Abstract
Purpose
Population BRCA1/BRCA2 screening identifies carriers irrespective of family history, yet this information is actionable for relatives. We examined familial communication rates and cascade testing in the screening setting and assessed sociodemographic and psychosocial predictors.
Methods
Participants in a BRCA1/BRCA2 screening study of healthy Ashkenazi Jews self-administered a family communication questionnaire. Intent to communicate was determined before genetic status was known, along with result communication (carriers and noncarriers) 6 months and 2 years after enrollment. Carriers underwent in-depth interviews and provided cascade testing information.
Results
In total, 88% (524/595) of questionnaire responders and 97% (30/32) of carriers informed at least one relative. In multivariate analysis, family history (P = 0.005) and greater Satisfaction With Health Decision scores (P < 0.001) predicted communication of results. Among carriers’ adult first- and second-degree relatives, 71 (48%) had cascade testing, more commonly performed in first- (58%) than in second-degree relatives (26%, P = 0.0002), and in females (56%) vs. males (36%, P = 0.02). At least 11% remained uninformed.
Conclusion
Familial communication rates and characteristics in a screening setting parallel those reported by Cancer Genetics clinics. Universal screening circumvents dependence on familial disclosure. However, our finding that satisfaction—a potentially modifiable factor—predicts communication, raises the hypothesis that improving the testing experience could facilitate familial communication.
Similar content being viewed by others
Introduction
Identifying a BRCA mutation has actionable familial implications. Noncarrier relatives can avoid unnecessary interventions, whereas carrier relatives can utilize surveillance and prevention measures, reducing morbidity and mortality.1,2 In the context of population screening, which aims to maximize identification of BRCA carriers, familial communication can increase the secondary yield of screening. Yield can be increased through cascade testing in carriers, and also by further familial testing in noncarriers with significant family history.
Early BRCA familial communication studies focused on communication rates and testing uptake in families harboring mutations. While 91–100% of participants reported communication with at least one relative,3,4,5,6 actual testing rates in relatives were much lower, ranging from 30 to 60%.4,5,7,8,9,10,11 This substantial gap led to studies that examined predictors of BRCA communication to determine potential strategies for promoting familial testing.12,13,14 Increased knowledge and satisfaction with the decision to have BRCA testing,12 as well as lower genetic worry,14 were found to be associated with increased familial communication.
Previous familial communication studies were based on carriers identified through clinical testing, mostly for personal history of cancer, where probands underwent conventional in-person pre- and post-test genetic counseling. We performed a population screening trial of BRCA mutations in Ashkenazi Jews,15 where testing was offered to participants without a personal cancer history. In-person genetic counseling was performed only after testing, and only for carriers and for noncarriers with suggestive family history. Of the carriers identified, 40% lacked relevant family history. The goal of this study was to explore familial communication among participants in a screening trial. Specifically, we aimed to determine the rates of communication and cascade testing, and to identify factors that affect them. Rates of intent to communicate and actual communication were assessed before and after test results were received, respectively. We examined sociodemographic and psychosocial variables as predictors of familial communication in both carriers and noncarriers. In carriers, in addition to evaluating rates and characteristics of cascade testing, themes relevant to familial communication were explored using in-depth interviews.
Materials and methods
This study was approved by the Shaare Zedek Medical Center institutional review board and participants gave written informed consent.
Participants
The BRCA1/BRCA2 population screening trial in Ashkenazi Jews has previously been reported.15 Inclusion criteria were that participants were of Ashkenazi Jewish origin, aged ≥25 years, lacked a personal cancer history, had not previously undergone BRCA testing, and had no known BRCA mutation in the family. Participants were not selected based on family history of cancer. A total of 1,771 participants were enrolled. Their mean age was 52 years (SD = 13), and 79% (1,406/1,771) were female. Participants were either recruited (n = 1,027, 58%) through mammography centers, ambulatory clinics, and executive screening clinics or self-referred in response to brochures and posters in medical settings (n = 744, 42%).
