Abstract
Recent advances in human genomics led to the identification of numerous defective genes causing deafness, which represent novel putative therapeutic targets. Future gene-based treatment of deafness resulting from genetic or acquired sensorineural hearing loss may include strategies ranging from gene therapy to antisense delivery. For successful development of gene therapies, a minimal requirement involves the engineering of appropriate gene carrier systems. Transfer of exogenous genetic material into the mammalian inner ear using viral or non-viral vectors has been characterized over the last decade. The nature of inner ear cells targeted, as well as the transgene expression level and duration, are highly dependent on the vector type, the route of administration and the strength of the promoter driving expression. This review summarizes and discusses recent advances in inner ear gene-transfer technologies aimed at examining gene function or identifying new treatment for inner ear disorders.
Similar content being viewed by others
Introduction
Approximately 278 million people worldwide suffer from inner ear disorders.1 The lack of effective treatments for many forms of hearing loss or balance disorders is complicated by the diversity of disease processes leading to functional hearing loss. The mature mammalian inner ear comprises one auditory and five vestibular organs: the cochlea, the utricle, the saccule and three semicircular canals. The sensory epithelia of these organs consist of sensory cells, non-sensory supporting cells (SCs) and nerve endings. Hair cells (HCs) and SCs arise from a common progenitor after proliferation and differentiation within the sensory epithelia. There are two types of HCs in the organ of Corti (OC), the inner HCs being the true sensory cell type, responsible for the main mechanotransduction mechanism, and the outer HCs used to enhance the performance of the cochlea.2 Numerous disease processes, such as presbycusis, sudden neurosensory hearing loss, genetic diseases or Menière’s disease, cause inner ear dysfunction. The greatest majority of these disorders result directly or indirectly from degeneration and death of cochlear sensory cells and/or their associated peripheral neurons (that is, spiral or vestibular ganglion neurons). Currently, therapeutic strategies to treat inner ear diseases are limited to systemic delivery of medications, surgical intervention or sound amplification (with hearing aids) with limited success. Recent technological advancements in gene therapy and local drug delivery shade a new light for inner ear diseases. Therefore, there is a growing interest in successfully transferring genes in OC or vestibular cells (HCs, SCs and progenitors) and spiral or vestibular ganglion neurons. There are currently two main technical approaches for gene transfer: viral and non-viral vectors (Table 1). Gene transfer using viruses is named transduction, whereas gene transfer using non-viral vectors is referred as transfection. Both approaches may be appropriate for inner ear gene modulation, depending on the experimental needs, especially which cell type should be targeted.
Part of the challenge for developing gene therapy for the inner ear is physical. The inner ear is separated from the general circulation by a blood–cochlea barrier with similar properties to the blood–brain barrier, making systemic delivery less efficient.3 However, the inner ear is accessible via intratympanic delivery and diffusion through the round window membrane (RWM) or via a cochleostomy, through the stapes footplate, or through the endolymphatic sac4 (Figure 1). As described here, gene transfection or transduction via cochleostomy into the basal turn of the scala media was found to be more efficient than the RWM approach, mainly linked to the cell barrier and tight junctions present between the scala tympani and scala media (Tables 2, 3, 4, 5). The inner ear is a relatively closed space, making gene or drug delivery very efficient as compared with systemic delivery, for which large doses would be needed to reach the inner ear.5
Schematic illustration of the inner ear and of a cochlear turn cross-section. The scala vestibuli (SV) and scala tympani (ST) are filled with perilymph fluid, whereas the scala media (SM), containing the OC, is filled with endolymph. The OC comprises the non-sensory supporting cells as well as the sensory inner HCs (IHCs) and outer HCs (OHCs), contacted by spiral ganglion neuron fibres. Various routes of administration have been tested in the inner ear for gene delivery. Gene transfection or transduction in the inner ear could be performed via intratympanic delivery through the round window membrane (a), after cochleostomy and injection in the ST (b) or in the SM (c), or through the endolymphatic sac (d).
Viral vectors
Viral vectors are powerful tools for gene delivery in vitro and in vivo. For vector development, elements of the viral genome that contribute to replication, virulence and disease are deleted and replaced by genes of interest, but infectivity (cis-acting regulatory sequence) is retained. The deleted genes encoding proteins that are involved in replication or capsid/envelope proteins are included in a separate packaging construct to provide helper functions in trans. Non-replicating viral particles are generated by the introduction of the vector genome and packaging construct into a packaging cell line.6 One of the major advantages of viral vectors is their good efficiency of transfection and distinct tropism capacity, which can help restrict transgene expression to a subset of cells. The major drawbacks of these systems are their potential immunological and genetical toxicities, causing inflammation and insertional mutations, respectively. Six families of viruses have been engineered for inner ear transfection, both in vitro and in vivo: adenovirus, adeno-associated virus (AAV), lentivirus, herpes simplex virus, vaccinia virus and Sendai virus. They differ in complexity of construction, expression time, potential side effects and carrying capacity.
