Abstract
Purpose
The purpose of this study was to model the performance of several known two-tier, predefined mutation panels and three-tier algorithms for cystic fibrosis (CF) screening utilizing the ethnically diverse California population.
Methods
The cystic fibrosis transmembrane conductance regulator (CFTR) mutations identified among the 317 CF cases in California screened between 12 August 2008 and 18 December 2012 were used to compare the expected CF detection rates for several two- and three-tier screening approaches, including the current California approach, which consists of a population-specific 40-mutation panel followed by third-tier sequencing when indicated.
Results
The data show that the strategy of using third-tier sequencing improves CF detection following an initial elevated immunoreactive trypsinogen and detection of only one mutation on a second-tier panel.
Conclusion
In a diverse population, the use of a second-tier panel followed by third-tier CFTR gene sequencing provides a better detection rate for CF, compared with the use of a second-tier approach alone, and is an effective way to minimize the referrals of CF carriers for sweat testing. Restricting screening to a second-tier testing to predefined mutation panels, even broad ones, results in some missed CF cases and demonstrates the limited utility of this approach in states that have diverse multiethnic populations.
Similar content being viewed by others
Introduction
Several recent publications have focused on the effectiveness of predefined mutation panels and sequencing of the cystic fibrosis transmembrane conductance regulator (CFTR) gene as a second- or third-tier approach to screening after an initial elevation of immunoreactive trypsinogen (IRT) in newborn screening.1, 2, 3, 4 In particular, Baker et al.5 showed that most of the mutations in the Wisconsin population could be identified, and proposed a model that refers for sweat chloride testing only those infants with two known mutations identified among a panel of 48 cystic fibrosis causing mutations maintained by the CFTR2 project.6
The authors endorse the idea of looking for two mutations in second-tier testing after an initial elevation of IRT in order to minimize the referral of carriers for follow up. However, our concern was that restricting the genetic test to a second-tier predefined mutation panel, even a very broad panel, would result in missed cases due to previously unreported or private mutations especially in minority populations.7 In order to compare the efficacy of different screening approaches, we compared the performance of several two-tier models using predefined mutation panels that are used by other state newborn screening programs and the California (CA) three-tiered approach, which uses a predefined mutation panel that was customized to reflect the ethnic diversity of the state followed by further sequencing of the CFTR gene.
In some other states, two specimens are routinely collected on all newborns. In these programs, a three-tier model of CF screening measures IRT in the first specimen, IRT in the second specimen, and DNA in a defined subset. This model is not under consideration in this paper.
Materials and methods
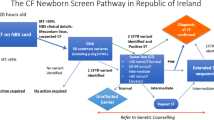
A recent publication has described the California CF newborn screening program in detail.2 After an initial elevated IRT level, a newborn’s specimen has a second-tier test using a select panel of 40 CFTR mutations chosen to cover our ethnically diverse population. Cases with two identified mutations are referred for follow up immediately. Cases with one mutation have third-tier sequencing of exons and critical intronic areas of the CFTR gene.8
We first defined a retrospective cohort of babies who were screened in California between 12 August 2008 and 18 December 2012 and were subsequently identified with CF, including CF cases missed by our screening program but later reported to us. We then reviewed the mutation data for these cases. The dates were chosen to define an interval during which no aspect of the California CF screening changed: neither the cutoff for the initial IRT determination, nor the mutations on the second-tier mutation panel. Restricting to a cohort that is at least four years old also allowed for the ascertainment of the CF cases that the California Newborn Screening Program (NBS) missed, that were subsequently identified clinically and then reported to us by the cystic fibrosis follow-up care centers in California. We retained all CF cases with available mutation data.
The most common mutation panel is the one developed by the American College of Medical Genetics and Genomics (ACMG) for CF-carrier screening, which consists of 23 mutations.9 The ACMG panel and the CA panel share 14 mutations. In contrast, the CFTR2 project listed more than 250 mutations in August 2015, and categorized them into (i) CF-causing, (ii) non-CF-causing, (iii) mutations of variable clinical significance, and (iv) mutations of unknown significance. Two mutations (F311del and Q98R) on the CA panel were not listed in the CFTR2 database as of August 2015.
