Abstract
Purpose:
Medical foods for methylmalonic acidemias (MMAs) and propionic acidemias contain minimal valine, isoleucine, methionine, and threonine but have been formulated with increased leucine. We aimed to assess the effects of imbalanced branched-chain amino acid intake on metabolic and growth parameters in a cohort of patients with MMA ascertained via a natural history study.
Methods:
Cross-sectional anthropometric and body-composition measurements were correlated with diet content and disease-related biomarkers in 61 patients with isolated MMA (46 mut, 9 cblA, and 6 cblB).
Results:
Patients with MMA tolerated close to the recommended daily allowance (RDA) of complete protein (mut0: 99.45 ± 32.05% RDA). However, 85% received medical foods, in which the protein equivalent often exceeded complete protein intake (35%). Medical food consumption resulted in low plasma valine and isoleucine concentrations, prompting paradoxical supplementation with these propiogenic amino acids. Weight- and height-for-age z-scores correlated negatively with the leucine-to-valine intake ratio (r = −0.453; P = 0.014; R2 = 0.209 and r = −0.341; P = 0.05; R2 = 0.123, respectively).
Conclusion:
Increased leucine intake in patients with MMA resulted in iatrogenic amino acid deficiencies and was associated with adverse growth outcomes. Medical foods for propionate oxidation disorders need to be redesigned and studied prospectively to ensure efficacy and safety.
Genet Med 18 4, 386–395.
Similar content being viewed by others
Introduction
Medical foods are specially formulated products intended to provide safe alternatives to a regular diet in patients with inborn errors of metabolism.1 These products are designed to abrogate the accumulation of toxic metabolites by limiting the amounts of precursors metabolized through a disease-specific enzymatic block. When the underlying defect involves the metabolism of essential nutrients, such as branched-chain amino acids (BCAAs), however, harmful deficiencies can arise if medical foods are used as a primary dietary source. Despite the inherent risk of inducing iatrogenic side effects, such products are currently classified as “foods for special dietary use” and therefore excluded from the regulatory requirements that apply to drugs ((37 FR 18229–30, 1972 and 21 U.S.C.360ee (b) (3)). It is recognized that except for phenylketonuria, for which medical foods have proven critical in improving disease outcomes, studies of the composition and efficacy of other special formulas remain sparse,2,3 yet their implementation has emerged as a cornerstone of therapy for many inborn errors of metabolism detected through newborn screening, including the hereditary isolated methylmalonic acidemias (MMAs).1,4,5
This group of inborn errors of metabolism results from deficiency of the methylmalonyl-coenzyme A (CoA) mutase (MUT) enzyme (mut0 and mut−, caused by complete or partial MUT deficiency) or related disorders (cblA, cblB, cblD variant 2) that affect the synthesis and transport of the cofactor of the MUT enzyme, 5′-deoxyadenosyl-cobalamin.6 MUT deficiency leads to impaired metabolism of the BCAAs valine (Val) and isoleucine (Ile), as well as methionine and threonine, odd-chain fatty acids, and cholesterol, all of which depend on MUT activity to isomerize succinyl-CoA at the terminal step of propionyl-CoA metabolism into the Krebs cycle.6 The management of this group of disorders remains particularly challenging and controversial because, despite early diagnosis by newborn screening and strict adherence to a protein-restricted diet, patients still experience high mortality and morbidity, including recurrent metabolic ketoacidosis and hyperammonemia, growth failure, chronic kidney disease, pancreatitis, and neurologic complications.6,7,8,9,10,11,12
The management of MMA includes restriction of dietary protein, which is challenging because sufficient essential amino acid (including Val and Ile) intake is needed for optimal growth and must be balanced against the production of “toxic” metabolites derived mainly from propiogenic amino acid oxidation.1,4 The use of specialized amino acid formulations containing minimal to no Val, Ile, methionine, and threonine in the treatment for MMA has become widely implemented,13,14 despite conflicting results about their efficacy over the past 30 years.11,15,16 Early studies by Nyhan et al.17 conducted with a carefully characterized patient convincingly demonstrated that protein restriction significantly improved somatic development, head growth, and intellectual outcome, but the supplementation with nonoffending amino acids offered no additional benefit. A subsequent study showed slightly improved nitrogen retention and plasma protein indexes when patients were administered medical foods, but no improvement in growth.18 The multicenter trial that provided the basis for the current practice guidelines1,5 used a 6-month nonrandomized, non-placebo-controlled study of an amino acid–modified medical food (Propimex-1; Ross Products Division, Abbott Laboratories, Columbus, OH). The study enrolled 16 infants (3 with MMA) and recorded a nonsignificant improvement in growth parameters, primarily body weight, in 7/16 (43%) of the patients.15 No genotypes or enzyme activity data were provided, and the wide range of amino acid intakes and plasma values were not correlated with the growth outcomes.
The lack of strong supporting evidence for a specific medical nutrition therapy and the continued poor growth outcomes for patients with MMA reported in multiple studies11,13 prompted a critical reappraisal of medical food use in the management of MMA. In this single-center natural history study, dietary parameters along with detailed phenotyping data were directly assessed in a large cohort of patients with isolated MMA. We demonstrate that a skewed BCAA intake resulting from generous consumption of medical foods was associated with disturbed plasma amino acid ratios and suboptimal growth and body habitus, likely because of dynamic BCAA metabolic rechanneling induced by the high leucine (Leu) content in the medical foods.19 Although a cause-and-effect relationship between medical foods and growth outcomes cannot be established without a randomized controlled or cross-over study, our study raises concerns about the liberal use of medical foods in MMA and related disorders of propionate oxidation, which has implications not only for the current management of MMA but also a large number of inborn errors of metabolism.
