Abstract
Purpose
Benzoate and phenylbutyrate are widely used in the treatment of urea cycle disorders, but detailed studies on pharmacokinetics and comparative efficacy on nitrogen excretion are lacking.
Methods
We conducted a randomized, three-arm, crossover trial in healthy volunteers to study pharmacokinetics and comparative efficacy of phenylbutyrate (NaPB; 7.15 g•m−2BSA•day−1), benzoate (NaBz; 5.5 g•m−2BSA•day−1), and a combination of two medications (MIX arm; 3.575 g NaPB and 2.75 g NaBz•m−2BSA•day−1) on nitrogen excretion. Stable isotopes were used to study effects on urea production and dietary nitrogen disposal.
Results
The conjugation efficacy for both phenylbutyrate and benzoate was 65%; conjugation was superior at the lower dose used in the MIX arm. Whereas NaPB and MIX treatments were more effective at excreting nitrogen than NaBz, nitrogen excretion as a drug conjugate was similar between phenylbutyrate and MIX arms. Nitrogen excreted per USD was higher with combination therapy compared with NaPB.
Conclusion
Phenylbutyrate was more effective than benzoate at disposing nitrogen. Increasing phenylbutyrate dose may not result in higher nitrogen excretion due to decreased conjugation efficiency at higher doses. Combinatorial therapy with phenylbutyrate and benzoate has the potential to significantly decrease treatment cost without compromising the nitrogen disposal efficacy.
Similar content being viewed by others
Introduction
The urea cycle is the main pathway in humans for the disposal of waste nitrogen derived from catabolism of dietary and endogenous proteins. Deficiency of one of the enzymes or transporters required for ureagenesis (Supplementary Figure S1 online) causes urea cycle disorders (UCDs), a group of inborn errors of metabolism characterized by a decreased ability to dispose nitrogen and subsequent accumulation of ammonia in tissues and blood. Hyperammonemia can have serious consequences, and if severe, can result in intellectual disability, neurocognitive deficits, and even coma and death.1 Thus, the main focus of treatment for UCDs is the prevention and treatment of hyperammonemia.
Nitrogen-scavenging medications, which use alternative pathways to dispose nitrogen, have become a standard of care for the prevention and treatment of hyperammonemia in UCDs.2,3 For long-term management, oral formulations of benzoate and phenylbutyrate are the commonly used alternative pathway therapies. Benzoate combines with glycine to form hippuric acid (HA). Phenylbutyrate, a prodrug, is converted to phenylacetate (PAA) by β-oxidation; PAA conjugates with glutamine to form phenylacetylglutamine (PAGN) (Figure 1). Because glutamine has two nitrogen atoms compared with one in glycine, theoretically, on a mole-per-mole basis, nitrogen-scavenging efficacy of phenylbutyrate should be twice that of benzoate. However, in vivo efficacy is dependent on medication absorption, conversion into active metabolite, and the efficacy of conjugation with amino acids. The conversion of benzoate into HA has been estimated to range from 65% to virtually 100%.4,5 Similarly, the conversion of phenylbutyrate to PAGN ranges from 50% to over 90%.5,6
With a block in ureagenesis, excretion of conjugates of amino acids can serve as an alternative mechanism for disposal of nitrogen. Benzoate and phenylacetate can be conjugated with glycine and glutamine, respectively, to generate hippuric acid and phenylacetylglutamine. The nitrogen atoms scavenged by these medications is depicted by gray circles. Whereas one molecule of benzoate scavenges one atom of nitrogen, one molecule of phenylacetate scavenges two atoms of nitrogen.