We reviewed mutation information for each CF case in the California cohort and assigned mutations to seven hierarchical and mutually exclusive groups: (i) the ACMG and CA panels combined, (ii) the ACMG panel only, (iii) the CA panel only, (iv) the panel of CFTR2 CF-causing mutations, (v) the CFTR2 CF mutations with variable or unknown significance, (vi) the CFTR2 non-CF-causing group, and (vii) mutations not on any panel nor in the CFTR2 database. For the last group, mutations not listed by any panel or CFTR2 database, we conducted literature and Internet searches, and identified those that had never been reported as novel.
In order to minimize the referral of CF carriers for follow up, we concentrated on screening strategies that look for two mutations. We divided the strategies into those that look for both mutations on the same predefined panel or list of mutations (the ACMG panel, the CA panel, or the CFTR2 CF-causing list), and an alternative strategy that looks for one mutation on one of the predefined panels or lists and then looks for a second mutation on a much broader list (either all of CFTR2 CF-causing mutations or any mutation found by broader sequencing). Our primary measure was the detection rate among our cohort of CF cases.
The race, ethnicity, or ancestry of the newborn was self-reported by the parents. We characterized each CF case into five single-race categories: (i) Hispanic; (ii) Black; (iii) White and Middle Eastern as white; and (iv) Chinese, Japanese, Korean, Cambodian, Laotian, Vietnamese, Filipino, Other Southeast Asian, and East Indian as Asian; and (v) all other ancestries or races including unknown race as Other/Unknown.
Results
Between 12 August 2008 and 18 December 2012, there were 2,212,915 newborns screened in California. Table 1 presents the race/ethnicity/ancestry profile of the cohort of newborns screened during this period and the distribution of race/ethnicity among the CF cases subsequently diagnosed in the cohort. Two cases were omitted because they had no known genetic information. As expected, whites (41.6%) were overrepresented in the CF population, with an incidence rate of 1 in 4,300, although they only represented 25.6% of total births. Hispanics, which made up the largest population group (41.9%), accounted for 31.2% of the CF cases; and Asians, which represented 9.0% of the screened population, accounted for 1.9% of CF cases. The California screening program identified 95.5% of white CF babies, but only 66.7% of Asian CF babies (4 of 6), the group with the lowest CF rate of 1/33,300. Over 90% of babies with Hispanic, black, or other ethnicity were identified by the program. One hallmark of the ethnicity difference is that only 11 of the 132 white cases that were sequenced included mutations that were either novel or not in CFTR2 or identified in CFTR2 as not disease causing. In contrast, this was true of 31 of the 99 Hispanic cases, 4 of the 14 black cases, and 3 of the 6 Asian cases.
The mutation pairs from the CF cases listed in Table 2 were classified into mutually exclusive groups based on their informatics source, whether ACMG, CA mutation panel, CFTR2, or in combination. Most mutation pairs identified among CF cases were included in one or several informatics sources. However, a total of 57 known CF cases had one mutation that was listed as non-CF-causing in the CFTR2 (2 cases) or was not in the CFTR2 list at all (55 cases). An additional 11 cases had a single panel mutation and a poly-T tract mutation. Fully 21% (68 out of 317) of California CF cases would have been missed using the broadest panel available.
With the information about each individual CF mutation, combined with the knowledge of the informatics source that it is associated with, we can apply various screening strategies to see how effective each strategy was. The basic outcome measure is the percentage of the cohort that is identified, i.e., the detection rate. These results are reported in Table 3.
All two-tier predefined panel approaches benefited from including the CRTR2 CF-causing mutations as part of a tier 3 test, such that the CA panel increased from 53 to 70% detection and the ACMG panel increased from 47 to 68% detection. The biggest improvement resulted from using the current CA panel followed by broad sequencing, which yielded a 97% detection rate for the California cohort of CF cases.