Adenovirus
Adenovirus is a non-enveloped, double-stranded DNA virus. The viral linear DNA genome coding region contains five early transcription regions (E1A, E1B, E2, E3 and E4), which have regulatory functions, and one late transcription region, encoding structural proteins.6 Adenoviruses exist as over 50 different serotypes, but only a few of them have been modified to generate vectors. Most emphasis has been placed on serotype 5 (Ad5).7 Adenoviral vectors infect a large variety of non-dividing cells. They grow easily in cell lines, allowing for production of high viral titres (>1011 viral particles per ml). To provide additional cloning space, the E1 and E3 early regions of the adenovirus are usually deleted to enable the insertion of an expression cassette of up to 7.5 Kb. Long-term and high expression levels of target genes are possible with this vector type; however, despite a good efficiency of transduction, its injection can provoke strong immune responses responsible for damage in recipient cells.8, 9, 10
The first generation of replication-deficient adenovirus vectors (deleted for E1A, E1B and a portion of E3 region) was based on the human Ad5 and has been widely used to transduce different cell types of inner ear explants in culture (Table 2). HCs, SCs and spiral ganglion neurons (SGNs) were successfully targeted by low titres of viral particles without any cell damage or defect in neurite extension.11, 12, 13, 14 However, transduction currents evoked by hair bundle displacement cannot be recorded after 36 h, despite a cell body appearing healthy.13
Cochlear cells have also been efficiently transduced in vivo by this first generation of adenoviral vectors. Ad5-RSV-LacZ (Ad5 expressing beta-galactosidase under the control of the Rous sarcoma virus—RSV—promoter) was injected through the round window into the scala tympani of the guinea pig cochlea. This led to a successful transduction of neural, epithelial and connective tissues of the cochlea.8, 15 Indeed, almost 50% of the cells in the spiral ganglion were efficiently infected, as well as the cells lining the perilymphatic space, including the cells of Reissner’s membrane and mesothelial cells (that is, fibroblasts that form a monolayer of specialized pavement-like cells that line the cavity of the scala tympani). However, this viral vector failed to transduce cells of the OC. In contrast, Ad5 vectors with the cytomegalovirus promoter driving green fluorescent protein (GFP) or LacZ expression have been shown to efficiently transduce pillar cells and, to a lesser extent, HCs when used at high titre (>108 Pfu per cochlea).10, 16 The use of alternative in vivo administration routes, through the endolymphatic sac or the scala media, enlarged the panel of transfected cells to stria vascularis cells and other types of SCs.17, 18, 19
To date, adenoviral vectors have proven their therapeutic potential in protecting inner ear cells from ototoxic damages. Delivery of glial cell-derived neurotrophic factor (GDNF) or transforming growth factor beta (TGFβ) genes to the mesothelial or Reissner’s membrane cells promoted survival of HCs and/or SGNs after aminoglycoside administration.20, 21, 22, 23, 24 However, the major limitation of this first generation of adenovirus vectors is that they usually trigger strong immune responses.13, 25 Ex vivo experiments with inoculation of fibroblasts, previously transduced with adenoviral vectors (Ad5-RSV-LacZ), into the perilymph, were performed to avoid an inflammatory response. Unfortunately, T-cell infiltration was not reduced using this approach.9 Therefore, new vector constructs were developed by retaining the E3 region, but deleting the E1 and E4 region.26 Various results were obtained using these new constructs (Table 2). Intact hair bundles of GFP-positive cells after exposure to high titres (107 particles per ml) of the defective vector were seen in vitro,27 whereas no difference in transfection efficiency and toxicity was observed in another study.12 In vivo experiments demonstrated that the second generation of adenoviruses were efficiently transduced in the OC after in utero injection. However, both early and advanced generation of adenoviruses induced toxicity when delivered to cells of the developing murine cochlea.28 E1/E3/E4 (Ad.11D)-deleted vectors were used to transduce Atoh1 gene, encoding a bHLH transcription factor involved in the generation of HCs in the mature guinea pig cochlea.29 Overexpression of Atoh1 resulted in the production of new HCs, both in physiological and pathological (destruction of HCs by aminoglycosides) conditions.29, 30 Ad5 vectors expressing catalase and Mn superoxide injected through the round window in the scala tympani, protects HCs against aminoglycoside-induced oxidative stress.31 The same Ad5 vector expressing neurotrophins transduced into the scala media in guinea pigs allowed short-term survival of SGNs after the degeneration of HCs, even if the vectors were not directly transduced into the neurons.32 Moreover, gain-of-function of Atoh1 with Ad28 vector in vestibular SCs (Ad28-GFAP-Atoh-1) was accompanied by de novo hair-cell generation and restoration of balance function following drug-induced hair-cell loss in mice.33
Adenoviruses bind cells primarily via the coxsackievirus and adenovirus receptor through the knob of the viral fibre. Adenovirus entry occurs through clathrin-mediated endocytosis after binding of the penton via its arginyl-glycyl-aspartic acid motif to αVβ3 and αVβ5 integrins.34 Therefore, the expression of coxsackievirus, adenovirus receptor and integrins on the host cells are a prerequisite to efficient transduction. Indeed, SGNs do not express the coxsackievirus and adenovirus receptor, and therefore, are not targeted by adenoviral vectors.35 Despite the presence of coxsackievirus and adenovirus receptor and integrins on other cochlear cells, poor transduction efficiency can be observed because of limited accessibility of those receptors. Different strategies to improve the binding of the vector to the cells have been developed. Incorporation of a small targeting ligand within the vector, such as an arginyl-glycyl-aspartic acid peptide specific to integrin receptor (Ad-arginyl-glycyl-aspartic acid) or seven lysine residues (Ad-F2K), greatly improves inner ear transduction.36 Searching for improving the yield of cochlear cell transfection with adenoviral vectors, Taura et al.37 recently discovered that histone deacetylase inhibition enhances adenoviral vector transduction in cochlear explants, and particularly in HCs and SCs.
Adeno-associated virus
AAVs are replication-deficient members of the parvovirus family with a 4.7 Kb single-stranded DNA genome. The viral genome flanked by two inverted terminal repeat sequences contains two open reading frames, rep and cap, and alternative splicing signals. The rep open reading frame encodes four proteins for replication, whereas the cap open reading frame encodes three structural proteins that form the capsid. A total of 12 human serotypes of AAV (AAV-1 to AAV-12) and more than 100 serotypes from non-human primates have been discovered to date. The use of the different AAV serotypes in a pseudotyping approach (creating hybrid AAV with the genome of one inverted terminal repeat sequence serotype being packaged into a different serotype capsid) has broadened tissue tropism.38, 39, 40 AAV is unique among viruses that are being developed for gene therapy in that the wild-type virus is not responsible for human disease. Therefore, AAV are able to transduce a wide range of cells and tissues, and are devoid of adverse consequences, such as immunogenicity, preventing cell clearance and thus allowing long-term gene expression. One major drawback of AAV is that the vector capacity is limited to 4–5 Kb, making it unsuitable for transfer of large genes.