To date, the comparative in vivo efficacy of phenylbutyrate and benzoate on nitrogen excretion in humans has not been systematically studied. In fact, detailed pharmacokinetic studies of either medication in individuals with UCDs were lacking until recently, when basic kinetic studies were performed with sodium phenylbutyrate as a part of studies comparing it with glycerol phenylbutyrate, a pre-prodrug.6 Moreover, even preclinical data on efficacy are lacking due to the absence of suitable models as animals other than primates conjugate glycine with phenylacetate.7,8 Despite of the lack of evidence, the theoretical advantage of phenylbutyrate over benzoate is likely one of the reasons for the preferential use of phenylbutyrate formulations (sodium phenylbutyrate and glycerol phenylbutyrate) in the United States. This approach, however, increases the economic burden of therapy as phenylbutyrate formulations are far more expensive than benzoate.9 A direct comparison between phenylbutyrate and benzoate and exploring the utility of combinatorial therapy with both medications would be of value in devising cost-effective management strategies for UCDs. The goal of this randomized crossover study was to determine the pharmacokinetics of phenylbutyrate and benzoate, the efficacy of the medications on nitrogen excretion, and the potential utility of combination therapy with both medications.
Materials and methods
The study was conducted at Baylor College of Medicine, Texas Children’s Hospital, and Children’s Nutrition Research Center in Houston, Texas. The study procedures were approved by the Baylor College of Medicine Institutional Review Board. Informed consent was obtained from all participants. Healthy adult volunteers (age ≥18 years) were recruited. Individuals with the following were excluded from the study: (i) history of dietary protein intolerance, (ii) history of liver diseases, (iii) inability to follow the prescribed diet or undergo the isotopic infusions, (iv) documented history of hyperammonemia (defined as plasma ammonia >100 μmol/L), (v) clinical or laboratory abnormality of grade 3 or greater according to the Common Terminology Criteria for Adverse Events v.4.0, and (vi) any condition(s) not covered by the Criteria for Adverse Events but that the investigators considered a severe condition. Pregnant or lactating women were not enrolled.
Study design
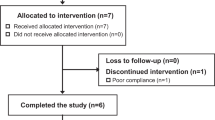
This was a randomized, three-arm, crossover study. Each arm was completed over a 4-day period with a washout period of at least 7 days between any two of the treatment arms (Figure 2). The treatment sequence was randomized in a nonblinded manner. The treatment and doses of the medications used were as follows: (i) NaPB arm: phenylbutyrate 7.15 g•m−2 of body surface area (BSA)•day−1, maximum dose, 20 g•day−1; (ii) NaBz arm: benzoate 5.5 g•m−2 of BSA•day−1, maximum dose, 12 g•day−1; and (iii) MIX arm: phenylbutyrate and benzoate, 3.575 and 2.75 g•m−2 of BSA•day−1, respectively (half the dose used in the NaPB and NaBz arms). The treatments were designed to provide isomolar amount of drugs and the total daily dose was administered in three equally divided doses. The doses of medications used in the study is representative of the typical doses that are used in the management of adults with UCDs.10
Every subject was crossed over to receive all three study medications, i.e., phenylbutyrate, benzoate, and combination of phenylbutyrate and benzoate at half the dose. On day 4, after consuming the test meal (0.4 g protein/kg) labeled with 15N spirulina, the subjects were administered the corresponding drugs and a urea tracer (13C18O urea). Blood and urea were sampled as indicated. H&P, history and physical examination; Safety labs, complete blood count, comprehensive metabolic panel, plasma ammonia, and urinalysis. *Safety labs in study arms 2 and 3 were repeated only if abnormalities were noted on safety labs from day 4 of the preceding study arm or if the washout period was greater than 28 days from the preceding treatment arm.