Testing and counseling
Before testing, participants received written information without in-person genetic counseling. Results were provided by in-person genetic counseling to all carriers and to noncarriers with a significant family history.
Participants were tested for the common Ashkenazi Jew mutations (BRCA1-185delAG, 5382insC and BRCA2-6174delT), and 32 (1.8%) mutation carriers were identified.
Study questionnaires
Sociodemographic information and family history of cancer were provided at the time of enrollment.15 Family communication was examined using questionnaires. Carriers also underwent in-depth interviews.
For psychosocial assessment, self-administered, Web-based questionnaires were sent 1 week after enrollment, before receiving the results (Q1), 6 months after enrollment, after receiving the results (Q2), and 2 years after enrollment (Q3). Q1 and Q2 have been described previously,15 and included six psychosocial measures: general satisfaction with participation and testing; the Satisfaction with Health Decision (SWHD) scale; the State Trait Anxiety Inventory scale-6 (STAI-6); the Impact of Events Scale (a measure of stress); the Perceived Personal Control scale; and knowledge items (score range: 0–10). Psychosocial scales were anchored to BRCA testing. Q3 questionnaires were shorter and included three psychosocial measures: general satisfaction with participation and testing; the Impact of Events Scale; and knowledge items.
Questions regarding familial BRCA communication were included in all three questionnaires (Table 1). Participants indicating communication to relatives were asked to identify which relatives they informed.
Carrier interviews
Interviews were semistructured, as previously reported.16 The structured component included questions regarding familial communication. Transcripts were qualitatively analyzed using Atlas.ti for recurring themes within interviews and across groups of respondents.17,18
Cascade testing
Post-test genetic counseling in carriers included recommendations to refer relatives. Genetic counseling and testing were available to relatives free of charge, both through the study and through Israel’s national health system. For relatives tested outside the study, information was completed by interviewing carriers. Cascade testing was analyzed in living first- and second-degree relatives on the relevant side of the family (if known) in females aged ≥25 years and males ≥35 years who were not tested before the carrier was identified through the study.
Statistical analysis
Continuous and categorical variables were respectively analyzed using t-tests and Chi-squared tests for univariate comparisons, and multiple linear and logistic regressions for multivariate analysis. Paired data were compared using paired t-tests and McNemar’s test. All reported P values are two-tailed and the results were considered significant for P < 0.05. Confidence intervals (CIs) were calculated at the 95% level.
Sample size calculations were not performed for this secondary analysis as the study was powered based on the primary aims of the screening trial.15
Results
Response to questionnaires
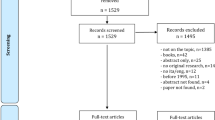
Of 1,771 participants in the BRCA screening study, 1,255 received Q1 and Q2 questionnaires. Due to technical difficulties, questionnaires were not sent to 516 participants. Q3 questionnaires were sent to all study participants. Response rates were 845 of 1,255 (67%) for Q1, 623 of 1,255 (50%) for Q2, and 759 of 1,771 (43%) for Q3. The characteristics of the questionnaire responders and nonresponders are shown in Table 2. At all time points, responders were more likely to be female (odds ratio (OR) = 1.5–1.7, P = 0.001) and to have been self-referred (OR = 1.6, P < 0.001). A family history of hereditary breast and ovarian cancer (HBOC) was more prevalent in responders to Q1 (OR = 1.3, P = 0.035), but similar to nonresponders in Q2 and Q3. Q1 response rates were lower among ultraorthodox participants (OR = 0.4, P < 0.001).
Response in carriers
Of the 32 carriers, 30 provided communication information. Carrier status was known only after Q1. The carrier response was 18 of 32 for Q2 and 27 of 32 for Q3. In-depth interviews were conducted for 26 (81%) carriers,16 and 3 additional carriers were interviewed by phone specifically regarding familial communication.