Materials and Methods
Study population
Patient studies were approved by the National Human Genome Research Institute Institutional Review Board and performed in compliance with the Declaration of Helsinki. The trial is registered at ClinicalTrials.gov under identifier NCT00078078. Subjects were enrolled between 2004 and 2014 from regional centers across the United States; a small number of international patients (United Kingdom, Belgium, Argentina, Canada, Taiwan, and China) were also assessed. Long-term medical care and dietary management were provided by regional metabolic centers. Study participants were evaluated at a steady state and were without acute clinical symptoms or laboratory markers of metabolic instability.
The diagnosis of MMA in a total of 61 patients was made using cellular enzymology (laboratory of David S. Rosenblatt, Division of Medical Genetics, McGill University, Canada) and/or molecular genetic analysis (GeneDx; Gaithersburg, MD).6 Ten patients were evaluated following isolated or combined organ transplantation: two with isolated liver, three with kidney, and five with combined liver and kidney transplantation. Data from patients receiving transplantation were used for the analysis of the dietary effects on plasma amino acid concentrations but were excluded from long-term outcome analyses because of the liberalization of protein intake in several transplanted patients.20 Five mut0 patients were not able to provide detailed diet data and were not included in the individual amino acid intake calculations, but they contributed to the dietary data with their daily natural and deficient protein and caloric intake prescription information. Thirty-four of 61 patients (55%) with isolated MMA and 30 of 39 (76%) with mut0 had a gastrostomy tube and received part or all their daily nutrition through bolus or continuous feeds. This allowed for accurate calculations of food intake in the majority of our patient population.
Laboratory studies
Routine laboratory investigations included complete blood count, serum electrolytes, protein, albumin and prealbumin concentrations, liver and pancreatic enzymes, thyroid-function tests, lipid panels, free and total carnitine and acyl/free carnitine ratios, and insulin-like growth factor-1, as well as a battery of research measurements. Metabolites (plasma and urine methylmalonic acid, plasma amino acids) were measured using liquid chromatography–tandem mass spectrometry.
Samples were obtained in the fasting state or 2–4 h after a meal; a smaller number of patients had blood drawn in both states. The National Institutes of Health Biomedical Translational Research Information System was used to retrieve patient clinical research data.
Dietary regimens and daily amino acid intake calculations
Dietary analysis was performed using formula recipes, a 3-day food record collected before the patients’ admission to the National Institutes of Health, and a detailed dietary history obtained by a research dietitian during their inpatient evaluation. Dietary analyses and calculations were performed using Nutrition Data System for Research software versions 2007–2012, developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN.21 Formula composition information was obtained from the respective manufacturers. Protein intake was recorded as complete protein from natural protein sources and incomplete/deficient protein-equivalent intake (grams/kilograms/day) in the form of specialized MMA formulas, such as Propimex1/2, OA1/2, XMTVI Analog, Maxamaid or Maxamum, and MMA/PA Express (Supplementary Table S2 online). Recommended daily allowance (RDA) for protein and amino acids were based on the National Research Council’s Dietary Reference Intakes for protein and amino acids (2005).22
Anthropometry and body-composition analysis
Anthropometric measurements were expressed as age- and gender-specific z-scores using the epidemiological software package Epi Info (version 3.5.1) based on the Centers for Disease Control and Prevention (Atlanta, GA) 2002 reference database. Whole-body composition in grams of fat or fat mass, as well as fat-free (or lean) body mass and bone density, were measured using dual-energy X-ray absorptiometry (Hologic Delphi A; Hologic, Bedford, MA). Values were compared with the mean and SD of reference child and adolescent models of body composition, matched for age, gender, and ethnicity.
Statistical analysis
The results are presented as means ± SD. Significance was set at P < 0.05. Statistical manipulations were performed using SPSS software version 21.0 (IBM, Chicago, IL) or GraphPad Prism software version 6.0 (GraphPad Software, San Diego, CA). An independent Student t-test was used to compare values between patients, who had or had not been receiving medical foods, between patients with incomplete amino acid equivalent–to–complete protein intake ratio more and less than 1, and between males and females. One-way analysis of variance, with Bonferroni correction for multiple comparisons, was used for comparisons among different MMA subtypes (mut, cblA, and cblB). Pearson correlation coefficient and linear or multiple logistic regression analyses were used to evaluate correlations between independent variables. Independent variables used in a multiple-regression equation included MMA subtype, gender, height-for-age z-score, serum creatinine, Leu-to-Val intake ratio, insulin-like growth factor-1, and other serum biomarkers (prealbumin, hemoglobin, white cell and platelet count, protein, albumin, estimated glomerular filtration rate).
Results
Patient cohort and anthropometric characteristics
Sixty-one patients with isolated MMA (46 mut, 9 cblA, and 6 cblB; 36 males, 25 females; age range: 2.5–35 years, mean age ± SD: 13.3 ± 9.1 years) were studied. In the mut cohort, 31/46 patients (67%) presented during the newborn period with hyperammonemia, and 26 individuals (56%) harbored at least one nonsense or frameshift mutation (38/86 alleles), of whom 12 (26%) were compound heterozygotes or homozygotes for these classes of alleles (Supplementary Table S1 online).