On day 1 of study arm 1, detailed medical history review and physical examination were performed. Complete blood count, comprehensive metabolic panel, plasma ammonia, and urinalysis (safety laboratory measurements) were performed. Urine pregnancy test was performed on all females. Meals prepared at the Children’s Nutrition Research Center to provide 0.8 g•kg−1•day−1 protein and 32 kcal•kg−1•day−1 were given for the next 3 days. The standardized protein and caloric intake allowed for comparison of nitrogen excretion among the three arms. Subjects were randomized to a predetermined treatment sequence and the first dose of the appropriate medication was administered under supervision. Subjects took the study medication with meals for 3 days (8:00 am breakfast; 1:00 pm lunch; 7:00 pm dinner) (Figure 2). The treatment period of 3 days was chosen to allow for metabolic adaptations to the study medication as previously published.11 On day 3, subjects omitted the 7:00 pm dose of the medication to prevent interference with the analysis on day 4 from metabolite conjugates from the previous day. On day 4, at ~8:00 am and after placing a catheter (Insyte Autoguard, Becton Dickinson, Franklin Lakes, NJ) on a superficial hand vein, a fasting blood sample was obtained for the determination of plasma amino acids and urea concentrations, background isotopic enrichments, basic metabolic profile, complete blood count, and plasma concentrations of phenylbutyrate, benzoate, PAGN, and HA. Urine was collected for measurements of urea, phenylbutyrate, benzoate, PAGN, and HA. At 0 h, the test meal containing half of the daily dietary allowance of protein (0.4 g•kg−1) was provided by a commercial liquid meal replacement (Ensure Plus, Abbott, Abbot Park, IL) and 15N labeled spirulina (40 mg•kg−1; ISOTEC, Miamisburg, OH). Spirulina is a natural source of protein from cyanobacteria that contains ~50% true protein and all essential amino acids.12 A dose of 40 mg•kg−1 labeled 15N-labeled spirulina was estimated to result in dietary 15N enrichment of ~5 mole percent excess. The test meal, which was ingested in ~10 min, was followed by a dose of study medication and an intravenous bolus dose of urea tracer, [13C18O]urea (6 mmol/subject; ISOTEC, Miamisburg, OH). Blood samples to determine concentrations and isotopic enrichments of the drugs and their conjugated products, as well as amino acids and urea, were collected every 30 min for the first 4 h and then hourly between hours 4 and 8 (Figure 2). Urine was collected in four 2-h batched periods during the 8-h admission period. The subjects then received a meal with the rest of the daily allowance and were discharged; the urine collection continued at home for the next 16 h for a total 24-h collection period. The procedures for the study arms 2 and 3 were identical to those performed in arm 1.
Sample analysis
The concentrations of drugs13 and their conjugates as well as urea14 and amino acids15 were determined by mass spectrometry and quantitated based on the dilution of labeled internal standards as previously published (Supplementary Information). Total urinary nitrogen was determined using the micro-Kjeldahl method.16
Calculations
Pharmacokinetic parameters, peak concentration (Cmax), time to achieve Cmax for drugs and their conjugated products (Tmax), and area under the curve for 8 h after drugs ingestion (AUC0–8) were determined using previously published methodology.17 Urea production was determined by noncompartmental analysis after fitting a biexponential model to the [13C18O] urea enrichment data.18,19
The total amount of nitrogen conjugated by drugs was calculated by multiplying the weight of 24 h urine, the concentration of the metabolite of interest, and the nitrogen content of the metabolite. We detected PAGN and HA in the urine of subjects during treatment arms in which they were not receiving phenylbutyrate or benzoate, respectively. Accordingly, these background values were subtracted from the values obtained during the treatment with phenylbutyrate and benzoate. The total amount of nitrogen conjugated was expressed as a fraction of the test meal, by dividing by the total nitrogen content of the test meal. The conjugation of dietary nitrogen was calculated as the amount of 15N conjugated by multiplying the total amount of nitrogen conjugated by the respective 15N enrichment. For PAGN, the labeling of the amino and amido groups of glutamine was considered.
Efficacy of drug conjugation, the technical relationship between the drug and its effects, was determined by dividing the amount of nitrogen conjugated by the amount of drug provided (in a molar and gram basis).20 Efficiency, an economic concept that relates efficacy to resource use, was calculated by dividing the amount of nitrogen conjugated by the estimated cost of phenylbutyrate (24.7 USD/g) and benzoate (0.03 USD/g) at our institution.21
Statistical analysis
Data were analyzed using the proc mixed procedure of SAS (v. 9.4; SAS Institute, Cary, NC) with subject as the random variable of the model; thus comparisons were done within subject. If a statistically significant effect for a particular treatment arm was observed (P < 0.05), post hoc Tukey procedure was performed for multiple pairwise comparisons. Data are expressed as means ± SEM.