Familial communication
All participants
Intent to communicate BRCA testing (Q1, testing communication)
Of 1,225 participants, 800 (65%) answered Q1 familial communication questions. Of these, 682 responders (85%) intended to inform relatives of being tested. Self-referral (OR = 2.1, P = 0.003) and HBOC family history (OR = 2.5, P = 0.002) were associated with increased intent to inform (Table 3). Intent to inform was higher in women (OR = 1.7, P = 0.049) and married participants (OR = 1.8, P = 0.04), and lower among the ultraorthodox (OR = 0.2, P = 0.003). Of the psychosocial measures, SWHD significantly predicted intent, and knowledge was a borderline predictor. For each one-point increase in the SWHD (range: 6–30) or knowledge score (range: 0–10), intent to inform relatives was greater by 1.1-fold (P = 0.002 and 0.054, respectively) (Table 3).
Intent to communicate BRCA carrier status (Q1, carrier communication)
In Q1, 774 of 800 responders (97%) said that if they were found to be carriers they would inform their relatives. In multivariate analysis, the entire model was not significant since intention to communicate carrier status was essentially uniform (97%). Notably, intent to inform relatives about carrier status was significantly higher than intent to inform them about being tested (97 versus 85%, P < 0.001).
Actual communication of test results (Q2)
After receiving their test results, 595 of 1,255 participants (47%) responded to Q2 familial communication questions. Of these, 524 (88%) reported communication of the test results to at least one relative. In multivariate analysis, HBOC family history and enrollment method were significant predictors of communication (OR = 3.3, P = 0.005 for moderate-to-high HBOC likelihood versus little or no family history; and OR = 1.9, P = 0.035 for self-referral versus recruiter enrollment; Table 3). Gender, age, education, marital status, having children, and religiosity did not predict communication. Neither did carrier status, but this analysis was limited by the small number of carriers. SWHD score was the only significant psychosocial predictor (OR = 1.2 per point, P < 0.001). The likelihood of communicating was sixfold higher in those whose SWHD scores were in the highest versus the lowest quartile. Scores in the other psychosocial scales (Perceived Personal Control, the Impact of Events Scale, STAI-6, and knowledge) were not significant predictors (Table 3).
Familial communication: intent versus performance and effect of relationship degree
The rate of intention to communicate about being tested (85%) was similar to communication of the results to at least one relative (88%). However, actual communication rates to specific types of relatives were significantly lower. Among responders to Q1 who indicated intent to communicate and also responded to Q2, gaps between intention and performance were observed for relatives of all degrees and both sexes (Table 4). Declines were greater for male versus female relatives at all degrees of relatedness (e.g., 54% (95% CI: 49–62%) and 61% (95% CI: 56–70%) declines for sons and brothers, respectively, versus 37% (95% CI: 34–43%) and 36% (95% CI: 33–43%) declines for daughters and sisters, respectively). Declines between intent and performance were also greater for more distant versus first-degree relatives (e.g., 67% (95% CI: 60–81%) for aunts versus 36% (95% CI: 33–43%) for sisters). Similar effects of sex and degree of relationship on intent and performance of familial communication were observed in all responders (Supplementary Table S1 online). See Supplementary Information for differences between intended versus actual utilization of consultation with others regarding familial communication.
Long-term communication (Q3)
Two years after testing, 301 of 721 responders to Q3 (42%), including 13 carriers, reported that they had informed a relative regarding their test results within the past 6 months. In multivariate analysis, having children (OR = 2.2, P = 0.01) and a family history of HBOC (OR = 1.5, P = 0.03 for a high-to-moderate likelihood of HBOC) significantly predicted this “late” communication (Table 3). Better knowledge was a borderline predictor (Table 3).
Carriers
Familial communication and cascade testing in carriers
All participating carriers except one (29/30; 97%) reported informing at least one relative. Complete information on communication and cascade testing was available for families of 27 of 30 carriers (90%) with first-degree relatives (2 carriers had no relevant first-degree relatives). All female relatives were tested in 9 of 27 families (33%) and all first-degree female relatives were tested in 17 of 27 families (59%). However, in 4 of 27 cases (15%), no first-degree female relatives were tested.