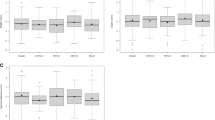
Height, weight, and body mass index for age for patients ≤20 years old are presented as z-scores (mean ± SD) per MMA subtype in Figure 1a and on gender specific growth charts in Supplementary Figure S1 online to allow comparisons with a cohort of 51 patients with MMA from Paris, France.11 For the nontransplanted mut0 patients (n = 28), the mean height z-score was −2.0725 ± 1.71, the weight z-score was −0.817 ± 1.46, and the body mass index z-score was 0.726 ± 0.67, whereas the mean head circumference z-score was −1.61 ± 1.75 (n = 21; Figure 1b ). The clinically less severe mut− and B12-responsive cblA patients had values closer to normal, whereas cblB patients’ growth outcomes were similar to those of the mut0 patients. No significant differences in growth outcomes were observed between males or females, or between patients with the mut0 subtype who presented in the newborn period with hyperammonemia (n = 18) versus those without (n = 7) or those diagnosed by newborn screening (n = 3) (P = 0.275, one-way analysis of variance). A trend for a lower occipitofrontal circumference z-score was observed in the young subgroup (2- to 9-year-old patients) with hyperammonemia as newborns (P = 0.088).
Growth and body composition parameters of MMA patient cohort. (a) Height-, weight- and body mass index (BMI)-for-age z-scores for patients 20 years and younger (n = 28 mut0, 3 mut−, 5 cblA, 2 cblB) are depicted in a box plot. The box represents the middle 50% of all cases per variable, whereas the remaining 50% is contained between the box and whiskers on each side. The single line inside the box represents the median of the entire data set. The location of this line suggests the skewness in the distribution when noticeably shifted away from the center, as is the case for the BMI-for-age z-score in the mut0 subgroup. As evidenced by the z-scores, mut0 patients were short and overweight or obese.(b) Head circumference z-score was lower in the mut0 group (mean ± SD: −1.66 ± 1.63; n = 22). (c) Percentage fat and fat-free (lean) mass are depicted by methylmalonic acidemia subtype for nontransplanted patients in a box plot (n = 28 mut0, 3 mut−, 7 cblA, and 5 cblB). Percentage fat mass was significantly higher in the mut0 subtype compared with the milder cblA subtype (P = 0.01, one-way analysis of variance between groups; Bonferroni post-hoc correction between mut0 and cblA, *P = 0.042 for percentage fat and *P = 0.037 for percentage lean).
Whole-body composition was measured by dual-energy X-ray absorptiometry imaging in 39 mut, 7 cblA, and 5 cblB patients. mut0 patients had a significantly higher percentage fat mass (36.7 ± 9.3%), and thus a lower percentage fat-free or lean mass (61.09 ± 9.25%), compared with those with cblA (24.9 ± 10.94 and 72.7 ± 10.6, respectively; P = 0.031) but not with cblB patients (P = 0.08) ( Figure 1c ). Moreover, mean percentage fat mass in patients aged <18 years were higher compared with the highest values observed in gender- and ethnicity-matched control reference data (27.6 ± 6.1% (n = 46) for females (P = 0.0001) and 22.2 ± 10.3 (n = 51) for males (P = 0.004).4
Protein needs and medical foods utilization
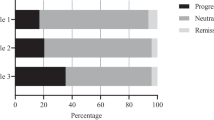
We aimed to investigate whether low protein intake or unbalanced BCAA composition of MMA medical foods could contribute to the poor growth outcomes and low muscle mass observed in our cohort of patients with MMA. Complete and incomplete protein intakes (in grams/kilogram/day) are presented for each of the patients per MMA subtype and age ( Figure 2a ). To our surprise, the mean daily complete protein intake ( Table 1 ) was close to the RDA for protein for healthy children: The mean for all the mut patients was 102.6 ± 30.3% RDA,22 while similar intakes were observed even in the fragile mut0 patients, 99.45 ± 32.05% for all nontransplanted patients ( Figure 2b ), especially in the younger age groups. Mean complete protein percentage of RDA was 105.4 ± 25.7 for the 2- to 9-year-old and 99.8 ± 47.5 for the 10- to 18-year-old mut0 patients. Values are presented per patients’ actual weight (kilograms) and hence would seem even more generous if expressed per ideal weight or adjusted for the decreased lean mass of the patients.