Numerous publications have reported AAV transduction of the rodent inner ear through different routes of administration, targeting a range of cell types with variable efficiencies (Table 3). Different serotypes of AAV, with different cell tropisms, have been tested in the inner ear to specifically target HCs or neurons. Among them, AAV-2 showed the ability to transduce HCs and SCs in vitro,41 although it can only infect the spiral limbus, spiral ligament and spiral ganglion cells in vivo, following injection through the RWM.16, 42, 43 The same results were obtained using AAV-1,41 whereas AAV-5 could not transduce HCs either in vitro or in vivo.41, 44 However, AAV5 was efficient for transducing cells of the spiral ganglion, inner sulcus cells and Claudius cells.44, 45
In addition to these three serotypes, other AAV serotypes (AAV-3, -4, -7, -8) were tested in vivo by injection through the round window into the mouse cochlea. The AAV-3 vector was shown to be the most efficient in transducing cochlear HCs, whereas AAV-1, -2 and -7 could also transfect efficiently the SGNs.44 To further increase the AAV potential for inner ear gene delivery, pseudotyped vectors derived from AAV-2 serotype were constructed. The distribution of six serotypes (AAV2/1, -2/2, -2/5, -2/7, -2/8 and -2/9) following injection into the perilymph after cochleostomy was studied. All these AAV serotypes displayed tropism to HCs, with AAV2/2 being the most efficient.46, 47
In addition to AAV serotype, successful transduction in vivo is also dependent on the route of administration. In 1998, Lalwani et al.48 tried to transduce cochlear cells through a cochleostomy rather than through the round window. Sensory cells were not transduced by this approach, whereas spiral ganglion cells and spiral limbus cells were moderately transduced. Recently, AAV was directly injected into the scala media through a cochleostomy, providing direct access to the OC. Serotypes -1, -2, -5, -6 and -8 were successfully transduced into sensory and non-sensory cells of the OC.19, 49 However, this type of surgery does not guarantee hearing preservation.
AAV transduction efficiency into the inner ear also varies upon the promoter type driving the transgene expression. Most of the studies have used the human cytomegalovirus immediate-early promoter to carry out transgene expression. Nevertheless, the hybrid CAG promoter sequence from the chicken β-actin promoter and the cytomegalovirus immediate-early enhancer41, 50, 51 seems to be, to date, the most efficient promoter-mediating expression in HCs and neurons of the inner ear. More recently, delivery of AAV vectors to mouse embryonic otocysts in vivo allows the targeting of cochlear progenitors, and therefore HCs, SCs and SGNs.47
One drawback of using the AAV vectors is that the efficiency of gene transduction could be diminished in patients who possess AAV neutralizing antibodies. Indeed, AAV infection is common in childhood, leading to the acquisition of immunity against this virus. Thus, a new generation of AAV has been used: the bovine AAV, which has been shown to be serologically distinct from AAV serotypes 1 to 4.52
Bovine AAV efficiently transduced auditory and vestibular HCs and SCs53 in vitro. They also successfully transduced cells of the OC in vivo, both via trans-uterine microinjection to the embryonic E12.5 mouse otocyst,28 or after injection into the scala media or the scala tympani in adult guinea pig cochlea.54
One therapeutic perspective is to express large amounts of secretory proteins using AAV constructs. An AAV-1 vector containing the GDNF gene under the control of the CAG promoter has been injected into the rat RWM, and allowed protection of HCs and SGNs against aminoglycoside ototoxicity.55 AAV-2 carrying the brain-derived neurotrophin factor (BDNF) gene has been successfully transfected into the basilar membrane area (epithelial and mesothelial cells) following aminoglycoside treatment. This resulted in robust regrowth of nerve fibres towards the cells that secreted the neurotrophin.56 More recently, gene therapy has been successfully used in vitro. Indeed, the bovine AAV vectors delivering the Cx26 gene restored gap-junction coupling in cochlear non-sensory cells from the Cx26 conditional knock-out mice maintained in organotypic cultures.57
Lentivirus
Lentiviruses belong to a subclass of retroviruses. The one used for transduction are molecularly modified lentiviruses derived from HIV-1. The lentiviral vectors include a transgene construct in which the viral genes gag, pol and env have been replaced by promoter and transgene sequences and three helper (packaging) constructs expressing gag/pol, env and rev separately, to prevent homologous recombination. Typically, packaging cells (for example, the 293T human embryonic kidney cells) are co-transfected with a plasmid containing the vector genome and the packaging constructs to produce lentiviruses. Biosafety has been further increased by the development of self-inactivating vectors that contain deletions of the intrinsic promoter/enhancer activity of the HIV-1 long terminal repeat sequence, eliminating the transcription of the packaging signal that is required for vector mobilization.58 Given the restricted host range of the HIV-1 env glycoprotein, lentiviral vectors are pseudotyped with the vesicular stomatitis virus glycoproteins. The main advantages of lentiviruses is that they offer the possibility of inserting long DNA fragments, and they are able to transduce non-dividing cells. Therefore, lentiviruses were considered as suitable candidates for inner ear gene therapy (Table 4). Second-generation self-inactivating vectors under the control of the human elongation factor-1α promoter with a GFP reporter cassette have been transduced in the inner ear directly through the RWM. GFP transgene expression was restricted to the cells lining the perilymphatic space and lining cells of the scala tympani.59, 60, 61 Using trans-uterine microinjection, a low GFP expression level could be detected in outer HCs and SCs, but not in inner HCs.47 In vitro infection of cochlear explants from neonatal rats allowed a successful transduction of SGNs and some SCs, but not of any HCs.59 Another unique feature of lentiviruses is their capacity to integrate the host genome, thus allowing long-term transgene expression, but this advantage can turn out to be a serious limitation to the use of these vectors in gene therapy, as it would be genetically deleterious for the recipient cells.
Herpes simplex virus
The herpes simplex virus type 1 (HSV-1) is a human neurotropic virus with an overall diameter of 180–200 nm. It is a complex double-stranded DNA virus of about 150 Kb, encoding over 80 proteins.62 It is surrounded by an icosahedral capsid and an envelope. A similar strategy to the one used for producing adenoviral vectors has been applied to generate replication-defective HSV amplicon vectors. All or a combination of the five immediate-early genes (ICP0, ICP4, ICP22, ICP27 and ICP47), which are required for lytic infection and expression of all other viral proteins, were removed. The interest of HSV-1 as a gene transfer vector stems from its ability to infect many different cell types, both quiescent and proliferating cells. In addition, its extensive transgene capacity make it suitable for gene therapy. Amplicons are capable of harbouring an insert gene up to 100 Kb, and it never integrates into cellular chromosomes thus avoiding the risk of insertional mutagenesis.