During this time period, 2,049 cases were sent for third-tier sequencing, having a single identified mutation from the California panel. Of them, 1,333 did not have a second mutation identified and were offered telephone genetic counseling as carriers. The remaining 716 were referred to a CF Center, where evaluation of the significance of the mutation, physical examination, and sweat testing allowed them to be characterized as 122 CF carriers, 141 CF cases, and 453 cases of CFTR-related metabolic syndrome (CRMS).
The advantage of adding the larger CFTR2 CF-causing panel or tier-3 sequencing to find the second mutation is particularly significant for minority populations. In these groups, moving from the ACMG panel to the ACMG panel plus CFTR2 CF-causing panel increased the detection by 29% in Hispanic cases, 28% in black cases, and 21% in cases of other race/ethnicities. Similarly, moving from the CA panel to the CA panel plus CFTR2 CF-causing increased the detection rate by 17% in Hispanic cases, 29% in black cases, and 17% in cases of other race/ethnicities. The improvement in moving to the current CA approach (CA panel plus broad sequencing) was even more dramatic, with a detection rate of 93% for Hispanic and black cases, and 91% of cases of other race/ethnicities. The CFTR2 panel showed similar significant improvement with third-tier sequencing. Only sequencing showed improvement in the detection of the small number of Asian CF cases.
Finally, among the mutations not listed in CFTR2, there are 10 that are also not listed in the CF Mutation Database.10 These novel mutations are listed in Table 4.
Discussion
At this point there should be little question that two- and three-tier molecular testing of the CFTR gene is an effective tool for follow-up screening after an initial elevated IRT result. Use of three-tier multiple-CFTR-mutation testing improves sensitivity, especially among nonwhite populations, who have not been well represented in the current CF screening panels. However, there is a concern that this improvement comes at a cost of increased referrals and carrier identification.1 Therefore, the challenge becomes how best to apply this technology to improve the screening algorithm and maximize sensitivity and specificity to both detect the maximum number of cases among all race/ethnic groups and to minimize the number of carriers sent for follow-up testing. The impact of a second novel variant identified through sequencing (in combination with a known disease-causing mutation) will require long term follow-up and eventual functional testing of these newly discovered mutations. The findings from this paper suggest that the strategy of requiring two mutations for follow-up, but allowing those mutations to be from a mutation panel proven pathogenic in a specific population followed by sequencing of CFTR for newborns identified with one mutation, would produce the optimal results with respect to clinical sensitivity and specificity.
One problem with the ACMG panel, and, to a lesser extent, all predefined panels, is that the mutations particular to minority populations may be underrepresented. This deficiency can arise because the panel was targeted for a specific population or because the mutations common only in minority populations have been studied far less. We found that 21% of CF cases had at least one mutation that was not on any panel and that combinations of panels only identified 70% of CF cases in California. In contrast, the current CA approach of a panel followed by sequencing yielded detection of 93% of CF cases. In their recent publication, Schrijver et al. listed the 50 most common mutations in white, Hispanic, black, Asian, and Native American populations.7 Mutations unique to one ethnic group comprised 8% of the white, 40% of the Hispanic, 28% of the black, 36% of the Asian, and 14% of the Native American lists. The ACMG panel was not designed for screening diverse populations; it does not include any mutations that are not in the top 50 for the white ethnicity. Although the CA panel does include some mutations specific to the Hispanic, black, and Asian ethnicities, our current publication will provide data to consider regarding the appropriate selection of additional mutations.
The approach currently used in California is similar in concept to NextGen sequencing where an initial, predefined, second-tier panel is run simultaneous to a deep scan that is masked. If the panel results identify two CF-causing mutations, the child is referred immediately. If only one mutation is found, then the deep scan is revealed via bioinformatics and any additional CF-causing mutations found are used as a third tier to determine referral. The difference between the two methodologies is that the full three-tier NextGen procedure is quicker, and is run on all IRT-positive blood samples. California runs a predefined panel first, but must wait up to one month, for the small number sequencing results.