Overall, 71 of 148 eligible first- and second-degree relatives of the 32 carriers (48%) were tested (Table 5). Testing rates were higher in first- versus second-degree relatives (59/101 (58%) versus 12/47 (26%), respectively; P = 0.0002) and among female versus male relatives (P = 0.02). Among first-degree relatives, 40 of 60 women (67%) and 19 of 41 men (46%) were tested, among whom 22 of 40 women (55%) and 9 of 19 men (47%) were identified as carriers. Among second-degree relatives, 9 of 27 females (33%) were tested, and they were significantly older than untested second-degree relatives (54.4 versus 37.2 years, respectively; P = 0.01). Of the first- and second-degree relatives tested, 19 of 148 (13%) had a previous cancer diagnosis, including 13 diagnosed with BRCA-associated malignancies (breast, ovarian, prostate, and melanoma). Of these, 12 of 19 (63%) were tested and 10 of 12 (83%) were carriers. The 2 phenocopies had breast cancer (age: 75) and melanoma (age: 59).
In univariate analysis, female first-degree relatives of carriers without children were more likely to be tested than those of carriers with children (100 versus 64%; P = 0.001). Self-referral (versus recruiter enrollment) was associated with higher rates of cascade testing only in male first-degree relatives (60 versus 11%; P = 0.002). HBOC family history did not affect testing rates. However, in multivariate analysis, the entire model was not significant.
Of 148 first- and second-degree degree relatives, 77 (52%) were not tested (Table 5). Of those not tested, 26 (34%) were aware of the familial mutation, 16 (21%) were not informed of the familial mutation, and we are uncertain whether the remaining 35 (45%) were informed. Thus, of 148 eligible first- and second-degree relatives, between 11% (16/148) and 34% (51/148) remained uninformed.
Carriers’ attitudes toward familial communication: a qualitative analysis
In-depth interviews were conducted with 26 of 32 carriers (81%), as previously reported.17 Here, we focus on familial communication. Carriers expressed three main motives for familial communication. The first was a general sense of responsibility and familial commitment: “I felt a duty to inform … that it was a very serious responsibility not to tell them because they must get tested.” (37-year-old female carrier with low-likelihood family history)
The second was the fear that a relative would be diagnosed with preventable cancer: “I want to do it right … to do what’s necessary for my daughters … [Heaven] forbid if I could have prevented something from happening and didn’t say anything…” (54-year-old female carrier with no family history)
The third was tapping into familial communication as a source of strength: “My husband … gave me strength when I told him I wished the mutation would be taken from me. He said, have the preventive oophorectomy … and it will go away … It’s one way of looking at it. Of course it helps to have such familial support.” (32-year-old female carrier with high-likelihood family history)
Despite these important motivators, 11–34% of carriers’ first- and second-degree relatives were uninformed of the familial mutation. The main communication barrier was the reluctance to cause fear, stress, and negative emotions: “I’m sad that because of me, everyone has to get into this. It’s difficult and scary.” (37-year-old female carrier with low-likelihood family history)
In some cases, carriers felt that the costs outweighed the benefits: “My parents still don’t know. I tried to tell them, but they are very old and I saw that it was very difficult for my Mom. So, ultimately, I didn’t tell.” (47-year-old female carrier with no family history)
Fear of discrimination was mentioned by only two carriers, both in the context of marriage. One 60-year-old carrier informed her two married daughters, but no one else, out of concern for her unmarried son. A 30-year-old unmarried carrier was asked by her parents not to inform relatives until she marries.
Additional barriers were the degree of personal connection and readiness for discussion. Six carriers expressed difficulty initiating contact with distant, rarely seen relatives (cousins and adult aunts or uncles), particularly relatives living abroad. Some carriers used other relatives (mostly their mothers) as surrogates. Some carriers perceived male relatives, especially brothers, as more vulnerable and less capable of handling carrier information, and resolved the communication dilemma by informing these men’s wives, even though they were not genetically related.
