the adventitial surface where transduction was also predominantly adventitial with some transduced medial and intimal cells too.34 Cells in the medial and intimal layers were presumably transfected by vector particles penetrating the tissue, or could be transfected adventitial cells that migrated there. From this study, it is not possibe to determine which is the case.
PCR analysis for plasmid biodistribution and RT-PCR analysis of INOS gene expression confirmed that both transgene expression and plasmid distribution were confined to the vein graft segments and were undetectable in other tissues (liver, lung, kidney, testis).
Interestingly, adventitial delivery led to the appearance of transfected cells in the adventitia, periadventitia, media and neointima. It has emerged in recent years that the adventitia has an important role in vascular development, repair and disease.39 The adventitia contains a number of resident stem cell and progenitor cell types40 and contains an active vasculature, the vasa vasorum, that maintains the medial layer and provides a conduit for migrating leukocytes and macrophages. The major cell types transfected by RTNs in all the regions of the saphenous vein wall were predominantly endothelial cells and macrophages. The iNOS-positive cells also co-expressed CD34 (CD34+), a cell-surface marker of endothelial progenitor cells, and CD34 colocalised with CD31 suggesting that endothelial progenitor cells were transfected. Interestingly, macrophages were the other major cell type expressing iNOS and it has been reported that the level of iNOS expressed in macrophages and smooth muscle cells correlated directly with endothelial progenitor cell–mediated graft repair.41 The potential for iNOS-transfected macrophages and endothelial progenitor cells to limit IH is an intriguing possibility that will require further investigation.
In summary, we have described a novel, non-viral vector formulation that achieves efficient transfection of vein segments transfected by immersion for as little as 20 min. The adventitial route of delivery resulted in transfection predominantly of endothelial lineage cells and macrophages throughout the vessel wall, and this had beneficial effects on the development of IH. Further studies will be required into the use of RTN-mediated transfection with iNOS and other genes to assess their effects on the biology of the vein graft relating to inflammation, progenitor cell migration and IH. Further safety and efficacy studies will also be required into the long-term benefits of this treatment and the health of treated vein grafts.
Materials and methods
Preparation of plasmid DNA
Plasmids used in this study included the eukaryotic expression vector pCI (Promega, Southampton, UK), the β-galactosidase reporter gene vector pAB1125 and the iNOS expressing plasmid pcDNA3-iNOS (a generous gift from Richard Shapiro, University of Pittsburgh, USA). All plasmids utilised the cytomegalovirus promoter.
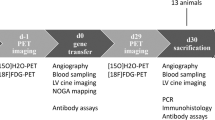
Animals
Male New Zealand white rabbits (3.0–3.5 kg) were maintained on standard rabbit chow. Twenty-two rabbits were divided into three groups according to different gene transfer treatments: (1) iNOS (n=7); (2) pCI control (n=8); and (3) surgery procedure control (n=7). Animals were maintained for 28 days after surgery and gene transfer, then killed for analysis of vein grafts and other tissues. To assess transgene expression, vein graft samples from a further 15 rabbits in the same three groups (n=5 in each group) were killed on day-7 post-surgery for tissue analysis. A further three rabbits were treated with the β-galactosidase reporter gene, which were killed at 7 days and processed for X-gal staining.
Vein graft surgery
The rabbits were anaesthetised by intramuscular injection of Hypnorm and maintained under anaesthesia with inhaled halothane (0.5∼1%) through a facial mask. Heparin (1000 units) was routinely given through the ear vein. The jugular-carotid vein graft surgery was performed using a cuffed, end-to-end anastomosis technique42 with minor modifications. Briefly, a 3.0-cm segment of left external jugular vein was isolated and harvested with both ends ligated using a 6-0 silk, and the jugular vein branch also removed and sutured, then transfected ex vivo for 30 min. After transfection and removal of the ligation sutures on both ends, the vein fragment was rinsed in normal saline; each end was passed through a polymer cuff (made from a 4-F introducer sheath), everted, and fixed with a piece of 8-0 silk suture. The left common carotid artery was then temporarily ligated with clips and cut open 2 cm longitudinally. The cuffed vein ends were inserted into the artery and secured with 6-0 sutures. The arterial clips were removed and the blood flow was re-established (Supplementary Figure S3). The animals were maintained until the harvest day of vein graft samples on day 7 or day 28. Aseptic techniques were maintained throughout the surgery procedures. The rate of occlusions was approximately one in seven procedures. There were no deaths.