Results
Seven individuals (five males, two females) were enrolled. The demographic characteristics and the treatment sequences are outlined in Supplementary Table S1.
Pharmacokinetics of phenylbutyrate, benzoate, and their conjugated products
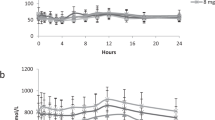
After a 3-day treatment adaptation, pharmacokinetics were determined following a single drug dose on day 4 (Table 1, Supplementary Figure S2). Tmax for phenylbutyrate and benzoate were not different whether the drugs were given alone or in combination (P > 0.28). Tmax for PAA was greater than Tmax for phenylbutyrate (P < 0.001), and tended to be greater in the NaPB arm as compared with the MIX arm (P = 0.086). As expected, Cmax and AUC0–8 were greater when the drugs were given alone as compared with half the dose in the MIX arm. The Cmax and AUC0–8 of phenylbutyrate and PAA were ~2–3 times greater when subjects were on the NaPB arm than on the MIX arm. Benzoate Cmax and AUC0–8 were ~4–5 times greater when subjects were on the NaBz arm than on the MIX arm.
For the conjugation products, Tmax for PAGN was greater than for HA (P < 0.01). For PAGN, no difference in Tmax was observed between the NaPB and MIX arms (P = 0.104); however, hippurate Tmax was greater on the NaBz arm than in the MIX arm (P < 0.008). As expected, Cmax and AUC0–8 for PAGN and HA were greater when phenylbutyrate and benzoate were given solely in the NaPB and NaBz arms as compared with the MIX arm (P < 0.014) (Table 1, Supplementary Figure S2). A similar pattern was detected for the conjugation of the drugs with 15N-labeled glutamine and glycine resulting from the ingestion of the 15N-labeled test meal (Table 1).
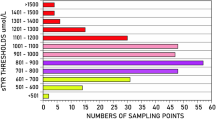
Urinary excretion of phenylbutyrate, benzoate, and their conjugated products
The urinary excretion of phenylbutyrate, PAA, and benzoate was negligible (Table 2). Urine contained an average of 0.8 ± 0.1 mmol/d of PAGN and 1.7 ± 0.3 mmol/d of HA even when phenylbutyrate and benzoate, respectively, were not administered. After adjusting for these background values, the efficacy of conjugation, i.e., percent of phenylbutyrate dose recovered as PAGN and percent of benzoate dose recovered as HA in 24 h urine were determined. The efficacy of conjugation (~65%) was similar for phenylbutyrate and benzoate when given as the sole treatments (P = 0.59); however, conjugation efficacy of phenylbutyrate was greater with the lower dose administered in the MIX arm as compared with the NaPB arm (P < 0.044). Similar trend was observed for benzoate (P = 0.058). A treatment effect (P < 0.004) was observed for the total amount of nitrogen excreted as conjugated products. NaPB and MIX treatments were more effective at conjugating and excreting nitrogen than the NaBz treatment (Table 2). However, no differences (P = 0.19) among the three treatment arms were detected for the conjugation and excretion of 15N originating from the test meal (Table 2).
The efficacy of nitrogen conjugation and excretion was greater for the NaPB and MIX arms as compared with the NaBz arm regardless of whether it was expressed on a per-molar (P < 0.004) or per-gram basis (P = 0.032) (Table 2). Nitrogen excretion as a drug conjugate was similar between the NaPB and the MIX arms, suggesting that combinatorial therapy could be as effective as therapy with NaPB. The efficiency of drug utilization (i.e., the amount of drug conjugated per dollar), however, was higher for the NaBz arm, followed by the MIX arm (Table 2).