Dietary protein and branched-chain amino acid intake. (a) Daily protein intake (grams/kilograms/day) is provided per patient sorted by age and methylmalonic acidemia (MMA) subtype (mut, cblA, and cblB). A number of mut patients (n = 7) required additional valine and/or isoleucine supplementation because of persistently low plasma amino acid concentrations during their follow-up monitoring by their home metabolic clinics (labeled with a star). Four of these patients had a complete protein intake at or above the recommended dietary allowance (RDA) for age (solid stars), whereas three were on a low complete protein diet (white stars). Age-adjusted RDA is depicted as a dotted line. (b) The mean daily complete protein intake is depicted as percentage RDA (%RDA) for protein for healthy children in a box plot. The box represents the middle 50% of all cases per variable, whereas the remaining 50% is contained between the box and whiskers on each side. The single line inside the box represents the median of the entire data set. Patients with the mut0 subtype consumed 99.45 ± 32.05% RDA complete protein (mean ± SD), mut− 119.0 ± 10.00%, cblA 139.6 ± 66.37, and cblB 68.83 ± 18.19% (n = 31, 6, 8, and 6, respectively). Transplant recipients were excluded. Although adjusting for the high versus low biological value of dietary protein source might decrease slightly the aforementioned percentage, this analysis was not feasible based on existing dietary records. On the other hand, calculations are provided for the actual and not ideal weight of the patients, suggesting that protein intake would be more generous if expressed per gram of their decreased lean mass. (c) The ratios of incomplete to complete protein intakes in the subset of patients consuming medical foods are provided per MMA subtype in a box plot. Patients with mut0 MMA had a ratio of 1.16 ± 0.13 (mean ± SD), mut− 0.68 ± 0.20, cblA 0.63 ± 0.13, and cblB 1.53 ± 0.24 (n = 24, 4, 3, and 4, respectively). 13/37, or 35.0%, of mut patients receiving medical foods exceeded the current treatment guidelines of 1:1 ratio of complete to deficient protein intake. (d) Daily intake of leucine, valine, and isoleucine (milligrams/kilogram/day by age group) for patients with the mut subtype of MMA is provided in a box plot. Leucine intake was 222.0 ± 24.9 in the 2- to 9-year-olds, 173.33 ± 55.6 in the 10- to 18-year-olds, and 60.0 ± 20.8 in the >18-year-olds. The younger patients consumed amounts four to five times higher than the recommended dietary reference intake based on the 2007 Food and Agriculture Organization/World Health Organization guidelines (dietary reference intake of 44–50 mg/kg/day, dotted line). (e) High daily consumption was recorded even for the two propiogenic amino acids, valine and isoleucine, in the younger age groups.
Sixty-five percent of the patients and 85% of those with mut MMA were consuming various amounts of special MMA formulas in addition to a natural protein intake approaching the RDA. The protein content of the special MMA formulas often exceeded the amount of natural protein intake (in 13/37, or 35.0%, of the mut patients). This is presented as a ratio of incomplete to complete protein intake ( Figure 2c ). A number of mut patients (n = 7) were prescribed additional Val (for valine) and/or Ile by their home metabolic clinics because of persistently low plasma concentrations (labeled with a star in Figure 2a ). Interestingly, a number of the patients requiring Val and/or Ile supplementation had a natural protein daily intake at or above RDA and a total protein intake between 2 and 2.5 g/kg/day (n = 4; filled stars in Figure 2a ).
Individual BCAA intake and plasma concentrations
To better understand the individual amino acid requirements of patients with MMA and analyze the effects of their daily intakes on various biochemical parameters, we estimated daily intakes for each of the BCAAs—Leu, Val, and Ile—from dietary records. We show in Table 2 the range of recommended individual amino acid intakes by age from reference nutrition books that are used to guide dietary management in MMA1,4 and the ranges we observed in our MMA cohort. The mean intake of Leu, Val, and Ile (in milligrams/kilogram/day) by age group is shown in Figure 2d , e .
Leu content is higher than Val and Ile content in all food sources.19,22 In human breast milk relative ratios of Leu to Val to Ile are about 2.0:1.2:1(Supplementary Table S2 online). Hence, a normal BCAA intake ratio was observed in our patients who did not consume medical foods ( Figure 3a ). These patients were mostly international with limited access to medical foods or from US centers that did not prescribe medical foods. Medical foods for MMA and propionic acidemia contain minimal to no Val or Ile but have an increased amount of Leu (Supplementary Table S2 online). Therefore, patients consuming medical foods had a significantly higher intake ratio for Leu/Val or Leu/Ile (P < 0.001 for both) compared with patients using no medical foods ( Figure 3a ). As expected, this difference was also translated to their measured plasma amino acid ratios, obtained 2–4 h after last meal/feeding ( Figure 3b ). Moreover, these abnormal plasma BCAA ratios were more pronounced the closer to the feedings a blood sample was taken, as illustrated with a case example (Supplementary Figure S2a online), whereas they returned to normal immediately following the discontinuation of medical foods (Supplementary Figure S2b,c online).
Correlation of medical food use with plasma amino acid concentrations and growth parameters. (a) Ratios of leucine (Leu) to valine (Val) or isoleucine (Ile) dietary intake are compared between patients on and off medical foods. Normal branched-chain amino acid ratios with very narrow distribution were observed in patients who consumed no medical foods (Leu-to-Val mean intake ratio was 1.54 ± 0.07, whereas the Leu-to-Ile intake ratio was 1.73 ± 0.10; n = 16; bars represent mean with 95% confidence interval), in contrast to significantly higher ratios recorded in patients taking medical foods (Leu-to-Val ratio of 3.82 ± 1.82 and Leu-to-Ile ratio of 3.99 ± 1.65; n = 34; ****P < 0.001 for both Leu/Val and Leu/Ile (independent t-test)) as a result of the high Leu content in these formulations. (b) Higher Leu over Val and Ile dietary intake ratios translated in reversed or higher ratios, respectively, in their relative plasma amino acid concentrations. Patients receiving medical foods had a reversed plasma Leu-to-Val ratio of 1.25 ± 0.74 and a close to twofold-increased ratio of Leu to Ile of 3.58 ± 2.4, compared with patients receiving no medical foods (***P = 0.003 and ****P < 0.001 for Leu/Val and Leu/Ile). (c) Amount of deficient protein intake (grams/kilograms/day) was inversely related to the plasma Val (solid circles) and Ile (clear circles) concentrations. Although a range of plasma concentrations were observed in patients without medical food intake—depicted on the left of the graph—the lowest plasma Val and Ile values were observed in patients consuming the highest amounts of medical food. (d) Dietary Leu/Val intake showed a negative correlation to height-for-age (solid squares) and weight-for-age z-scores (white squares) in the subgroup of mut0 patients with MMA, supporting that increased consumption of deficient protein administered at the expense of complete protein may adversely affect growth parameters. Patients of comparable severity (age at onset, frequency and severity of metabolic crises/hospitalizations, renal disease, among other disease complications) are present at each end of the regression curve.