Transfection of vein grafts
Gene transfer was performed by incubating the vein graft ex vivo in a normal saline solution of the RTN vector containing plasmid DNA. The RTN vector was composed of the cationic liposome Lipofectin (Invitrogen, Paisley, UK), which is a 1:1 formulation of the cationic lipid DOTMA and the neutral, fusogenic lipid DOPE, a peptide (Peptide-Y: K16GACYGLPHKFCG), and plasmid DNA in a weight ratio of 0.75:4:1 (Lipid:Peptide:DNA). The formulation was prepared in 1 ml saline containing 50 μg of plasmid DNA, 200 μg of peptide K16GACYGLPHKFCG and 37.5 μg of Lipofectin, then left at room temperature for 30 min to allow complex formation. The vein graft was immersed in the RTN solution for 30 min at room temperature, to mimic the clinical situation, and then rinsed in saline before being surgically interposed to the left carotid artery.
Sample harvest
The animals were killed with an overdose of sodium pentobarbital plus exsanguination. Animals were injected through the ear vein with a mixture of heparin (1000 units) and sodium pentobarbital (100 mg kg−1) followed by exsanguination from the abdominal aorta. The vein graft samples were collected and flushed thoroughly through the lumen with normal saline. Each sample was divided into two equal portions. The caudal halves of all the samples were immersion-fixed in 2% paraformaldehyde (PFA) for 30 min and embedded in OCT (optimal cutting temperature) for immunohistochemistry, while the cranial halves of the 28-day samples were immersion-fixed in 4% PFA for 6 h and made into paraffin blocks for histomorphometry analysis. The cranial halves of the 7-day samples were snap-frozen in liquid nitrogen and stored at −80 °C for molecular (PCR and RT-PCR) analysis. For biodistribution analysis of the plasmid DNA, organ samples (lung, liver, kidney and testis) from 7-day animals were collected and snap-frozen in liquid nitrogen and stored at −80 °C.
X-Gal staining
Vein graft samples transfected with pAB11 were fixed in 2% PFA for 20 min and stained in X-Gal (5-bromo-4-chloro-3-indolyl-β-D-galactopyranoside) solution for 2 h. They were then embedded in OCT, cut into 10 μm sections and stained in X-Gal solution for another 16 h followed by counterstaining with nuclear fast red reagent. The peri-nuclear, dark-blue pigmentation indicated transfected cells.
Histomorphometry analysis
Five consecutive paraffin sections, each 5 μm thick at 30 μm intervals, were cut from each of the 28-day vein graft samples and were stained by the Elastic van Gieson method.43 Regions for analysis selected were located away from the sutured ends, to avoid effects of surgical tissue damage and to focus on effects of transgene expression on IH. Microscopic images from each section were captured using OpenLab software (Perkin Elmer, Fremont, CA, USA). Histomorphometry analysis was performed using LaserPix software (Bio-Rad Laboratories, Hemel Hempstead, UK). The thickness of each section was measured at eight points around the circumference at approximately 45-degree intervals. The area of the neointima was calculated by subtracting the luminal area from the area within the internal elastic lamina. Measurements from five consecutive sections were averaged to form the parameters of each case.
Immunohistochemistry and immunofluorescence
Cryostat sections of 10 μm thickness were stained with the avidin-biotinylated-peroxidase complex (ABC) method as described previously.44 Briefly, endogenous peroxidase was inactivated with 0.3% hydrogen peroxide in methanol and the non-specific binding was blocked with 3% normal horse serum. Sections were incubated with the primary antibody overnight at 4 °C. After incubation with biotinylated anti-mouse or anti-goat immunoglobulin G (IgG) and freshly prepared ABC reagent (Vector Labs, Peterborough, UK), slides were developed in DAB (3,3′diaminobenzidine) solution (Sigma-Aldrich, Dorset, UK) and counterstained with haematoxylin. The control slides were stained as above with the primary antibody being replaced with non-specific rabbit IgG (isotype control) and phosphate-buffered saline (blank control), respectively.
For immunofluorescent staining, the ‘Mouse On Mouse’ staining procedure was performed using the M.O.M. Immunodetection Kit (Vector Labs, Peterborough, UK) according to the manufacturer’s modified protocol. Briefly, sections were incubated with the first primary antibody overnight at 4 °C. Following incubation with biotinylated horse anti-mouse IgG, and Fluorescein-Avidin reagent, the sections were incubated with Avidin, Biotin reagents and the mouse Ig blocking reagent to prevent the interaction between the first and second sets of these labelling reagents and antibodies. The sections were then labelled with the second primary antibody overnight, followed by the biotinylated horse anti-mouse IgG, Texas Red-Avidin reagent and DAPI nuclear counterstaining. Antibodies used in this study included mouse anti-CD31 (Dako Cytomation, Cambridgeshire, UK), mouse anti-macrophage (clone RAM11, Dako), mouse anti-muscle actin (clone HHF35, Dako) and mouse anti-iNOS (Santa Cruz Biotechnology, Santa Cruz, CA, USA).