One carrier inferred lack of interest. She discussed BRCA testing with her uncle and his wife because the wife (unrelated to the proband) was recently diagnosed with breast cancer: “I told myself now is the time to bring it up … but she (the uncle’s wife) said that my uncle told her not to have the BRCA test. My uncle said: “What’s the use? How is it helpful?” … So I stopped myself. I felt that I couldn’t tell him.” (37-year-old female carrier with moderate-likelihood family history)
A few carriers described rejection of information they communicated. One 36-year-old carrier informed her 33-year-old sister who was affected with breast cancer, and was met with refusal to receive genetic information16.
Three of the interviewed carriers described complicated situations where first-degree relatives they informed about the mutation did not want to deliver the information to their children. Interestingly, all three felt they had fulfilled their duty, and that informing children is the parent’s responsibility, even when the uninformed individuals were the proband’s grandchildren or nieces. For example, a carrier’s brother and his wife said they would not tell their daughter: “I told my sister-in-law, “I’m telling you because it’s my responsibility and moral [duty] … Do whatever you want with this [information]. She’s your daughter.” The next day, she texted me to say she’s sorry if she responded too aggressively, but that this is what they believe [it is right to do]. I told her … “I respect your choice. Do whatever you want.”” (47-year-old female carrier with no family history)
Familial communication over time
Carriers differed in the timing of communication. Some informed relatives immediately, even in the car on their way home from the post-test counseling appointment. Some described waiting for a convenient meeting or timing. At the other end of the spectrum, some carriers waited for longer periods—even a year or more. Some had external reasons for delaying; e.g., waiting for daughters to get pregnant or give birth. Others needed the time to complete an internal, personal process before they were ready to communicate. One carrier explained that her first reaction was not to share the information since it was difficult and uncharacteristic for her to expose herself: “But then time passes and you understand the meaning and the responsibility. This niece who might be pregnant now, or that cousin who is a single mother … I couldn’t afford [to keep it] to myself. It would be really irresponsible. I understood that I have no choice, and I started on my way.” (42-year-old female carrier with moderate-likelihood family history)
Discussion
This study reports familial communication in a BRCA1/BRCA2 screening setting. Universal screening seemingly preempts the need for familial communication, since testing is offered to all, regardless of family history or a familial mutation. However, familial communication remains important even in this setting: relatives can be alerted of their high risk of being carriers, and the screening program yield can be increased by cascade testing and through identification of high-risk families.19,20,21
Previous studies of familial communication were performed in Cancer Genetics clinics on people tested because of a personal or family history of cancer. We found an 85% rate of intent to communicate about testing to any relative and an 88% rate of actual communication of the test results to at least one relative 3–4 months after receiving them. In comparison, reported rates of any test communication in Cancer Genetics clinics are >90%.4,5,6,7 We hypothesized that this difference could be explained by the lack of a family history in most screening participants. Indeed, HBOC family history predicted greater communication at all time points, especially shortly after receipt of the test results (OR = 3.3, P = 0.005).
Communication of carrier status was significantly higher than testing communication: in Q1, 97% indicated that they would inform relatives if they were found to be carriers. Among the participating carriers, all but one (29/30; 97%) disclosed their carrier status to at least one relative. The carrier communication rates were similar to those previously reported,4,5,7,8,9,10,11 suggesting that while testing communication is perhaps lower in the screening setting, carrier communication is as high as in the clinical setting. Qualitative interviews revealed that communication of carrier status was driven by a sense of responsibility, familial commitment, and the fear of not preventing a cancer diagnosis in relatives. These motivators reflect the carriers’ perception that carrier identification is actionable and can save lives.
Similar to previous studies, testing communication and carrier communication were strongly affected by relatives’ gender and degree of relationship.4,5,11,22,23,24,25 At all time points, communication was greater to first- versus second-degree relatives, and to women versus men.