Effect of benzoate and phenylbutyrate on plasma amino acids
There was no treatment effect on glutamine (P = 0.15) or glycine (P = 0.13) AUC0–8 (Supplementary Figure S3). A treatment effect, however, was detected for leucine AUC0–8 (P < 0.01), which showed a reduction in subjects on the NaPB treatment. This was not evident for the other branched-chain amino acids and other amino acids analyzed. The exception was tryptophan, which showed a strong treatment effect (P < 0.001), with a reduction in AUC0–8 in response to phenylbutyrate (P < 0.001; Supplementary Figure S3). The ingestion of the 15N-labeled test meal resulted in the 15N enrichment of all plasma amino acids, which peaked around 3–4 h (data not shown). Substantial 15N amino acid enrichments were still observed 8 h after the test meal (data not shown).
Effect of phenylbutyrate and benzoate on urea metabolism and total urinary nitrogen excretion
There was no treatment effect on plasma urea concentration (P = 0.16) and urea production (P = 0.80) for any of the three treatment arms (Table 3). Likewise, there was no effect of treatment on total nitrogen (P = 0.67) or urea-nitrogen excretion (P = 0.74). Total urinary nitrogen excretion accounted for ~67% of the dietary nitrogen and urinary urea nitrogen accounted for ~65.5% of the total urinary nitrogen. Similarly, there was no treatment effect on urea 15N excretion (P = 0.94); on average urea excretion accounted for ~15% of the test meal nitrogen (Table 3).
Discussion
In the early 1980s, Saul Brusilow and Mark Batshaw22,23,24 made the serendipitous discovery of the utility of benzoate and phenylacetate for nitrogen disposal in UCDs. Currently, benzoate and formulations of phenylbutyrate are widely used in the long-term management of UCDs. Benzoate is available as a generic compound and is widely used as a food preservative; however, it has not been specifically approved by the US Food and Drug Administration for the treatment of UCDs, which can sometimes pose a challenge for procuring prescription coverage. Whereas generic formulations of phenylbutyrate exist, for the most part, the availability of phenylbutyrate formulations is restricted. In the United States, the trademarked formulations of both sodium phenylbutyrate and glycerol phenylbutyrate are marketed by the same pharmaceutical company. In addition to the standard formulations of sodium phenylbutyrate, a taste-masked granule formulation is also available in Europe and Canada, but not in the United States.25,26 Over the past two decades, nitrogen-scavenging medications have become a standard of care in the treatment of UCDs, and their use, at least in part, has contributed to the increased survival.2,27 However, the cost of treatment and access to medications are far from ideal.9 In patients who are able to get medications, the increase in number of pills and side effects associated with higher doses of medications can affect compliance.28 Whereas chronic treatment with phenylbutyrate in UCDs has generally been safe, phenylbutyrate affects many physiologic processes through its actions on transcription, inhibition of histone deacetylation, and modulation of endoplasmic reticulum stress, among others.29,30,31 Few of these off-target effects, such as a decrease in the plasma levels of branched-chain amino acids, may be of direct relevance in the management of UCDs.32 Understanding the comparative efficacy of nitrogen-scavenging medications and exploring combinatorial therapy would be an important first step in devising effective and affordable treatment regimens for UCDs.
In this study, we demonstrate that the efficacy of phenylbutyrate to conjugate and excrete nitrogen was greater than that of benzoate. However, as expected, none of the drugs conjugated completely and the efficacy of drug conjugation with its target amino acid at the highest dose of each drug was ~65%. Although some other metabolites may also be excreted,33 quantitatively they seem to be negligible. Neutral loss scans of urine by tandem mass spectrometry, to detect the loss of the phenyl ring from unknown molecules, allowed us to identify phenylbutyrylglutamine; however, due to its low abundance we did not attempt to quantify this compound. Interestingly, the conjugation efficacy was greater when lower doses of phenylbutyrate and benzoate were used in the MIX arm. A likely reason for this observation was the lack of linearity in the pharmacokinetics of the drugs. Under the assumption of first-order kinetics, doubling the dose of the drugs should result in a doubling of the Cmax and AUC; however, phenylbutyrate, PAA, and benzoate Cmax and AUC were significantly greater than expected when phenylbutyrate and benzoate were given as sole treatments as compared with half of these doses in the MIX arm. Moreover, as phenylbutyrate and benzoate conjugate different amino acids, the greater efficacy of conjugation with the MIX treatment may be due to the availability of substrate amino acids. An important finding from this study is that combination therapy using benzoate and phenylbutyrate could be as effective as a higher dose of phenylbutyrate. Due to its low cost, the inclusion of benzoate in the MIX arm virtually halved the cost per unit of nitrogen conjugated and excreted without reducing the efficacy of the treatment when compared with the NaPB arm.