PCR
DNA was extracted from tissues by the Tri-Reagent procedure (Sigma-Aldrich, Gillingham, UK). The templates were amplified with 0.5 μmol l−1 specific primers, 0.025 mmol l−1 deoxyribonucleotide triphosphates, 10 mmol l−1 Tris–HCl at pH 9.0, 50 mmol l−1 KCl, 1.5 mmol l−1 MgCl2, 0.1% Triton X-100 and 2.5 U Taq DNA polymerase (Bioline, London, UK) in a volume of 50 μl. The primer sequences for GAPDH (glyceraldehyde 3-phosphate dehydrogenase) were; forward 5′-CCCTTCATTGACCTCAACTACATGG-3′ and reverse 5′-AGTCTTCTGGGTGGCAGTGATGG-3′, producing a 458 bp signal. Primers for iNOS were; forward 5′-CGG TGC TGT ATT TCC TTA CGA GGC GAA GAA GG-3′ and reverse 5′-GGT GCT GCT TGT TAG GAG GTC AAG TAA AGG GC-3′, which produced a product of 257 bp. The amplification followed the cycle of 0.5 min at 94 °C, 1 min at 58 °C and 2 min at 72 °C. The reaction proceeded for 40 cycles of PCR for detection purposes. The amplification products were size-fractionated by electrophoresis on a 2% (wt/vol) agarose gel (run at 100 V for 1 h), then photographed using a gel documentation system (Uvitec, Glasgow, UK).
RNA extraction, reverse transcription and RT-PCR
Total cellular RNA was isolated from tissues using the Tri-Reagent procedure (Sigma-Aldrich, Gillingham, UK). Samples of total cellular RNA were treated with DNase (Turbo DNA RNAse-free, Ambion, Warrington, UK) before cDNA synthesis. Reverse transcription was performed with 1 μg total cellular RNA and 5 μmol l−1 random hexanucleotide primers (Invitrogen). Mixtures were incubated at 70 °C for 5 min, cooled on ice before the addition of 50 mmol l−1 Tris–HCl at pH 8.3, 75 mmol l−1 KCl, 3 mmol l−1 MgCl2, 10 mmol l−1 dithiothreitol, 10 U RNasin (Invitrogen), 0.125 mmol l−1 deoxyribonucleotide triphosphates and 200 U Superscript III Moloney murine leukaemia virus reverse transcriptase (Invitrogen) in a total volume of 20 μl, followed by a further incubation at 37 °C for 1 h. PCR analysis of the cDNA was performed as above except that 25 cycles were required as these conditions were in the exponential phase of amplification and, therefore, provided correlation between the amount of products and the RNA template abundance in the samples. Agarose gel electrophoresis was performed as above.
Statistical analysis
Data are expressed as means±s.d. Differences between the two groups were compared by analysis of variance with post analysis by the Bonferroni’s test.
References
Scarborough P, Bhatnagar P, Wickramisinghe K, Smolina K, Mitchell C, Rayner M . Coronary Heart Disease Statistics. Oxford, UK, 2010.
Izzat MB, West RR, Bryan AJ, Angelini GD . Coronary artery bypass surgery: current practice in the United Kingdom. Br Heart J 1994; 71: 382–385.
Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, Folliguet T et al. Guidelines on myocardial revascularization. Eur J Cardiothorac Surg 2010; 38 (Suppl): S1–S52.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. New Engl J Med 2009; 360: 961–972.
Motwani JG, Topol EJ . Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 1998; 97: 916–931.
Ip JH, Fuster V, Badimon L, Badimon J, Taubman MB, Chesebro JH . Syndromes of accelerated atherosclerosis: role of vascular injury and smooth muscle cell proliferation. J Am Coll Cardiol 1990; 15: 1667–1687.
Campeau L, Hunninghake DB, Knatterud GL, White CW, Domanski M, Forman SA et al. Aggressive cholesterol lowering delays saphenous vein graft atherosclerosis in women, the elderly, and patients with associated risk factors. NHLBI post coronary artery bypass graft clinical trial. Post CABG Trial Investigators. Circulation 1999; 99: 3241–3247.
Rissanen TT, Yla-Herttuala S . Current status of cardiovascular gene therapy. Mol Ther 2007; 15: 1233–1247.
Mann MJ . Gene therapy for vein grafts. Curr Cardiol Rep 2000; 2: 29–33.