Test communication was often delayed. Two years after testing (Q3), 42% of participants (carriers and noncarriers) reported that they had informed at least one relative only within the previous 6 months. This contrasts with some studies showing that test result disclosure occurs within 1 week to several months, or not at all.11,13 Delayed communication can reflect larger family size or more emotionally or geographically distant relationships, but also deliberate procrastination. In interviews, carriers described waiting for “the right time,” either for technical reasons or to achieve emotional readiness for self-exposure and communication.26
Sociodemographic factors other than family history and enrollment method were not associated with communication of the results, and neither were knowledge, stress (Impact of Events Scale), and perceived control (Perceived Personal Control). Although 44% of responders intended to consult others before familial communication, only 6% actually did so, and the main consultants were health-care providers or another relative. The only psychosocial predictor of actual communication was the SWHD score: the likelihood of communication was sixfold higher in participants whose scores were in the highest versus the lowest quartile (P < 0.001). SWHD was also the single most important predictor of communication in the largest clinic study to date.12 Perhaps individuals with greater internal satisfaction are also more likely to communicate, but these results suggest that familial communication rates are not immutable and predetermined by demographic variables, but rather they could be enhanced by increasing satisfaction with the testing process.
Improving familial communication could perhaps help to minimize the gap we observed between intent to communicate and actual communication. Among all participants, we observed a 37–36% gap for daughters and sisters, a 54–61% gap for sons and brothers, and even greater declines between intent and performance for more distant relatives. Of carrier’s first and second degree relatives, at least 11% and up to 34% were not informed of the familial mutation. This contradicts the consensus expressed by Israelis in previous studies regarding the importance and even perceived “duty” to inform relatives about cancer carrier information.27,28,29
The major goal of carrier communication is cascade testing. In this study, cascade testing was performed in about half of first- and second-degree relatives. Testing rates were higher in first- (58%) than in second-degree relatives (26%) (P = 0.0002) and higher in female than in male relatives (P = 0.02). These rates are comparable to those observed in recent reports of carriers identified in clinical settings, where cascade testing rates were 44% (60% in first- and 28% in second-degree relatives),11 31% (43% in first- and 20% in second-degree relatives),13 and 53%.30 HBOC family history was not found to be associated with carrier communication, and carriers with little or no family history did not mention the lack of family history as a deterrent for informing relatives. Although cascade testing rates in families identified through screening are not lower than in clinically identified families, this and previous studies show that cascade testing falls far short of reaching all relatives at risk. We found that at least 21% of relatives who were not tested were not informed regarding the familial mutation. The main barriers for carrier communication are well known.31 Carriers expressed their reluctance to cause fear and stress in relatives, as well as the hurdles posed by physical and emotional distance.
Limitations
Familial communication and cascade testing were examined in the specific setting of Israeli Ashkenazi Jews. Cascade testing was covered by either the study or the national health system. Thus, applicability of the study results to other populations, countries, and health systems should be determined. Participants were highly educated,15 but this is generally characteristic of persons who undergo recommended screening.32,33 Response rates were partial (Q1: 67%; Q2: 50%; Q3: 43%) and responders were more likely to be female, self-enrolled, and have a family history of HBOC. Cascade testing information was partly based on carriers’ reports, and may be incomplete. Although carriers exemplified a range of characteristics (e.g., significant versus little or no family history, females versus males), their entire sample size was small, which could limit the analysis of family communication among carriers.
Conclusion
In this BRCA screening study, rates and characteristics of testing communication, carrier communication, and cascade testing are comparable to those reported in Cancer Genetics clinics, in the context of personal or family history. This suggests that universal BRCA screening does not differentially affect communication or the use of familial genetic information. While rates of communication to at least one relative were high (97%), 11–34% of relatives remained uninformed, and cascade testing was performed in only about 50% of relatives, similar to the results of previous studies. Satisfaction with being tested (SWHD) was a major predictor of familial communication, suggesting that improving the testing experience may facilitate communication. Further research is necessary to develop such strategies. However, it should be noted that universal screening at least partly preempts dependence on familial communication, since all individuals are tested irrespective of their relatives.