The influx of dietary amino acids peaks approximately 3–4 h after a meal, which agrees with our observation using the 15N-labeled test meal.34,35 Because the drugs were provided with the test meal, the greater efficacy of phenylbutyrate may also be due, at least in part, to a closer match between its pharmacokinetics and the kinetics of protein and amino acid digestion, absorption, and metabolism. However, we could not detect differences in the conjugation and excretion of 15N between the drugs or among the treatments.
There were no treatment differences in urea production among the three treatment arms and urea production in this study was comparable to our previous studies in control subjects consuming a diet that provided 0.6 g protein•kg−1•d−1 and receiving phenylbutyrate.11 Likewise, no differences among the treatments were found for urea nitrogen, 15N urea nitrogen, and total nitrogen urinary excretion.
Because benzoate is widely present in foods as a preservative, it was not surprising to find HA in the urine of subjects not receiving benzoate. However, PAGN was also present in the urine of subjects not receiving phenylbutyrate. It is likely that endogenous PAA, generated by a minor pathway of phenylalanine disposal, was responsible for the appearance of this metabolite in urine.36 Regardless, basal levels of these two metabolites need to be considered when determining the efficiency of drug conjugation in future studies.
A limitation of this study is that it was conducted in healthy subjects. A major goal in the management of UCDs is the control of ammonemia and thus the effect of these drugs on plasma ammonia concentration is central to their therapeutic function.37 Due to the fact that ammonemia is well controlled in healthy subjects, this endpoint was not assessed. Previous studies on phenylbutyrate metabolism were conducted in fasted and drug-naïve individuals or in metabolically adapted subjects who were fed small, frequent meals.11,38,39 A strength of the present study is that the drugs were studied after a 3-day adaptation period and in conjunction with a meal, which better represents the clinical scenario in the management of individuals with UCDs. An additional strength of the study was the use of 15N spirulina to determine the conjugation and excretion of dietary nitrogen, and thus determine for the first time the fate of exogenous nitrogen when alternative pathways for nitrogen disposal are elicited.
In summary, on a molar basis, phenylbutyrate was more efficacious than benzoate at conjugating and disposing of nitrogen. The inclusion of both drugs resulted in a reduction of treatment cost without compromising the amount of nitrogen conjugated. The differences found in the pharmacokinetics between the two drugs may be utilized to devise cost-effective management strategies that maximize the efficacy of drug conjugation and at the same time increase the cost-effectiveness of the therapy.
Change history
06 May 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41436-021-01099-9
References
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits ED. Neurologic outcome in children with inborn errors of urea synthesis. Outcome of urea-cycle enzymopathies. N Engl J Med 1984;310:1500–155.
Batshaw ML, MacArthur RB, Tuchman M. Alternative pathway therapy for urea cycle disorders: twenty years later [see discussion]. J Pediatr 2001;138:S46–S54.
Ah Mew N, Simpson HL, Gropman AL et al. Urea cycle disorders overview. In: Pagon RA, Adam MP, Ardinger HH et al (eds.) GeneReviews. University of Washington: Seattle, WA, 1993.
Mitch WE, Brusilow S. Benzoate-induced changes in glycine and urea metabolism in patients with chronic renal failure. J Pharmacol Exp Ther 1982;222:572–575.