Mannion JD, Ormont ML, Shi Y, O'Brien JEJ, Chung W, Roque F et al. Saphenous vein graft protection: effects of c-myc antisense. J Thorac Cardiovasc Surg 1998; 115: 152–161.
Mannion JD, Ormont ML, Magno MG, O'Brien JE, Shi Y, Zalewski A . Sustained reduction of neointima with c-myc antisense oligonucleotides in saphenous vein grafts. Ann Thorac Surg 1998; 66: 1948–1952.
Shi Y, O'Brien JEJ, Mannion JD, Morrison RC, Chung W, Fard A et al. Remodeling of autologous saphenous vein grafts. The role of perivascular myofibroblasts. Circulation 1997; 95: 2684–2693.
Mann MJ, Whittemore AD, Donaldson MC, Belkin M, Conte MS, Polak JF et al. Ex-vivo gene therapy of human vascular bypass grafts with E2F decoy: the PREVENT single-centre, randomised, controlled trial. Lancet 1999; 354: 1493–1498.
Kritz AB, Yu J, Wright PL, Wan S, George SJ, Halliday C et al. In vivo modulation of Nogo-B attenuates neointima formation. Mol Ther 2008; 16: 1798–1804.
Eichstaedt HC, Liu Q, Chen Z, Bobustuc GC, Terry T, Willerson JT et al. Gene transfer of COX-1 improves lumen size and blood flow in carotid bypass grafts. J Surg Res 2010; 161: 162–167.
Newman KD, Dunn PF, Owens JW, Schulick AH, Virmani R, Sukhova G et al. Adenovirus-mediated gene transfer into normal rabbit arteries results in prolonged vascular cell activation, inflammation, and neointimal hyperplasia. J Clin Invest 1995; 96: 2955–2965.
Yla-Herttuala S, Martin JF . Cardiovascular gene therapy. Lancet 2000; 355: 213–222.
Laitinen M, Pakkanen T, Donetti E, Baetta R, Luoma J, Lehtolainen P et al. Gene transfer into the carotid artery using an adventitial collar: comparison of the effectiveness of the plasmid-liposome complexes, retroviruses, pseudotyped retroviruses, and adenoviruses. Hum Gene Ther 1997; 8: 1645–1650.
Irvine SA, Meng QH, Afzal F, Ho J, Wong JB, Hailes HC et al. Receptor-targeted nanocomplexes optimized for gene transfer to primary vascular cells and explant cultures of rabbit aorta. Mol Ther 2008; 16: 508–515.
Barbato JE, Tzeng E . iNOS gene transfer for graft disease. Trends Cardiovasc Med 2004; 14: 267–272.
Osawa M, Hanada K-I, Hamada H, Nakauchi H . Long-term lymphohematopoietic reconstiitution by a single CD34-low/negative hematopoietic stem cell. Science 1996; 273: 242–245.
Hu Y, Zhang Z, Torsney E, Afzal AR, Davison F, Metzler B et al. Abundant progenitor cells in the adventitia contribute to atherosclerosis of vein grafts in ApoE-deficient mice. J Clin Invest 2004; 113: 1258–1265.
Wan S, George SJ, Berry C, Baker AH . Vein graft failure: current clinical practice and potential for gene therapeutics. Gene Therapy 2012; 19: 630–636.
Strauss BH, Chisholm RJ, Keeley FW, Gotlieb AI, Logan RA, Armstrong PW . Extracellular matrix remodeling after balloon angioplasty injury in a rabbit model of restenosis. Circ Res 1994; 75: 650–658.
Meng QH, Jamal W, Hart SL, McEwan JR . Application to vascular adventitia of a nonviral vector for TIMP-1 gene therapy to prevent intimal hyperplasia. Hum Gene Ther 2006; 17: 717–727.
Kibbe MR, Tzeng E, Gleixner SL, Watkins SC, Kovesdi I, Lizonova A et al. Adenovirus-mediated gene transfer of human inducible nitric oxide synthase in porcine vein grafts inhibits intimal hyperplasia. J Vasc Surg 2001; 34: 156–165.
McCarthy HO, Coulter JA, Robson T, Hirst DG . Gene therapy via inducible nitric oxide synthase: a tool for the treatment of a diverse range of pathological conditions. J Pharm Pharmacol 2008; 60: 999–1017.
Muhs A, Heublein B, Schletter J, Herrmann A, Rudiger M, Sturm M et al. Preclinical evaluation of inducible nitric oxide synthase lipoplex gene therapy for inhibition of stent-induced vascular neointimal lesion formation. Hum Gene Ther 2003; 14: 375–383.