The temporal association of depressed plasma Ile and Val concentrations in the setting of medical food ingestion suggested that the high Leu content of medical foods was distorting the BCAA ratios. A negative, statistically significant correlation was observed between the amount of incomplete daily protein intake (grams/kilograms/day) and plasma Val and Ile concentrations, taken 2–4 h after feedings, across all patients (Val: r = −0.569; P < 0.001; R2 = 0.324; Ile: r = −0.469; P = 0.001; R2 = 0.22) ( Figure 3c ) and for mut0 patients separately (Val: r = −0.538; P = 0.002; R2 = 0.289; Ile: r = −0.417; P = 0.022; R2 = 0.174). Importantly, the correlation persisted in the subset of patients consuming >100% RDA complete protein intake (Val: r = −0.602; P = 0.001; R2 = 0.363; Ile: r = −0.413; P = 0.032; R2 = 0.171). A similar correlation to incomplete protein intake was observed for methionine and threonine plasma concentrations (in mut0 patients r = −0.523; P = 0.003; R2 = 0.273 for methionine and r = −0.458; P = 0.011; R2 = 0.210 for threonine; data not shown).
Correlation to growth and other disease-related outcomes
Recognizing that dietary prescriptions can change significantly in a patient’s life span and that data on patient-years on a higher than recommended medical foods/natural protein intake (leucine-to-valine, 1:1) ratio would be the preferred variable for the associations presented, we attempted to evaluate whether patients’ protein intakes at the time of our study were correlated to their growth parameters. We looked for such associations in the subgroup of patients with the genotype-confirmed mut0 MMA subtype before any transplantation procedure.
A negative correlation was observed between the ratio of dietary leucine/valine intake and height, weight, and bone mineral density z-scores in our mut0 patients (height-for-age z-score: r = −0.341; P = 0.05; R2 = 0.123 (n = 23); weight-for-age z-scores: r = −0.453; P = 0.014; R2 = 0.209 ( Figure 3d ); and BMD: r = −0.406; P = 0.049; R2 = 0.165 (data not shown)). However, when the absolute amount of deficient protein/kilograms/day was correlated with the growth indexes, these correlations were not statistically significant. In aggregate, our data suggest that diets containing a high content of Val- and Ile-deficient protein provided by medical foods, especially in the context of reduced natural protein intake, are associated with poor growth parameters. Stepwise regression modeling revealed that the combination of serum creatinine (β coefficient = −0.66; P = 0.003), Leu-to-Val intake ratio (β= −0.482; P = 0.008), and serum insulin-like growth factor-1 values (β = 0.471; P = 0.025) best predicted height z-score, with a model R2 of 0.478. The R2 of the regression model improved significantly from 0.123 (only dietary Leu/Val intake included) to 0.296 (creatinine added to the model) and 0.478 (insulin-like growth factor-1 added), showing the effect of incorporating the well-described effects of renal function and growth hormone axis on growth. The significant correlations of renal function with height z-score and plasma MMA values are provided separately in Supplementary Figure S3 online and expand on previous observations in a subset of this patient cohort.12,13,23
Protein intake and biochemical indexes of protein status correlated with lean body mass and platelet counts (Supplementary Figure S3a,d online), whereas indexes of renal function showed a negative correlation with height z-score and, similarly, with prealbumin (transthyretin) concentrations, a lab test used by many clinics for monitoring protein status in patients with MMA and other inborn errors of metabolism (r = −0.659; P = 0.002, R2 = 0.434; Supplementary Figure S3c online), whereas a positive correlation was observed with the plasma MMA values, as shown previously in a subset of this cohort.12,13,23
Discussion
This study presents a critical reappraisal of medical food use in MMA, derived from inpatient measurements performed as part of a dedicated, single-center natural history protocol (ClinicalTrials.gov NCT00078078). Because we enrolled patients from national and international metabolic clinics with varied management approaches to dietary therapy, our study revealed unique insights into the current management of MMA as well as iatrogenic effects of medical food use. Over 10 years we encountered a number of patients with MMA who, despite an apparently adequate natural protein intake, had persistently low plasma BCAA concentrations, prompting their clinics to increase the complete protein or supplement with individual amino acids, that is, Val and/or Ile, to avoid essential amino acid deficiencies13 ( Figure 1a , stars). The supplementation with Val and/or Ile was paradoxical because these are the propiogenic amino acids targeted for dietary minimization because they are the main contributors to the “toxic” metabolite pool.24
Growth outcomes in our MMA cohort were poor (height, weight, and occipital-frontal circumference z-scores for age), and body composition showed significantly increased percentage fat mass ( Figure 1 ). We have previously shown that mut patients with MMA receive nearly two times more calories than their measured resting energy expenditure,13 which predisposes them to obesity. In this study we sought to explore whether severe protein restriction could contribute to the short stature and decreased lean body mass of patients of MMA, as well as the paradoxical requirement for BCAA supplementation observed in a subset of patients.