HSV-1 amplicon vectors have been employed in vitro in the OC and the spiral ganglion explants (Table 4). Indeed, HCs and neurons were successfully infected and thus protected against specific ototoxic injuries with the use of HSV vectors harbouring brain-derived neurotrophin factor, NT-3 or bcl-2 cDNA.63, 64, 65 Similar amplicons were injected in vivo through the round window or via the lateral wall of the scala vestibuli. Although very few cells of the OC were transduced, SGNs were highly infected.66, 67, 68 In addition, inoculation of HSV vector driving NT-3 or brain-derived neurotrophin factor expression was able to protect neurons from a toxic insult66 or following hair-cell destruction.68
Other viral vectors
Vaccinia virus is a large, complex, enveloped virus belonging to the poxvirus family. Its genome consists of a linear, double-stranded DNA molecule of approximately 190 Kb. Vaccinia virus bearing the lacZ gene was tested for in vivo cochlear infection, following injection through the round window. Spiral ligament, Reissner’s membrane, lining cells of the scala vestibuli, and occasionally the inner and outer HCs of the apical region of the OC were transfected.69
Sendai virus, one of the members of Paramyxoviridae, is an enveloped virus with a negative-strand RNA genome of about 15 Kb. It causes severe respiratory disease in mice, but is non-pathogenic for humans.70 Sendai virus vector has been developed and has been shown to have high gene transduction efficiency and protein expression in different cell lineages.71 One of the characteristics of this vector is that its genome is located exclusively in the cytoplasm of infected cells and never goes through a DNA phase, thus precluding the integration of its genetic information into the cellular genome. Sendai virus vectors were injected into the guinea pig cochlea through the scala media or via the scala tympani, and were able to transfect a huge variety of cells, including the stria vascularis cells, SGNs and sensory cells of the OC.72
Non-viral delivery systems
Another strategy for gene delivery is based on the use of natural or synthetic compounds (also named non-viral vectors) in which complexes of DNA, proteins, polymers or lipids are formed in particles capable of efficiently transferring genes into cells. Methods of non-viral gene delivery can be subdivided into physical (carrier-free gene delivery) and chemical approaches (synthetic vector-based gene delivery). Despite their relatively lower efficiency, non-viral approaches are emerging as simpler, safer and more flexible alternatives to viral vectors. Methods of non-viral gene delivery to target the inner ear cells include chemical approaches using liposomes or polymers, and physical methods employing a physical force such as pressure or electric pulse. Noteworthy, these techniques are widely used as a tool of choice for research, allowing the functional characterization of numerous genes (Table 5), but less developed for gene therapy, as they are associated with a lack of specificity, a short-term transgene expression and cell toxicity.
Cationic liposomes
Liposomes are spherical vesicles composed of concentric phospholipid bilayers enclosing an aqueous compartment. The lipid-based reagents used for transfection (that is, lipofection) are generally composed of synthetic cationic lipids that are often mixed with helper lipids such as DOPE (L-a-dioleoyl phosphatidyl-ethanolamine) or cholesterol, which destabilizes the endosome following endocytosis, thus releasing DNA into the cytoplasm.73 These lipid mixtures assemble in the liposomes or micelles with an overall positive charge at physiological pH, and are able to form complexes (lipoplexes) with negatively charged nucleic acids through electrostatics interactions. A broad range of liposomal reagents is commercially available and includes Lipofectamine 2000, Lipofectin (Invitrogen, Gent, Belgium), Fugene (Promega Benelux, Leiden, The Netherlands), Hifect (Lonza, Verviers, Belgium) and Trifectin (IDT, Leuven, Belgium). Cationic liposomes are easily prepared in large amounts, making them inexpensive to make and protect the DNA from nuclease-mediated degradation. In addition, liposomes overcome problems of immunogenicity. However, they present limitations, such as the absence of relative tissue specificity and low transfection efficiency compared to viral vectors. Numerous studies using cationic liposomes have been performed both in vitro and in vivo to mediate transgene expression in the inner ear (Table 4). Neonatal organs of Corti have been successfully transfected in vitro using commercially available reagents (Lipofectamine 2000 or Lipofectin) with plasmids containing Math1(ref. 74) or with antisense oligonucleotides.75 However, the transfection yield was low (around 3%) as compared with viral delivery approaches. Different formulations of liposomes have also been tested in vivo, principally following local application on the RWM.42, 76, 77, 78 Analysis of cochlear sections from all liposomes-GFP or liposomes-β-galactosidase revealed transgene expression in various cell types, including SGNs, spiral limbus and spiral ligament cells. Transgene expression was persistent up to 14 days in certain cell populations, including SGNs.
Cationic non-liposomal polymers
Synthetic and naturally occurring cationic polymers, in linear or branched configuration, constitute another category of DNA carriers that have been widely used for gene delivery. These include, among others, polyethylenimine, polyamidoamine, polypropyleneimine dendrimers, cationic dextran, chitosan and poly (lactic-co-glycolic) acid.79 Although most cationic polymers condense DNA into small particles, forming polyplexes, and facilitate cellular uptake via endocytosis through charge–charge interaction with anionic cell surfaces, their transfection activity and toxicity differ dramatically.
In the cochlea, hyperbranched poly-L-lysine nanoparticles have been tested as delivery agents both in vivo and in vitro. These dendritic polymers with imperfectly branched or irregular structures, efficiently transfected spiral ganglion cells in cochlear organotypic cultures, although few HCs were targeted. Application of a gelatin sponge immersed in hyperbranched poly-L-lysine nanoparticles on the rat RWM in vivo favoured the targeting of HCs and SCs of the OC, cells of the stria vascularis, the spiral ligament and SGNs.80 Polyethylenimine-mediated cochlear gene transfer via cochleostomy and osmotic minipump was also tested.81 Mesothelial cells lining the scala vestibuli and scala tympani, mesenchymal and epithelial cells of the Reissner’s membrane and fibrocytes in the supra-striatal zone of the spiral ligament were successfully targeted. Unfortunately, no transfected cells were observed in the OC or in the stria vascularis. Poly (lactic-co-glycolic) acid nanoparticles encapsulating rhodamine and placed locally on the RWM in adult guinea pigs allow gene transfer in cells bordering the scala tympani after 24 h.82 All these polymer-based vehicles for DNA delivery lack selectivity toward cells and present significant cytotoxicity, therefore largely limiting their application in clinical practice.
Electroporation
This technique is based on the application of electric field pulses that create transient pores in lipidic membrane, allowing uptake of large charged molecules, such as plasmid DNA. The permeability of the membrane quickly reseals. Gene delivery efficiency is determined by the pulse intensity, duration and frequency.83 Electroporation works best on cells that are suspended in solution, but also works on solid tissue where electrodes can be applied.84 Indeed, in 2000, Zheng and Gao85 successfully transfected by electroporation postnatal rat cochlear explants with a pClig-GFP-Atoh1 vector in vitro. They showed that overexpression of Atoh-1 in the greater epithelial ridge and in the OC gave rise to new HCs. This technique has further been successfully used to transfect mouse explants at earlier developmental stages (starting at E13.5 in mice) and to silence specific gene expression by the use of short hairpin RNAs.86, 87
The choice of the vector promoter to drive gene expression is critical for the electroporation efficiency. Indeed, the use of the hybrid CAG promoter instead of cytomegalovirus alone results in a higher percentage of cells expressing the transgene to the sensory epithelia and the SGNs.88, 89 Recently, the need of an adequate promoter driving transgene expression was circumvented by cloning the transgene into a particular plasmid that allows synthesis of stabilized mRNA.90 Electroporation of this stable messenger greatly increases the number of cells expressing the transgene in the OC as compared with classical DNA plasmids.