One goal of all screening programs is to minimize the impact of false positive results. By limiting diagnostic evaluation to babies who have two identified mutations, the California programs resolved two-thirds of the cases with one panel mutation and avoided unnecessary sweat testing. While more cases of CRMS are identified than CF, it is important to recognize that the symptoms associated with CRMS have a wide range, and some of these children do eventually progress to CF.11, 12 We hope that it is more helpful to avoid a later diagnostic odyssey that parents and children with undiagnosed CRMS may face when CF symptoms later emerge after initial screening results ruled out CF.
The just-published consensus guidelines from the CF Foundation13 include specific recommendations for CRMS/CFSPID (CF screen positive, inconclusive diagnosis), which include criteria for diagnosis of CRMS/CFSPID, the need for sweat testing, the need for appropriate clinical evaluation to find the small number of CRMS/CFSPID that develop clinical symptoms, and the appropriateness of genetic counseling for these families. Eight out of 27 recommendations addressed CRMS/CFSPID specifically. Recommendation 24 acknowledges that infants “with a designation of CRMS/CFSPID (by definition) do not have clinical features consistent with a diagnosis of CF and further research is needed to determine the prognosis and best practices for frequency and duration of follow-up.” There is an impetus implicit in the guidelines for families to remain on high alert for a later onset of CF symptoms.
In contrast, in a comprehensive study of the parents of children identified with CF, either clinically or through newborn screening, Grob14 states that the “mixture of absolute surprise and full-throttle panic about what a positive newborn screening test means is paradigmatic of parents’ NBS experiences” (p. 46). Later, there is an extensive comment on what we would characterize as CRMS:
For another subset of parents, the jarring juxtaposition of disease labeling and good health that begins with NBS diagnosis lasts for months, years, or indefinitely. For these families, CF diagnosis turns out to be a complicated genetic profile that may or may not result in any manifestation of illness. A CFTR mutation has been identified and the result has been given to the parent, but the child is healthy and may well remain so into adulthood or throughout life. In many instances where children manifest no illness, it is unclear whether the preventive care regimen has in fact been essential for maintaining their good health, or whether their particular genetic makeup would have kept them symptom-free regardless of early diagnosis and prophylactic treatment14 (p. 55).
Attempting to reconcile these two disparate perspectives on CRMS suggests to us the necessity of future study not only of the natural history of CRMS cases, their prognosis, and best options for clinical follow-up, but also of the psychosocial impact on families, the availability of appropriate support services including genetic counseling, and the long-term impact on family dynamics of these challenging diagnoses.
One of the limitations of this study is that it contains only cases from California. Although more ethnically diverse than many states, even California does not represent the whole spectrum of CF mutations that exist around the world. There also may be a small number of missed cases that have not yet come to our attention, either because of a gradual onset of somewhat nonspecific symptoms or because of demise before diagnosis. In addition, race and ancestry information is self-reported and can be inaccurate, incomplete, or imprecise. We classified children of mixed-race and heterogeneous ancestry into a large category of Other, which may warrant future scrutiny and analysis.
A second limitation of the study is the unavailability of functional testing or other assessment of the pathogenicity of the novel mutations reported in Table 4. One can anticipate that the mutations causing frame shifts or destruction of the canonical splice site motifs will not generate functional protein. Nonsynonymous substitutions will require additional testing or analysis to understand their implications for disease.