Simell O, Sipila I, Rajantie J, Valle DL, Brusilow SW. Waste nitrogen excretion via amino acid acylation: benzoate and phenylacetate in lysinuric protein intolerance. Pediatr Res 1986;20:1117–1121.
Lee B, Rhead W, Diaz GA et al. Phase 2 comparison of a novel ammonia scavenging agent with sodium phenylbutyrate in patients with urea cycle disorders: safety, pharmacokinetics and ammonia control. Mol Genet Metab 2010;100:221–228.
James MO, Smith RL, Williams RT, Reidenberg M. The conjugation of phenylacetic acid in man, sub-human primates and some non-primate species. Proc R Soc Lond B Biol Sci 1972;182:25–35.
Jones AR. Some observations on the urinary excretion of glycine conjugates by laboratory animals. Xenobiotica 1982;12:387–395.
Cederbaum S, Lemons C, Batshaw ML. Alternative pathway or diversion therapy for urea cycle disorders now and in the future. Mol Genet Metab 2010;100:219–220.
Haberle J, Boddaert N, Berlina A et al. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis 2012;7:32.
Marini JC, Lanpher BC, Scaglia F et al. Phenylbutyrate improves nitrogen disposal via an alternative pathway without eliciting an increase in protein breakdown and catabolism in control and ornithine transcarbamylase-deficient patients. Am J Clin Nutr 2011;93:1248–1254.
Becker EW. Micro-algae as a source of protein. Biotechnol Adv 2007;25:207–210.
Sarkissian CN, Scriver CR, Mamer OA. Measurement of phenyllactate, phenylacetate, and phenylpyruvate by negative ion chemical ionization-gas chromatography/mass spectrometry in brain of mouse genetic models of phenylketonuria and non-phenylketonuria hyperphenylalaninemia. Anal Biochem 2000;280:242–249..
Beylot M, David F, Khalfallah NS et al. Determination of (13C) urea enrichment by gas chromatography/mass spectrometry and gas chromatography/isotope ratio mass spectrometry. Biol Mass Spectrom 1994;23:510–513.
Marini JC. Quantitative analysis of 15N-labeled positional isomers of glutamine and citrulline via electrospray ionization tandem mass spectrometry of their dansyl derivatives. Rapid Commun Mass Spectrom 2011;25:1291–1296.
Kirk PL. Kjeldahl method for total nitrogen. Anal Chem 1950;22:354–358.
Urso R, Blardi P, Giorgi G. A short introduction to pharmacokinetics. Eur Rev Med Pharmacol Sci 2002;6:33–44.
Matthews DE, Downey RS. Measurement of urea kinetics in humans: a validation of stable isotope tracer methods. Am J Physiol 1984;246:E519–E527.
Marini JC, Lee B, Garlick PJ. In vivo urea kinetic studies in conscious mice. J Nutr 2006;136:202–206.
Mackenzie R, Dixon AK. Measuring the effects of imaging: an evaluative framework. Clin Radiol 1995;50:513–518.
Palmer S, Torgerson DJ. Economic notes: definitions of efficiency. BMJ 1999;318:1136.
Batshaw ML, Brusilow S, Waber L et al. Treatment of inborn errors of urea synthesis: activation of alternative pathways of waste nitrogen synthesis and excretion. N Engl J Med 1982;306:1387–1392.
Brusilow S, Tinker J, Batshaw ML. Amino acid acylation: a mechanism of nitrogen excretion in inborn errors of urea synthesis. Science 1980;207:659–661.
Brusilow SW, Valle DL, Batshaw ML. New pathways of nitrogen excretion in inborn errors of urea synthesis. Lancet 1979;2:452–454.
Kibleur Y, Dobbelaere D, Barth M, Brassier A, Guffon N. Results from a Nationwide Cohort Temporary Utilization Authorization (ATU) survey of patients in France treated with Pheburane® (sodium phenylbutyrate) taste-masked granules. Paediatr Drugs 2014;16:407–415.