Leyen, von der HE, Mugge A, Hanefeld C, Hamm CW, Rau M, Rupprecht HJ et al. A prospective, single-blind, multicenter, dose escalation study of intracoronary iNOS lipoplex (CAR-MP583) gene therapy for the prevention of restenosis in patients with de novo or restenotic coronary artery lesion (REGENT I extension). Hum Gene Ther 2011; 22: 951–958.
George SJ, Wan S, Hu J, MacDonald R, Johnson JL, Baker AH . Sustained reduction of vein graft neointima formation by ex vivo TIMP-3 gene therapy. Circulation 2011; 124: S135–S142.
Channon KM, Qian HS, Youngblood SA, Olmez E, Shetty GA, Neplioueva V et al. Acute host-mediated endothelial injury after adenoviral gene transfer in normal rabbit arteries: impact on transgene expression and endothelial function. Circ Res 1998; 82: 1253–1262.
Channon KM, Qian H, Neplioueva V, Blazing MA, Olmez E, Shetty GA et al. In vivo gene transfer of nitric oxide synthase enhances vasomotor function in carotid arteries from normal and cholesterol-Fed rabbits. Circulation 1998; 98: 1905–1911.
Bowey K, Tanguay JF, Tabrizian M . Liposome technology for cardiovascular disease treatment and diagnosis. Expert Opin Drug Deliv 2012; 9: 249–265.
Turunen MP, Hiltunen MO, Ruponen M, Virkamaki L, Szoka FCJ, Urtti A et al. Efficient adventitial gene delivery to rabbit carotid artery with cationic polymer-plasmid complexes. Gene Therapy 1999; 6: 6–11.
Akowuah EF, Gray C, Lawrie A, Sheridan PJ, Su C-H, Bettinger T et al. Ultrasound-mediated delivery of TIMP-3 plasmid DNA into saphenous vein leads to increased lumen size in a porcine interposition graft model. Am J Physiol Heart Circ Physiol 2005; 12: 1154–1157.
Yamaoka T, Yonemitsu Y, Komori K, Baba H, Matsumoto T, Onohara T et al. Ex vivo electroporation as a potent new strategy for nonviral gene transfer into autologous vein grafts. Am J Physiol Heart Circ Physiol 2005; 289: H1865–H1872.
West NE, Qian H, Guzik TJ, Black E, Cai S, George SE et al. Nitric oxide synthase (nNOS) gene transfer modifies venous bypass graft remodeling: effects on vascular smooth muscle cell differentiation and superoxide production. Circulation 2001; 104: 1526–1532.
Krieg AM . CpG motifs in bacterial DNA and their immune effects. Annu Rev Immunol 2002; 20: 709–760.
Majesky MW, Dong XR, Hoglund V, Mahoney WM, Daum G . The adventitia: a dynamic interface containing resident progenitor cells. Arterio Throm Vasc Biol 2011; 31: 1530–1539.
Torsney E, Xu Q . Resident vascular progenitor cells. J Mol Cell Cardiol 2011; 50: 304–311.
Mayr U, Zou Y, Zhang Z, Dietrich H, Hu Y, Xu Q . Accelerated arteriosclerosis of vein grafts in inducible NO synthase(−/−) mice is related to decreased endothelial progenitor cell repair. Circ Res 2006; 98: 412–420.
Jiang Z, Wu L, Miller BL, Goldman DR, Fernandez CM, Abouhamze ZS et al. A novel vein graft model: adaptation to differential flow environments. Am J Physiol Heart Circ Physiol 2004; 286: H240–H245.
Bradbury P, Gordon K . Connective tissues and stains. In: Bancroft JD, Stevens A (eds). Theory and Practice of Histological Techniques, Churchill Livingstone: London, 1992: 119–142.
Cunningham S, Meng QH, Klein N, McAnulty RJ, Hart SL . Evaluation of a porcine model for pulmonary gene transfer using a novel synthetic vector. J Gene Med 2002; 4: 438–446.
Acknowledgements
We thank Dr Scott Berceli and Dr Zhi-Hua Jiang for their help with the rabbit vein graft model; Ms Dyanne Rampling and Mr Steve Bottoms for EVG staining. This work was funded by the Wellcome Trust.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SH is an inventor on a patent for the peptide and lipid/peptide formulation used in this study. He also holds equity in, and is an advisor to a start-up company, Nanogenic Solutions Ltd., which aims to develop these technologies commercially. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Gene Therapy website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Meng, QH., Irvine, S., Tagalakis, A. et al. Inhibition of neointimal hyperplasia in a rabbit vein graft model following non-viral transfection with human iNOS cDNA. Gene Ther 20, 979–986 (2013). https://doi.org/10.1038/gt.2013.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2013.20