Surprisingly, the complete protein intake and individual essential BCAA intake consumed by patients in our study were higher than the recommended amounts for other inborn errors, such as phenylketonuria or maple syrup urine disease,1,4,25 where protein restriction is an essential part of management and amounts were higher than the Food and Agriculture Organization/World Health Organization/United Nations University (2007) safe protein intake levels5 proposed in the European guidelines or metabolic textbooks for MMA ( Table 2 ). It has been argued that RDA is inadequate in organic acidemias because (i) most of the dietary protein is plant-derived, which may not contain complementary amino acids or can be less digestible; (ii) complete protein when given as free amino acid formula (e.g., Splash, Neocate, Elecare) should be increased by about 20% to account for altered absorption and oxidation rates; and (iii) patients have frequent catabolic episodes, resulting in the need for catch-up growth.1 However, the argument for increased natural/complete protein is often translated to a higher deficient protein prescription, resulting in a higher than recommended ratio of deficient to natural protein. Many patients in this study indeed consumed significant quantities of medical foods in addition to an apparently sufficient amount of complete protein. Of note, total protein intake reached 2–3 g/kg/day in patients up to 11 years of age, a significant amount of total nitrogen load, especially for a patient cohort with chronic kidney disease and at risk to develop hyperammonemia. It was, therefore, even more perplexing that some patients required Val and Ile supplementation, which prompted us to search for alternative explanations for possible deficiencies and reevaluate the amino acid composition of dietary and medical food–derived protein equivalents.
Compared with formulas composed for the treatment of maple syrup urine disease, which are devoid of all BCAAs, those prepared for disorders of propionate oxidation contain little to no Val, Ile, methionine, and threonine because these amino acids are oxidized to propionyl-CoA and generate methylmalonic acid. Upon analysis, however, it became evident that MMA formulas contain a normal to increased amount of Leu (Supplementary Table S2 online). Hence, they represent the only formulas with an imbalanced BCAA composition and their administration results in a significantly increased and nonphysiologic Leu versus Val and Ile intake, especially when prescribed in significant quantities. Leu intake in our MMA patient cohort was indeed four to five times higher than the daily recommended intake based on the 2007 Food and Agriculture Organization/World Health Organization guidelines (mean: 195.1 mg/kg/day, range: 30–510 mg/kg/day, compared with the daily recommended intake of 44–50 mg/kg/day; Figure 2d ). In some of the patients with MMA, Leu intake reached levels shown to cause hyperammonemia and other side effects when administered to healthy volunteers26 ( Table 2 ). Of note, target amounts for Leu consumption are not considered in the proposed guidelines for the dietary management of MMA.1,4,5
Hence, this study raises the following intriguing question: Can we assume that, just because Leu is not oxidized into MMA, any amount of Leu is completely safe for patients with MMA? From the work of Nyhan et al.27 on the originally reported case of ketotic hyperglycinemia, it was noted that Leu administration resulted in a decrease of Val and Ile plasma concentrations in the patient, as well as in healthy controls. These observations have been further extended in animal models (rats,28,29 chicks,30 and pigs,31 among others) that demonstrate when Leu is ingested, especially by animals receiving a low-protein diet, it causes depletion of Val/α-ketoisovaleric acid and Ile/α-keto-β-methylvaleric concentrations in the plasma and tissue pools, and is associated with marked growth depression that can be overcome with Val or Ile supplementation. Furthermore, in numerous studies performed with human subjects, administration of a Leu load (but not of Val or Ile) by mouth or intravenously results in dramatic decreases in plasma concentrations of Val, Ile, phenylalanine, tyrosine, threonine, and methionine within 1–3 h of administration.19,26,32,33,34 While the mechanism(s) behind the lowering effect of Leu on plasma amino acid concentrations are not fully understood, it has been proposed that the inhibitory role of Leu-derived α-ketoisocaproate on the branched-chain ketoacid dehydrogenase-kinase results in activation of branched-chain ketoacid dehydrogenase and increased BCAA oxidation.19
In addition, Leu displays a multitude of effects that have not been carefully considered in the management of patients with MMA. Leu enhances protein synthesis,35 inhibits muscle protein breakdown,36,37 stimulates insulin secretion,38 and plays a role in central nervous system food intake regulatory circuits and feeding behavior.39 Because Leu is primarily transported via the large neutral amino acid transporter LAT1 at the blood–brain barrier,40 it can compete with other large neutral amino acids for uptake/transport and, subsequently, neurotransmitter biosynthesis, as detailed in studies of maple syrup urine disease,41 phenylketonuria,42 and glutaric acidemia type 1.43 The high Leu-to-Val, -Ile, and -methionine plasma ratios observed in the current study would be predicted to impair the uptake of Val, Ile, and methionine through the blood–brain barrier and result in depletion of these amino acids in the brain, with potentially detrimental consequences, especially during periods of brain growth.
The main caveat of this study is the cross-sectional representation of dietary composition and growth outcomes, which precludes causal claims, especially because dietary prescriptions can change significantly over time. Furthermore, growth failure is a well-recognized complication of MMA and a result of multiple factors, including frequent catabolic events, protein restriction, chronic renal disease, growth or thyroid hormone deficiency, and possibly factors intrinsic to the disease pathophysiology, such as mitochondrial dysfunction. However, our observations highlight a previously unrecognized iatrogenic amino acid deficiency with use of medical foods, a concept reinforced by the fact that removing medical foods from the diet restored BCAA homeostasis in two patients in our cohort (Supplementary Figure S2 online), and raise questions about the current lack of consideration of the effects of Leu supplementation in the dietary management of MMA.