Promising results were also obtained in the developing mouse inner ear in vivo. The DNA plasmid (pEF1-GFP) was microinjected through the uterine wall into the mouse E11.5 otic vesicle, and electric pulses transferred it into otic epithelial progenitor cells.91 Robust GFP expression was observed in HCs and SCs in the OC at E18.5. However, this technique, so far, has not been successfully used to transfect postnatal mice in vivo.
Biolistic
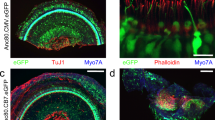
This method of gene delivery is also referred to as particle bombardment, micro-projectile gene transfer or gene gun. DNA is deposited on the coated surface of gold particles, which are then accelerated by high-voltage electronic discharge, spark discharge or helium pressure discharge onto cells or a tissue. Biolistic DNA injection also offers the capacity to deliver precise DNA dosages. Unfortunately, genes delivered by this method are expressed transiently, and there is considerable cell damage occurring at the centre of the discharge site. Early postnatal organs of Corti, were gene-gun transfected with pMYO15-EGFP-C2 previously coated with gold particles and were observed 24 h later. HCs were efficiently targeted, but the efficiency remains low (around three cells per explant).92, 93, 94
Conclusion
Tremendous efforts have been made over the last decade to improve gene transfer technologies in the inner ear. Despite the fact that some of these are not suitable for gene therapy because of poor transfection efficiencies, immunogenicity or cellular toxicity, they all represent a tool of choice for basic research on the auditory system. In the absence of adequate mouse models, overexpressing or silencing a specific gene expression in a spatio-temporal controlled manner can be accomplished using these technologies without affecting other tissues, thus allowing for precise functional characterization of key actors in inner ear development, cell survival and cell regeneration. Nevertheless, the recent advances in gene delivery opens the door to future prospects in inner ear gene therapy. Among the available viral vectors, AAV is one of the most promising gene therapy vectors for human clinical trials. Other viruses are less efficient in transducing sensory cells or SGNs. Regarding non-viral systems, although the chemical and physical approaches showed efficient targeting of HCs, SCs and SGNs, the amount of transfected cells and the in vivo selectivity are not sufficient for gene therapy.
Because of recent work to improve cochlear transfection and/or transduction, gene therapy in the inner ear appears to be more accessible than in the past. Continuing efforts in improving cochlear gene delivery, crossed with improving the knowledge of molecular events driving development, may lead to successful establishment of gene therapy to treat deafness.
References
Tucci DL, Schulz K, Witsell DL . Building a national research network for clinical investigations in otology and neurotology. Otol Neurotol Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 2010; 31: 190–195.
Raphael Y, Altschuler RA . Structure and innervation of the cochlea. Brain Res Bull 2003; 60: 397–422.
Harris JP . Immunology of the inner ear: evidence of local antibody production. Annal Otol Rhinol Laryngol 1984; 93: 157–162.
Staecker H, Brough DE, Praetorius M, Baker K . Drug delivery to the inner ear using gene therapy. Otolaryngol Clin North Am 2004; 37: 1091–1108.
Staecker H, Praetorius M, Brough DE . Development of gene therapy for inner ear disease: Using bilateral vestibular hypofunction as a vehicle for translational research. Hear Res 2011; 276: 44–51.
Kootstra NA, Verma IM . Gene therapy with viral vectors. Annu Rev Pharmacol Toxicol 2003; 43: 413–439.
Breyer B, Jiang W, Cheng H, Zhou L, Paul R, Feng T et al. Adenoviral vector-mediated gene transfer for human gene therapy. Curr Gene Ther 2001; 1: 149–162.
Raphael Y, Frisancho JC, Roessler BJ . Adenoviral-mediated gene transfer into guinea pig cochlear cells in vivo. Neurosci Lett 1996; 207: 137–141.
Weiss MA, Frisancho JC, Roessler BJ, Raphael Y . Viral-mediated gene transfer in the cochlea. Int J Dev Neurosci 1997; 15: 577–583.
Dazert S, Aletsee C, Brors D, Gravel C, Sendtner M, Ryan A . In vivo adenoviral transduction of the neonatal rat cochlea and middle ear. Hear Res 2001; 151: 30–40.
Dazert S, Battaglia A, Ryan AF . Transfection of neonatal rat cochlear cells in vitro with an adenovirus vector. Int J Dev Neurosci 1997; 15: 595–600.
Kanzaki S, Ogawa K, Camper SA, Raphael Y . Transgene expression in neonatal mouse inner ear explants mediated by first and advanced generation adenovirus vectors. Hear Res 2002; 169: 112–120.
Holt JR, Johns DC, Wang S, Chen ZY, Dunn RJ, Marban E et al. Functional expression of exogenous proteins in mammalian sensory hair cells infected with adenoviral vectors. J Neurophysiol 1999; 81: 1881–1888.
Ruan Q, Chen D, Wang Z, Chi F, He J, Wang J et al. Effects of Kir2.1 gene transfection in cochlear hair cells and application of neurotrophic factors on survival and neurite growth of co-cultured cochlear spiral ganglion neurons. Mol Cell Neurosci 2010; 43: 326–339.
Duan LM, Bordet T, Mezzina M, Kahn A, Ulfendahl M . Adenoviral and adeno-associated viral vector mediated gene transfer in the guinea pig cochlea. Neuroreport 2002; 13: 1295–1299.
Luebke AE, Foster PK, Muller CD, Peel AL . Cochlear function and transgene expression in the guinea pig cochlea, using adenovirus- and adeno-associated virus-directed gene transfer. Hum Gene Ther 2001; 12: 773–781.
Yamasoba T, Yagi M, Roessler BJ, Miller JM, Raphael Y . Inner ear transgene expression after adenoviral vector inoculation in the endolymphatic sac. Hum Gene Ther 1999; 10: 769–774.