Koren G, Rieder MJ, Amitai Y. Averting the foul taste of pediatric medicines improves adherence and can be lifesaving: Pheburane® (sodium phenylbutyrate). Patient Prefer Adherence 2016;10:2141–2144.
Enns GM. Nitrogen sparing therapy revisited 2009. Mol Genet Metab 2010;100(suppl 1):S65–71.
Shchelochkov OA, Dickinson K, Scharschmidt BF, Lee B, Marino M, Le Monds C. Barriers to drug adherence in the treatment of urea cycle disorders: assessment of patient, caregiver and provider perspectives. Mol Genet Metab Rep 2016;8:43–47.
Iannitti T, Palmieri B. Clinical and experimental applications of sodium phenylbutyrate. Drugs R D 2011;11:227–249.
Kolb PS, Ayaub EA, Zhou W, Yum V, Dickhout JG, Ask K. The therapeutic effects of 4-phenylbutyric acid in maintaining proteostasis. Int J Biochem Cell Biol 2015;61:45–52.
Kusaczuk M, Bartoszewicz M, Cechowska-Pasko M. Phenylbutyric acid: simple structure—multiple effects. Curr Pharm Des 2015;21:2147–2166.
Burrage LC, Jain M, Gandolfo L et al. Sodium phenylbutyrate decreases plasma branched-chain amino acids in patients with urea cycle disorders. Mol Genet Metab 2014;113:131–135.
Kasumov T, Brunengraber LL, Comte B et al. New secondary metabolites of phenylbutyrate in humans and rats. Drug Metab Dispos 2004;32:10–19.
Gaudichon C, Mahe S, Benamouzig R et al. Net postprandial utilization of [15N]-labeled milk protein nitrogen is influenced by diet composition in humans. J Nutr 1999;129:890–895.
Bos C, Metges CC, Gaudichon C et al. Postprandial kinetics of dietary amino acids are the main determinant of their metabolism after soy or milk protein ingestion in humans. J Nutr 2003;133:1308–1315.
Stein WH, Paladini AC, Hirs CHW, Moore S. Phenylacetylglutamine as a constituent of normal human urine. J Am Chem Soc 1954;76:2848–2849.
Lee B, Diaz GA, Rhead W et al. Blood ammonia and glutamine as predictors of hyperammonemic crises in patients with urea cycle disorder. Genet Med 2015;17:561–568.
Darmaun D, Welch S, Rinia A et al. Phenylbutyrate-induced glutamine depletion in humans: effect on leucine metabolism. Am J Physiol 1998;274:E801–E807.
Comte B, Kasumov T, Pierce BA et al. Identification of phenylbutyrylglutamine, a new metabolite of phenylbutyrate metabolism in humans. J Mass Spectrom 2002;37:581–590.
Acknowledgments
This study was supported by federal funds from the US Department of Agriculture–Agricultural Research Service under cooperative agreement 58-3092-5-001, the National Institute of Child Health and Human Development (R03 HD078447), and the Urea Cycle Disorders Consortium (U54HD061221). The Urea Cycle Disorders Consortium is a part of the Rare Disease Clinical Research Network, an initiative of the Office of Rare Disease Research, National Center for Advancing Translational Sciences. This consortium is funded through collaboration between the National Center for Advancing Translational Sciences and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. The project described was also supported by Clinical Translational Core of the Baylor College of Medicine IDDRC grant 1 U54 HD083092 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Agriculture, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, or the National Institutes of Health. S.C.S.N. was supported by a Clinical Scientist Development Award from the Doris Duke Charitable Foundation (grant 2013095). A.T. was supported by the T32 GM07526-40 Medical Genetics Research Fellowship Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Nagamani, S., Agarwal, U., Tam, A. et al. A randomized trial to study the comparative efficacy of phenylbutyrate and benzoate on nitrogen excretion and ureagenesis in healthy volunteers. Genet Med 20, 708–716 (2018). https://doi.org/10.1038/gim.2017.167
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.167