In conclusion, the excessive use of medical foods, especially in the setting of reduced natural protein intake, resulted in iatrogenic amino acid deficiencies and was associated with poor growth outcomes in a large cohort of patients with isolated MMA. The unbalanced intake of Leu carries theoretical risks, especially with respect to brain amino acid uptake and whole-body metabolism, and unexplored long-term sequelae. Medical foods and dietary guidelines for MMA should be revised based on well-controlled and sufficiently powered clinical studies to support their efficacy and safety. The questions raised with this work are relevant to a collectively large number of inborn errors of metabolism detected by newborn screening.
Disclosure
The authors declare no conflict of interest.
References
Acosta, P. Nutrition Management of Patients with Inherited Metabolic Disorders. Jones & Bartlett: Burlington, MA, 2010:476.
Camp KM, Lloyd-Puryear MA, Yao L, et al. Expanding research to provide an evidence base for nutritional interventions for the management of inborn errors of metabolism. Mol Genet Metab 2013;109:319–328.
Camp KM, Lloyd-Puryear MA, Huntington KL. Nutritional treatment for inborn errors of metabolism: indications, regulations, and availability of medical foods and dietary supplements using phenylketonuria as an example. Mol Genet Metab 2012;107:3–9.
Blau N, Hoffmann GF, Leonard J, Clark JTR. Physician’s Guide to the Treatment and Follow-Up of Metabolic Diseases. Springer: Berlin, Germany, 2006.
Baumgartner MR, Hörster F, Dionisi-Vici C, et al. Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis 2014;9:130.
Manoli I, Venditti CP. Methylmalonic acidemia. In: Pagon RA, Adam MP, Ardinger HH, et al. (eds.). GeneReviews. University of Washington: Seattle, WA, 2005.
Matsui SM, Mahoney MJ, Rosenberg LE. The natural history of the inherited methylmalonic acidemias. N Engl J Med 1983;308:857–861.
Rosenberg LE, Lilljeqvist AC, Hsia YE. Methylmalonic aciduria. An inborn error leading to metabolic acidosis, long-chain ketonuria and intermittent hyperglycinemia. N Engl J Med 1968;278:1319–1322.
Hörster F, Baumgartner MR, Viardot C, et al. Long-term outcome in methylmalonic acidurias is influenced by the underlying defect (mut0, mut-, cblA, cblB). Pediatr Res 2007;62:225–230.
Cosson MA, Benoist JF, Touati G, et al. Long-term outcome in methylmalonic aciduria: a series of 30 French patients. Mol Genet Metab 2009;97:172–178.
Touati G, Valayannopoulos V, Mention K, et al. Methylmalonic and propionic acidurias: management without or with a few supplements of specific amino acid mixture. J Inherit Metab Dis 2006;29:288–298.
Manoli I, Sysol JR, Li L, et al. Targeting proximal tubule mitochondrial dysfunction attenuates the renal disease of methylmalonic acidemia. Proc Natl Acad Sci USA 2013;110:13552–13557.
Hauser NS, Manoli I, Graf JC, Sloan J, Venditti CP. Variable dietary management of methylmalonic acidemia: metabolic and energetic correlations. Am J Clin Nutr 2011;93:47–56.
Zwickler T, Lindner M, Aydin HI, et al. Diagnostic work-up and management of patients with isolated methylmalonic acidurias in European metabolic centres. J Inherit Metab Dis 2008;31:361–367.
Yannicelli S, Acosta PB, Velazquez A, et al. Improved growth and nutrition status in children with methylmalonic or propionic acidemia fed an elemental medical food. Mol Genet Metab 2003;80:181–188.
Walter JH, MacDonald A. The use of amino acid supplements in inherited metabolic disease. J Inherit Metab Dis 2006;29:279–280.
Nyhan WL, Fawcett N, Ando T, Rennert OM, Julius RL. Response to dietary therapy in B 12 unresponsive methylmalonic acidemia. Pediatrics 1973;51:539–548.
Ney D, Bay C, Saudubray JM, et al. An evaluation of protein requirements in methylmalonic acidaemia. J Inherit Metab Dis 1985;8:132–142.
Harper AE, Miller RH, Block KP. Branched-chain amino acid metabolism. Annu Rev Nutr 1984;4:409–454.
Reineking BA, Maraglino AC, Ueda K. Nutritional management of methylmalonic and propionic acidemia. Three peritransplant patients. Top Clin Nutr 2009;24:347–358.
Schakel SF. Maintaining a nutrient database in a changing marketplace: keeping pace with changing food products—a research perspective. J Food Compost Anal 2001;14:315–322.
National Research Council. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press: Washington, DC, 2005.
Kruszka PS, Manoli I, Sloan JL, Kopp JB, Venditti CP. Renal growth in isolated methylmalonic acidemia. Genet Med 2013;15:990–996.
Thompson GN, Walter JH, Bresson JL, et al. Sources of propionate in inborn errors of propionate metabolism. Metabolism 1990;39:1133–1137.
Parsons HG, Carter RJ, Unrath M, Snyder FF. Evaluation of branched-chain amino acid intake in children with maple syrup urine disease and methylmalonic aciduria. J Inherit Metab Dis 1990;13:125–136.