Ishimoto S, Kawamoto K, Kanzaki S, Raphael Y . Gene transfer into supporting cells of the organ of Corti. Hear Res 2002; 173: 187–197.
Iizuka T, Kanzaki S, Mochizuki H, Inoshita A, Narui Y, Furukawa M et al. Noninvasive in vivo delivery of transgene via adeno-associated virus into supporting cells of the neonatal mouse cochlea. Hum Gene Ther 2008; 19: 384–390.
Yagi M, Magal E, Sheng Z, Ang KA, Raphael Y . Hair cell protection from aminoglycoside ototoxicity by adenovirus-mediated overexpression of glial cell line-derived neurotrophic factor. Hum Gene Ther 1999; 10: 813–823.
Suzuki M, Yagi M, Brown JN, Miller AL, Miller JM, Raphael Y . Effect of transgenic GDNF expression on gentamicin-induced cochlear and vestibular toxicity. Gene Therapy 2000; 7: 1046–1054.
Kawamoto K, Yagi M, Stover T, Kanzaki S, Raphael Y . Hearing and hair cells are protected by adenoviral gene therapy with TGF-beta1 and GDNF. Mol Ther 2003; 7: 484–492.
Yagi M, Kanzaki S, Kawamoto K, Shin B, Shah PP, Magal E et al. Spiral ganglion neurons are protected from degeneration by GDNF gene therapy. J Assoc Res Otolaryngol 2000; 1: 315–325.
Hakuba N, Watabe K, Hyodo J, Ohashi T, Eto Y, Taniguchi M et al. Adenovirus-mediated overexpression of a gene prevents hearing loss and progressive inner hair cell loss after transient cochlear ischemia in gerbils. Gene Therapy 2003; 10: 426–433.
Luebke AE, Steiger JD, Hodges BL, Amalfitano A . A modified adenovirus can transfect cochlear hair cells in vivo without compromising cochlear function. Gene Therapy 2001; 8: 789–794.
Brough DE, Lizonova A, Hsu C, Kulesa VA, Kovesdi I . A gene transfer vector-cell line system for complete functional complementation of adenovirus early regions E1 and E4. J Virol 1996; 70: 6497–6501.
Holt JR . Viral-mediated gene transfer to study the molecular physiology of the mammalian inner ear. Audiol Neurootol 2002; 7: 157–160.
Sheffield AM, Gubbels SP, Hildebrand MS, Newton SS, Chiorini JA, Di Pasquale G et al. Viral vector tropism for supporting cells in the developing murine cochlea. Hear Res 2011; 277: 28–36.
Kawamoto K, Ishimoto S, Minoda R, Brough DE, Raphael Y . Math1 gene transfer generates new cochlear hair cells in mature guinea pigs in vivo. J Neurosci 2003; 23: 4395–4400.
Izumikawa M, Minoda R, Kawamoto K, Abrashkin KA, Swiderski DL, Dolan DF et al. Auditory hair cell replacement and hearing improvement by Atoh1 gene therapy in deaf mammals. Nat Med 2005; 11: 271–276.
Kawamoto K, Sha SH, Minoda R, Izumikawa M, Kuriyama H, Schacht J et al. Antioxidant gene therapy can protect hearing and hair cells from ototoxicity. Mol Ther 2004; 9: 173–181.
Wise AK, Tu T, Atkinson PJ, Flynn BO, Sgro BE, Hume C et al. The effect of deafness duration on neurotrophin gene therapy for spiral ganglion neuron protection. Hear Res 2011; 278: 69–76.
Schlecker C, Praetorius M, Brough DE, Presler RG, Hsu C, Plinkert PK et al. Selective atonal gene delivery improves balance function in a mouse model of vestibular disease. Gene Therapy 2011; 18: 884–890.
Wickham TJ, Mathias P, Cheresh DA, Nemerow GR . Integrins alpha v beta 3 and alpha v beta 5 promote adenovirus internalization but not virus attachment. Cell 1993; 73: 309–319.
Venail F, Wang J, Ruel J, Ballana E, Rebillard G, Eybalin M et al. Coxsackie adenovirus receptor and alpha nu beta3/alpha nu beta5 integrins in adenovirus gene transfer of rat cochlea. Gene Therapy 2007; 14: 30–37.
Praetorius M, Brough DE, Hsu C, Plinkert PK, Pfannenstiel SC, Staecker H . Adenoviral vectors for improved gene delivery to the inner ear. Hear Res 2009; 248: 31–38.
Taura A, Taura K, Choung YH, Masuda M, Pak K, Chavez E et al. Histone deacetylase inhibition enhances adenoviral vector transduction in inner ear tissue. Neuroscience 2010; 166: 1185–1193.
Sugiyama A, Hattori S, Tanaka S, Isoda F, Kleopoulos S, Rosenfeld M et al. Defective adenoassociated viral-mediated transfection of insulin gene by direct injection into liver parenchyma decreases blood glucose of diabetic mice. Horm Metab Res 1997; 29: 599–603.
Champion HC, Georgakopoulos D, Haldar S, Wang L, Wang Y, Kass DA . Robust adenoviral and adeno-associated viral gene transfer to the in vivo murine heart: application to study of phospholamban physiology. Circulation 2003; 108: 2790–2797.
Peel AL, Klein RL . Adeno-associated virus vectors: activity and applications in the CNS. J Neurosci Methods 2000; 98: 95–104.
Stone IM, Lurie DI, Kelley MW, Poulsen DJ . Adeno-associated virus-mediated gene transfer to hair cells and support cells of the murine cochlea. Mol Ther 2005; 11: 843–848.
Jero J, Mhatre AN, Tseng CJ, Stern RE, Coling DE, Goldstein JA et al. Cochlear gene delivery through an intact round window membrane in mouse. Hum Gene Ther 2001; 12: 539–548.
Li Duan M, Bordet T, Mezzina M, Kahn A, Ulfendahl M . Adenoviral and adeno-associated viral vector mediated gene transfer in the guinea pig cochlea. Neuroreport 2002; 13: 1295–1299.
Liu Y, Okada T, Sheykholeslami K, Shimazaki K, Nomoto T, Muramatsu S et al. Specific and efficient transduction of Cochlear inner hair cells with recombinant adeno-associated virus type 3 vector. Mol Ther 2005; 12: 725–733.
Ballana E, Wang J, Venail F, Estivill X, Puel JL, Arbones ML et al. Efficient and specific transduction of cochlear supporting cells by adeno-associated virus serotype 5. Neurosci Lett 2008; 442: 134–139.