Cystic fibrosis continues to be a challenge for newborn screening programs around the world. Ongoing research to identify the mutations found in different populations is essential. This paper suggests that the incorporation of sequencing into newborn screening for CF may play an important role in this research. Perhaps even more important is the need for ongoing curation of the repositories of clinical information regarding individual mutations so that it is possible to assess the significance of mutations as they are identified in particular patients. New approaches to CF screening continue to emerge. With commitment and diligence, one day we may be able to provide screening with unprecedented specificity and sensitivity.15
References
Comeau AM, Parad RB, Dorkin HL et al, Population-based newborn screening for genetic disorders when multiple mutation DNA testing is incorporated: a cystic fibrosis newborn screening model demonstrating increased sensitivity but more carrier detections. Pediatrics 2004;113:1573–1581.
Kharrazi M, Yang J, Bishop T et al, Newborn screening for cystic fibrosis in California. Pediatrics 2015;136:1062–1072.
Wells J, Rosenberg M, Hoffman G, Anstead M, Farrell PM . A decision-tree approach to cost comparison of newborn screening strategies for cystic fibrosis. Pediatrics 2012;129:e339–e347.
Ranieri E, Lewis BD, Gerace RL et al, Neonatal screening for cystic fibrosis using immunoreactive trypsinogen and direct gene analysis: four years' experience. BMJ 1994;308:1469–1472.
Baker MW, Atkins AE, Cordovado SK, Hendrix M, Earley MC, Farrell PM . Improving newborn screening for cystic fibrosis using next-generation sequencing technology: a technical feasibility study. Genet Med 2016;18:231–238.
Castellani C, on behalf of team C. CFTR2: how will it help care? Paediatr Respir Rev 2013;14 (suppl 1): 2–5.
Schrijver I, Pique L, Graham S, Pearl M, Cherry A, Kharrazi M . The spectrum of CFTR variants in nonwhite cystic fibrosis patients: implications for molecular diagnostic testing. J Mol Diagn 2016;18:39–50.
Stanford Health Care CFTR Screen by Sequencing (CFSS). http://www.stanfordlab.com/esoteric/test-cftr-screen-by-sequencing.html (Accessed 13 April 2016).
Watson MS, Cutting GR, Desnick RJ et al, Cystic fibrosis population carrier screening: 2004 revision of American College of Medical Genetics mutation panel. Genet Med 2004;6:387–391.
Cystic Fibrosis Mutation Database, 2016. http://www.genet.sickkids.on.ca/Home.html (Accessed 3 May 2016).
Ren CL, Desai H, Platt M, Dixon M . Clinical outcomes in infants with cystic fibrosis transmembrane conductance regulator (CFTR) related metabolic syndrome. Pediatr Pulmonol 2011: 461079–461084.
Ren CL, Fink AK, Petren K et al, Outcomes of infants with indeterminate diagnosis detected by cystic fibrosis newborn screening. Pediatrics 2015;135:e1386–e1392.
Farrell PM, White TB, Ren CL et al, Diagnosis of cystic fibrosis: consensus guidelines from the Cystic Fibrosis Foundation. J Pediatr 2017;181S (S4–S15): e11.
Grob R . Testing Baby: The Transformation of Newborn Screening, Parenting and Policymaking. Rutgers University Press: Piscataway, NJ, 2011.
Lefterova MI, Shen P, Odegaard JI et al, Next-generation molecular testing of newborn dried blood spots for cystic fibrosis. J Mol Diagn 2016;18:267–282.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Currier, R., Sciortino, S., Liu, R. et al. Genomic sequencing in cystic fibrosis newborn screening: what works best, two-tier predefined CFTR mutation panels or second-tier CFTR panel followed by third-tier sequencing?. Genet Med 19, 1159–1163 (2017). https://doi.org/10.1038/gim.2017.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.32
Keywords
This article is cited by
-
Expanding the Australian Newborn Blood Spot Screening Program using genomic sequencing: do we want it and are we ready?
European Journal of Human Genetics (2023)
-
Racially equitable diagnosis of cystic fibrosis using next-generation DNA sequencing: a case report
BMC Pediatrics (2021)
-
Evaluating sequence data quality from the Swift Accel-Amplicon CFTR Panel
Scientific Data (2020)
-
A brief history of human disease genetics
Nature (2020)