Elango R, Chapman K, Rafii M, Ball RO, Pencharz PB. Determination of the tolerable upper intake level of leucine in acute dietary studies in young men. Am J Clin Nutr 2012;96:759–767.
Nyhan WL, Borden M, Childs B. Idiopathic hyperglycinemia: a new disorder of amino acid metabolism. II. The concentrations of other amino acids in the plasma and their modification by the administration of leucine. Pediatrics 1961;27:539–550.
Shinnick FL, Harper AE. Effects of branched-chain amino acid antagonism in the rat on tissue amino acid and keto acid concentrations. J Nutr 1977;107:887–895.
Block KP, Harper AE. Valine metabolism in vivo: effects of high dietary levels of leucine and isoleucine. Metabolism 1984;33:559–566.
Boldizsár HK, Boorman KN, Buttery PJ. The effect of excess leucine on valine catabolism in the chick. Br J Nutr 1973;30:501–510.
Langer S, Scislowski PW, Brown DS, Dewey P, Fuller MF. Interactions among the branched-chain amino acids and their effects on methionine utilization in growing pigs: effects on plasma amino- and keto-acid concentrations and branched-chain keto-acid dehydrogenase activity. Br J Nutr 2000;83:49–58.
Swendseid ME, Villalobos J, Figueroa WS, Drenick EJ. The effects of test doses of leucine, isoleucine or valine on plasma amino acid levels. The unique effect of leucine. Am J Clin Nutr 1965;17:317–321.
Hambraeus L, Bilmazes C, Dippel C, Scrimshaw N, Young VR. Regulatory role of dietary leucine on plasma branched-chain amino acid levels in young men. J Nutr 1976;106:230–240.
Eriksson S, Hagenfeldt L, Wahren J. A comparison of the effects of intravenous infusion of individual branched-chain amino acids on blood amino acid levels in man. Clin Sci (Lond) 1981;60:95–100.
Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell 2012;149:274–293.
Baptista IL, Leal ML, Artioli GG, et al. Leucine attenuates skeletal muscle wasting via inhibition of ubiquitin ligases. Muscle Nerve 2010;41:800–808.
Russell RC, Yuan HX, Guan KL. Autophagy regulation by nutrient signaling. Cell Res 2014;24:42–57.
Sener A, Malaisse WJ. L-leucine and a nonmetabolized analogue activate pancreatic islet glutamate dehydrogenase. Nature 1980;288:187–189.
Cota D, Proulx K, Smith KA, et al. Hypothalamic mTOR signaling regulates food intake. Science 2006;312:927–930.
Manoli I, Venditti C. Branched chain amino acid disorders. In: Lee B, Scaglia F (eds.). Inborn Errors of Metabolism: From Neonatal Screening to Metabolic Pathways. Oxford University Press: New York, 2015. pp. 92–118.
Muelly ER, Moore GJ, Bunce SC, et al. Biochemical correlates of neuropsychiatric illness in maple syrup urine disease. J Clin Invest 2013;123:1809–1820.
Camp KM, Parisi MA, Acosta PB, et al. Phenylketonuria Scientific Review Conference: state of the science and future research needs. Mol Genet Metab 2014;112:87–122.
Sauer SW, Opp S, Hoffmann GF, Koeller DM, Okun JG, Kölker S. Therapeutic modulation of cerebral L-lysine metabolism in a mouse model for glutaric aciduria type I. Brain 2011;134(Pt 1):157–170.
Acknowledgements
The authors thank all the patients and their families for their participation in our natural history protocol and donation of blood/tissues for our studies; referring physicians, nurses, and dietitians for their help with patient’s evaluations; Isa Bernardini and Roxanne Fischer for processing patient samples; the nurses, research dietitians of the National Institutes of Health Clinical Research Center, and clinical fellows of the National Human Genome Research Institute genetics fellowship program for their help with patient care and dedication to clinical research. I.M, J.L.S., and C.P.V were supported by the Intramural Research Program of the National Human Genome Research Institute, Bethesda, MD. J.M. was supported by the National Institutes of Health clinical center. Oleg A. Shchelochkov was supported by National Institutes of Health/National Institute of Child Health and Human Development grant K12 HD027748. The authors also thank Cheryl Stimson, MS, RD (University of Iowa Hospitals and Clinic), for her help with patient care.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figures
(PDF 526 kb)
Supplementary Tables
(DOC 116 kb)
Rights and permissions
About this article
Cite this article
Manoli, I., Myles, J., Sloan, J. et al. A critical reappraisal of dietary practices in methylmalonic acidemia raises concerns about the safety of medical foods. Part 1: isolated methylmalonic acidemias. Genet Med 18, 386–395 (2016). https://doi.org/10.1038/gim.2015.102
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2015.102
Keywords
This article is cited by
-
Review of neuropsychological outcomes in isolated methylmalonic acidemia: recommendations for assessing impact of treatments
Metabolic Brain Disease (2022)
-
Genetic testing is necessary for correct diagnosis and treatment in patients with isolated methylmalonic aciduria: a case report
BMC Pediatrics (2021)
-
Severe anemia in patients with Propionic acidemia is associated with branched-chain amino acid imbalance
Orphanet Journal of Rare Diseases (2021)
-
Autozygosity mapping of methylmalonic acidemia associated genes by short tandem repeat markers facilitates the identification of five novel mutations in an Iranian patient cohort
Metabolic Brain Disease (2018)
-
Role of medical food in MMA
Genetics in Medicine (2016)