References
Domchek SM, Friebel TM, Singer CF et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 2010;304:967–975.
Domchek SM, Friebel TM, Neuhausen SL et al. Mortality after bilateral salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Lancet Oncol 2006;7:223–229.
Patenaude AF, Dorval M, DiGianni LS, Schneider KA, Chittenden A & Garber JE. Sharing BRCA1/2 test results with first-degree relatives: factors predicting who women tell. J Clin Oncol 2006;24:700–706.
Finlay E, Stopfer JE, Burlingame E et al. Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test 2008;12:81–91.
McGivern B, Everett J, Yager GG, Baumiller RC, Hafertepen A & Saal HM. Family communication about positive BRCA1 and BRCA2 genetic test results. Genet Med 2004;6:503–509.
MacDonald DJ, Sarna L, van Servellen G, Bastani R, Giger JN & Weitzel JN. Selection of family members for communication of cancer risk and barriers to this communication before and after genetic cancer risk assessment. Genet Med 2007;9:275–282.
Hagoel L, Dishon S, Almog R, Silman Z, Bisland-Becktell S & Rennert G. Proband family uptake of familial-genetic counselling. Psychooncology 2000;9:522–527.
French Cancer Genetic NetworkJulian-Reynier C French Cancer Genetic NetworkSobol H French Cancer Genetic NetworkSévilla C French Cancer Genetic NetworkNoguès C French Cancer Genetic NetworkBourret P French Cancer Genetic Network. Uptake of hereditary breast/ovarian cancer genetic testing in a French national sample of BRCA1 families. The French Cancer Genetic Network. Psychooncology 2000;9:504–510.
Landsbergen K, Verhaak C, Kraaimaat F & Hoogerbrugge N. Genetic uptake in BRCA-mutation families is related to emotional and behavioral communication characteristics of index patients. Fam Cancer 2005;4:115–119.
Holloway SM, Bernhard B, Campbell H & Lam WWK. Uptake of testing for BRCA1/2 mutations in South East Scotland. Eur J Hum Genet 2008;16:906–912.
Sanz J, Ramón y Cajal T, Torres A et al. Uptake of predictive testing among relatives of BRCA1 and BRCA2 families: a multicenter study in northeastern Spain. Fam Cancer 2010;9:297–304.
Cheung EL, Olson AD, Yu TM, Han PZ & Beattie MS. Communication of BRCA results and family testing in 1,103 high-risk women. Cancer Epidemiol Biomarkers Prev 2010;19:2211–2219.
Fehniger J, Lin F, Beattie MS, Joseph G & Kaplan C. Family communication of BRCA1/2 results and family uptake of BRCA1/2 testing in a diverse population of BRCA1/2 carriers. J Genet Couns 2013;22:603–612.
Elrick A, Ashida S, Ivanovich J et al. Psychosocial and clinical factors associated with family communication of cancer genetic test results among women diagnosed with breast cancer at a young age. J Genet Couns 2017;26:173–181.
Lieberman S, Tomer A, Ben-chetrit A et al. Population screening for BRCA1/BRCA2 founder mutations in Ashkenazi Jews: proactive recruitment compared with self-referral. Genet Med 2017;19:754–762.
Lieberman S, Lahad A, Tomer A, Cohen C, Levy-Lahad E & Raz A. Population screening for BRCA1/BRCA2 mutations: lessons from qualitative analysis of the screening experience. Genet Med 2017;19:628–634.
Corbin JM & Strauss AL. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd edn. Sage:: Thousand Oaks, CA, 2008.
Denzin NK & Lincoln YS. The Sage Handbook of Qualitative Research. Sage: Thousand Oaks, CA, 2011.
Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE & Neil HA. Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis. Health Technol Assess 2000;4:1–123.