Konishi M, Kawamoto K, Izumikawa M, Kuriyama H, Yamashita T . Gene transfer into guinea pig cochlea using adeno-associated virus vectors. J Gene Med 2008; 10: 610–618.
Bedrosian JC, Gratton MA, Brigande JV, Tang W, Landau J, Bennett J . In vivo delivery of recombinant viruses to the fetal murine cochlea: transduction characteristics and long-term effects on auditory function. Mol Ther 2006; 14: 328–335.
Lalwani A, Walsh B, Reilly P, Carvalho G, Zolotukhin S, Muzyczka N et al. Long-term in vivo cochlear transgene expression mediated by recombinant adeno-associated virus. Gene Therapy 1998; 5: 277–281.
Kilpatrick LA, Li Q, Yang J, Goddard JC, Fekete DM, Lang H . Adeno-associated virus-mediated gene delivery into the scala media of the normal and deafened adult mouse ear. Gene Therapy 2011; 18: 569–578.
Alexopoulou AN, Couchman JR, Whiteford JR . The CMV early enhancer/chicken beta actin (CAG) promoter can be used to drive transgene expression during the differentiation of murine embryonic stem cells into vascular progenitors. BMC Cell Biol 2008; 9: 2.
Liu Y, Okada T, Nomoto T, Ke X, Kume A, Ozawa K et al. Promoter effects of adeno-associated viral vector for transgene expression in the cochlea in vivo. Exp Mol Med 2007; 39: 170–175.
Luchsinger E, Strobbe R, Wellemans G, Dekegel D, Sprecher-Goldberger S . [Haemagglutinating adeno-associated virus (AAV) in association with bovine adenovirus type 1. Brief report]. Arch Gesamte Virusforsch 1970; 31: 390–392.
Di Pasquale G, Rzadzinska A, Schneider ME, Bossis I, Chiorini JA, Kachar B . A novel bovine virus efficiently transduces inner ear neuroepithelial cells. Mol Ther 2005; 11: 849–855.
Shibata SB, Di Pasquale G, Cortez SR, Chiorini JA, Raphael Y . Gene transfer using bovine adeno-associated virus in the guinea pig cochlea. Gene Therapy 2009; 16: 990–997.
Liu Y, Okada T, Shimazaki K, Sheykholeslami K, Nomoto T, Muramatsu S et al. Protection against aminoglycoside-induced ototoxicity by regulated AAV vector-mediated GDNF gene transfer into the cochlea. Mol Ther 2008; 16: 474–480.
Shibata SB, Cortez SR, Beyer LA, Wiler JA, Di Polo A, Pfingst BE et al. Transgenic BDNF induces nerve fiber regrowth into the auditory epithelium in deaf cochleae. Exp Neurol 2010; 223: 464–472.
Crispino G, Di Pasquale G, Scimemi P, Rodriguez L, Galindo Ramirez F, De Siati RD et al. BAAV mediated GJB2 gene transfer restores gap junction coupling in cochlear organotypic cultures from deaf Cx26Sox10Cre mice. PLoS One 2011; 6: e23279.
Zufferey R, Dull T, Mandel RJ, Bukovsky A, Quiroz D, Naldini L et al. Self-inactivating lentivirus vector for safe and efficient in vivo gene delivery. J Virol 1998; 72: 9873–9880.
Han JJ, Mhatre AN, Wareing M, Pettis R, Gao WQ, Zufferey RN et al. Transgene expression in the guinea pig cochlea mediated by a lentivirus-derived gene transfer vector. Hum Gene Ther 1999; 10: 1867–1873.
Pietola L, Aarnisalo AA, Joensuu J, Pellinen R, Wahlfors J, Jero J . HOX-GFP and WOX-GFP lentivirus vectors for inner ear gene transfer. Acta Otolaryngol 2008; 128: 613–620.
Lei L, Han D . Efficient transduction of spiral ganglion cells using adenovirus type 5 vector in the rat. Acta Otolaryngol 2010; 130: 810–814.
Epstein AL . Progress and prospects: biological properties and technological advances of herpes simplex virus type 1-based amplicon vectors. Gene Therapy 2009; 16: 709–715.
Chen X, Frisina RD, Bowers WJ, Frisina DR, Federoff HJ . HSV amplicon-mediated neurotrophin-3 expression protects murine spiral ganglion neurons from cisplatin-induced damage. Mol Ther 2001; 3: 958–963.
Staecker H, Liu W, Malgrange B, Lefebvre PP, Van De Water TR . Vector-mediated delivery of bcl-2 prevents degeneration of auditory hair cells and neurons after injury. ORL J Otorhinolaryngol Relat Spec 2007; 69: 43–50.
Geschwind MD, Hartnick CJ, Liu W, Amat J, Van De Water TR, Federoff HJ . Defective HSV-1 vector expressing BDNF in auditory ganglia elicits neurite outgrowth: model for treatment of neuron loss following cochlear degeneration. Hum Gene Ther 1996; 7: 173–182.
Bowers WJ, Chen X, Guo H, Frisina DR, Federoff HJ, Frisina RD . Neurotrophin-3 transduction attenuates cisplatin spiral ganglion neuron ototoxicity in the cochlea. Mol Ther 2002; 6: 12–18.
Staecker H, Li D, O’Malley BW, Van De Water TR . Gene expression in the mammalian cochlea: a study of multiple vector systems. Acta Otolaryngol 2001; 121: 157–163.
Staecker H, Gabaizadeh R, Federoff H, Van De Water TR . Brain-derived neurotrophic factor gene therapy prevents spiral ganglion degeneration after hair cell loss. Otolaryngol Head Neck Surg 1998; 119: 7–13.
Derby ML, Sena-Esteves M, Breakefield XO, Corey DP . Gene transfer into the mammalian inner ear using HSV-1 and vaccinia virus vectors. Hear Res 1999; 134: 1–8.
Bitzer M, Armeanu S, Lauer UM, Neubert WJ . Sendai virus vectors as an emerging negative-strand RNA viral vector system. J Gene Med 2003; 5: 543–553.
Hosoya N, Miura T, Kawana-Tachikawa A, Koibuchi T, Shioda T, Odawara T et al. Comparison between Sendai virus and adenovirus vectors to transduce HIV-1 genes into human dendritic cells. J Med Virol 2008; 80: 373–382.
Kanzaki S, Shiotani A, Inoue M, Hasegawa M, Ogawa K . Sendai virus vector-mediated transgene expression in the cochlea in vivo. Audiol Neurootol 2007; 12: 119–126.
Wrobel I, Collins D . Fusion of cationic liposomes with mammalian cells occurs after endocytosis. Biochim Biophys Acta 1995; 1235: 296–304.
Zhang W, Zhang Y, Sood R, Ranjan S, Surovtseva E, Ahmad A et al. Visualization of intracellular trafficking of Math1 protein in different cell types with a newly-constructed nonviral gene delivery plasmid. J Gene Med 2011; 13: 134–144.
Zine A, Van De Water TR, de Ribaupierre F . Notch signaling regulates the pattern of auditory hair cell differentiation in mammals. Development 2000; 127: 3373–3383.
Wareing M, Mhatre AN, Pettis R, Han JJ, Haut T, Pfister MH et al. Cationic liposome mediated transgene expression in the guinea pig cochlea. Hear Res 1999; 128: 61–69.
Jero J, Tseng CJ, Mhatre AN, Lalwani AK . A surgical approach appropriate for targeted cochlear gene therapy in the mouse. Hear Res 2001; 151: 106–114.
Zou J, Saulnier P, Perrier T, Zhang Y, Manninen T, Toppila E et al. Distribution of lipid nanocapsules in different cochlear cell populations after round window membrane permeation. J Biomed Mater Res B Appl Biomater 2008; 87: 10–18.
Gao X, Kim KS, Liu D . Nonviral gene delivery: what we know and what is next. Aaps J 2007; 9: E92–104.
Zhang W, Zhang Y, Lobler M, Schmitz KP, Ahmad A, Pyykko I et al. Nuclear entry of hyperbranched polylysine nanoparticles into cochlear cells. Int J Nanomed 2011; 6: 535–546.
Tan BT, Foong KH, Lee MM, Ruan R . Polyethylenimine-mediated cochlear gene transfer in guinea pigs. Arch Otolaryngol Head Neck Surg 2008; 134: 884–891.
Tamura T, Kita T, Nakagawa T, Endo T, Kim TS, Ishihara T et al. Drug delivery to the cochlea using PLGA nanoparticles. Laryngoscope 2005; 115: 2000–2005.
Heller LC, Ugen K, Heller R . Electroporation for targeted gene transfer. Expert Opin Drug Deliv 2005; 2: 255–268.
Favard C, Dean DS, Rols MP . Electrotransfer as a non viral method of gene delivery. Curr Gene Ther 2007; 7: 67–77.
Zheng JL, Gao WQ . Overexpression of Math1 induces robust production of extra hair cells in postnatal rat inner ears. Nat Neurosci 2000; 3: 580–586.
Ono K, Nakagawa T, Kojima K, Matsumoto M, Kawauchi T, Hoshino M et al. Silencing p27 reverses post-mitotic state of supporting cells in neonatal mouse cochleae. Mol Cell Neurosci 2009; 42: 391–398.
Jones JM, Montcouquiol M, Dabdoub A, Woods C, Kelley MW . Inhibitors of differentiation and DNA binding (Ids) regulate Math1 and hair cell formation during the development of the organ of Corti. J Neurosci 2006; 26: 550–558.
Driver EC, Kelley MW . Transfection of mouse cochlear explants by electroporation. Current Protocols in Neuroscience 2010; Chapter 4, Unit 4.34 1–10.
Puligilla C, Dabdoub A, Brenowitz SD, Kelley MW . Sox2 induces neuronal formation in the developing mammalian cochlea. J Neurosci 2010; 30: 714–722.
Hayashi T, Lamba DA, Slowik A, Reh TA, Bermingham-McDonogh O . A method for stabilizing RNA for transfection that allows control of expression duration. Dev Dyn 2010; 239: 2034–2040.
Gubbels SP, Woessner DW, Mitchell JC, Ricci AJ, Brigande JV . Functional auditory hair cells produced in the mammalian cochlea by in utero gene transfer. Nature 2008; 455: 537–541.
Belyantseva IA . Helios Gene Gun-mediated transfection of the inner ear sensory epithelium. Methods Mol Biol 2009; 493: 103–123.
Belyantseva IA, Boger ET, Friedman TB . Myosin XVa localizes to the tips of inner ear sensory cell stereocilia and is essential for staircase formation of the hair bundle. Proc Natl Acad Sci USA 2003; 100: 13958–13963.
Belyantseva IA, Boger ET, Naz S, Frolenkov GI, Sellers JR, Ahmed ZM et al. Myosin-XVa is required for tip localization of whirlin and differential elongation of hair-cell stereocilia. Nat Cell Biol 2005; 7: 148–156.
Toyama K, Ozeki M, Hamajima Y, Lin J . Expression of the integrin genes in the developing cochlea of rats. Hear Res 2005; 201: 21–26.
Woods C, Montcouquiol M, Kelley MW . Math1 regulates development of the sensory epithelium in the mammalian cochlea. Nat Neurosci 2004; 7: 1310–1318.
Brigande JV, Gubbels SP, Woessner DW, Jungwirth JJ, Bresee CS . Electroporation-mediated gene transfer to the developing mouse inner ear. Methods Mol Biol 2009; 493: 125–139.
Acknowledgements
We thank Bernard Minguet for his assistance with Figure 1. This work was supported by the Belgian Fonds National de la Recherche Scientifique (FNRS) and the Fonds Leon Fredericq (FLF, Faculty of Medicine, University of Liege). LN is funded by the Walloon Excellence in Lifesciences and Biotechnology (WELBIO). LB, LN and BM are postdoctoral researcher, research associate and research director, respectively, from FNRS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sacheli, R., Delacroix, L., Vandenackerveken, P. et al. Gene transfer in inner ear cells: a challenging race. Gene Ther 20, 237–247 (2013). https://doi.org/10.1038/gt.2012.51
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2012.51
Keywords
This article is cited by
-
Effect of ursodiol on alginate/PLL nanoparticles with non-ionic surfactant for gene delivery
Journal of Nanoparticle Research (2024)
-
Gene Therapy for Congenital Hearing Loss
Current Otorhinolaryngology Reports (2022)
-
Stem Cells and Gene Therapy in Progressive Hearing Loss: the State of the Art
Journal of the Association for Research in Otolaryngology (2021)
-
Recent development of AAV-based gene therapies for inner ear disorders
Gene Therapy (2020)
-
Treatment of autosomal dominant hearing loss by in vivo delivery of genome editing agents
Nature (2018)