Song FJ, Barton P, Sleightholme V, Yao GL & Fry-Smith A. Screening for fragile X syndrome: a literature review and modelling study. Health Technol Assess 2003;7:1–106.
Morris JK, Law MR & Wald NJ. Is cascade testing a sensible method of screening a population for autosomal recessive disorders? Am J Med Genet A 2004;128A:271–275.
Forrest K, Simpson S, Wilson B et al. To tell or not to tell: barriers and facilitators in family communication about genetic risk. Clin Genet 2003;64:317–326.
Green J, Richards M, Murton F, Statham H & Hallowell N. Family communication and genetic counseling: the case of hereditary breast and ovarian cancer. J Genet Couns 1997;6:45–60.
Hamilton RJ, Bowers BJ & Williams JK. Disclosing genetic test results to family members. J Nurs Scholarsh 2005;37:18–24.
Smith KR, Zick CD, Mayer RN & Botkin JR. Voluntary disclosure of BRCA1 mutation test results. Genet Test 2002;6:89–92.
Nycum G, Avard D & Knoppers BM. Factors influencing intrafamilial communication of hereditary breast and ovarian cancer genetic information. Eur J Hum Genet 2009;17:872–880.
Raz AE & Schicktanz S. Diversity and uniformity in genetic responsibility: moral attitudes of patients, relatives and lay people in Germany and Israel. Med Health Care Philos 2009;12:433–442.
Gilbar R, Shalev S, Spiegel R et al. Patients’ attitudes towards disclosure of genetic test results to family members: the impact of patients’ sociodemographic background and counseling experience. J Genet Couns 2016;25:314–324.
Raz AE & Schicktanz S. Lay perceptions of genetic testing in Germany and Israel: the interplay of national culture and individual experience. New Genet Soc 2009;28:401–414.
Sermijn E, Delesie L, Deschepper E et al. The impact of an interventional counselling procedure in families with a BRCA1/2 gene mutation: efficacy and safety. Fam Cancer 2016;15:155–162.
Chivers Seymour K, Addington-Hall J, Lucassen AM & Foster CL. What facilitates or impedes family communication following genetic testing for cancer risk? A systematic review and meta-synthesis of primary qualitative research. J Genet Couns 2010;19:330–342.
Cooper GS, Kou TD, Dor A, Koroukian SM & Schluchter MD. Cancer preventive services, socioeconomic status, and the Affordable Care Act. Cancer 2017;123:1585–1589.
Smith RA, Manassaram-Baptiste D, Brooks D et al. Cancer screening in the United States, 2015: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2015;65:30–54.
Acknowledgments
This study was supported by a grant from the Breast Cancer Research Foundation (NY) (to E.L.-L.). We thank Rachel Beeri and Esther Korzin Bez for testing BRCA1 and BRCA2 mutations, and Vered Colthof and Halel Dolinsky for administrative assistance in patient recruitment.
Funding: This study was supported by a grant from the Breast Cancer Research Foundation (to E.L.-L.)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lieberman, S., Lahad, A., Tomer, A. et al. Familial communication and cascade testing among relatives of BRCA population screening participants. Genet Med 20, 1446–1454 (2018). https://doi.org/10.1038/gim.2018.26
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2018.26
Keywords
This article is cited by
-
Cascade genetic testing for hereditary cancer syndromes: a review of barriers and breakthroughs
Familial Cancer (2024)
-
Pakistani healthcare professionals’ perceptions of communication with patients and their relatives about hereditary breast cancer: a qualitative study in a LMIC
Journal of Community Genetics (2023)
-
Barriers to completion of cascade genetic testing: how can we improve the uptake of testing for hereditary breast and ovarian cancer syndrome?
Familial Cancer (2023)
-
Cascade testing in Italian Hereditary Breast Ovarian Cancer families: a missed opportunity for cancer prevention?
Familial Cancer (2023)
-
“What does not kill you… mutates and tries again.” A study on personality determinants of post-traumatic growth during the COVID-19 pandemic
Current Psychology (2023)