Abstract
Purpose:
Advanced maternal age and altered recombination are known risk factors for Down syndrome cases due to maternal nondisjunction of chromosome 21, whereas the impact of other environmental and genetic factors is unclear. The aim of this study was to investigate an association between low maternal socioeconomic status and chromosome 21 nondisjunction.
Methods:
Data from 714 case and 977 control families were used to assess chromosome 21 meiosis I and meiosis II nondisjunction errors in the presence of three low socioeconomic status factors: (i) both parents had not completed high school, (ii) both maternal grandparents had not completed high school, and (iii) an annual household income of <$25,000. We applied logistic regression models and adjusted for covariates, including maternal age and race/ethnicity.
Results:
As compared with mothers of controls (n = 977), mothers with meiosis II chromosome 21 nondisjunction (n = 182) were more likely to have a history of one low socioeconomic status factor (odds ratio = 1.81; 95% confidence interval = 1.07–3.05) and ≥2 low socioeconomic status factors (odds ratio = 2.17; 95% confidence interval = 1.02–4.63). This association was driven primarily by having a low household income (odds ratio = 1.79; 95% confidence interval = 1.14–2.73). The same statistically significant association was not detected among maternal meiosis I errors (odds ratio = 1.31; 95% confidence interval = 0.81–2.10), in spite of having a larger sample size (n = 532).
Conclusion:
We detected a significant association between low maternal socioeconomic status and meiosis II chromosome 21 nondisjunction. Further studies are warranted to explore which aspects of low maternal socioeconomic status, such as environmental exposures or poor nutrition, may account for these results.
Genet Med 15 9, 698–705.
Similar content being viewed by others
Main
Down syndrome (DS) is the most commonly diagnosed genetic cause of intellectual disability, with a prevalence of approximately 1 in 700 live births in the United States.1 DS results primarily from an extra chromosome 21 (trisomy 21), with the vast majority of cases of DS being due to segregation errors occurring in the oocyte (for review, see Sherman et al.2). Furthermore, data from the National Down Syndrome Project (NDSP), a large population-based case–control study,3 are consistent with other population-based studies showing that the majority of maternal nondisjunction errors occur during meiosis I (MI).4,5 On average, the ratio of MI to meiosis II (MII) nondisjunction errors associated with DS is ~3:1, although this proportion varies with the maternal age structure of the study sample.6
Meiosis in females is initiated during fetal development and arrests in prophase of MI around gestation week 20. MI is resumed when an oocyte is recruited for ovulation, some 10–50 years later. MII is initiated after the completion of MI at ovulation and is arrested at metaphase until fertilization. This process leaves an extended time period for exposure to risk factors for nondisjunction. The etiology of meiotic nondisjunction errors that occur during oogenesis is complex; however, two risk factors have been clearly defined: advanced maternal age6,7,8,9,10 and patterns of meiotic recombination.11,12,13,14,15,16 Associated recombination events, which are established and resolved during MI, are altered with respect to the location of recombination break points and the number of events.
In addition to advanced maternal age and recombination patterns, many potential genetic and environmental risk factors are being investigated for chromosome nondisjunction. Only now are the specific biological mechanisms behind the increased risk of nondisjunction with increasing maternal age being elucidated (see Nagaoka et al.17 for review). One potential factor involved in the reduction of oocyte quality over time is the accumulation of toxic elements from the environment that could damage the meiotic machinery.18,19,20 The cellular components of the oocyte and the somatic compartment are exposed to toxic influences that depend on the chronological age of the oocyte, lifestyle, and environment. Along with the intrinsic aging process of the oocyte, diminished oocyte quality could result from damage by reactive oxygen species from metabolism.21 Given the timeline of oogenesis, exposures impacting oocyte quality could occur during the fetal period of the woman or at any point in her lifetime before fertilization.
Torfs and Christianson22 published the results of a population-based case–control study analyzing 997 DS cases and 1,007 controls ascertained as part of a birth surveillance program in selected counties across California. Maternal socioeconomic status (SES) was used as a proxy for environmental exposures to predict the risk of a clinically recognized pregnancy with DS. The SES level of the mother was assessed both during her fetal development (e.g., her father’s occupation at the time of her birth) and during her lifetime before conception (e.g., the mother’s level of education). After adjusting for race/ethnicity, gravidity, and maternal age, results of the study indicated an association of a clinically recognized pregnancy with DS and low maternal SES. Specifically, the association with DS was significantly higher when the mother had less than a high school education (odds ratio (OR) = 1.29; 95% confidence interval (CI) = 1.01–1.65), the maternal grandfather was employed as a laborer or unemployed (OR = 1.35; 95% CI = 1.06–1.71), and the household income was <$20,000 (OR = 1.31; 95% CI = 1.02–1.68). In a follow-up study, the authors determined the type of meiotic error in 150 of the cases analyzed in the previous study and found that the association with these SES risk factors differed by the type of maternal meiotic error. Specifically, mothers of DS cases due to a MII nondisjunction error (n = 29) were more likely to have a history of low SES (OR = 12.20; 95% CI = 2.26–66.02), defined as the presence of at least one low SES risk factor (mother had less than a high school education, father had less than a high school education, father was a laborer or unemployed, maternal grandfather was a laborer or unemployed, or family income was <$20,000) as compared with controls.23 This same effect was not seen among MI cases (n = 103) as compared with controls (OR = 1.25; 95% CI = 0.72–2.22).
In this study, we used the data from the NDSP, a large, diverse population-based case–control study of live births, to further examine the association between maternal history of low SES and having an infant with DS. Of note, we stratified mothers by type of maternal meiotic error. Our study population was drawn from six sites across the United States and included the three major race/ethnic groups in the United States, namely, non-Hispanic African Americans (referred to as “blacks”), non-Hispanic whites (referred to as “whites”), and Hispanics.
Materials and Methods
Study population
The current study assessed 714 DS case and 977 control families recruited for the NDSP based at Emory University in Atlanta, Georgia. The NDSP was a population-based, epidemiological study to recruit families of infants born with DS at six sites across the United States (Arkansas, Iowa, New Jersey, New York, California, and Georgia) from 2001 through 2004. Ascertainment and recruitment protocols for this project have been previously published.3 Cases were live births with standard trisomy 21, and for the current study, case families were limited to those with a maternal MI or MII nondisjunction error. Control infants were live births without major structural birth defects selected randomly from all live births from the same study period and geographical areas as the cases. All participating NDSP sites obtained institutional review board approval and informed consent from all participants.
Maternal questionnaire
Mothers were asked to complete a structured, self-report questionnaire administered by trained study personnel in English or Spanish, dependent on the mother’s primary language. Mothers were asked about various demographic characteristics, including race/ethnicity, household income, and education history of parents and grandparents of the case or control infant. Mothers were also asked about their pregnancy history and smoking and alcohol consumption before and around the time of conception.
Laboratory methods
Biological samples, either a buccal cell sample or venous blood sample, were obtained from the case infant and both birth parents to determine the parental origin and meiotic stage of the nondisjunction error. We genotyped the index infant and both parents for chromosome 21–specific polymorphic markers and established the parental origin of the nondisjunction error using methods outlined in the study by Freeman et al.3 Once parental origin was established, markers targeting the pericentromeric region were used to determine the meiotic stage of the error (MI or MII) as described in the study by Allen et al.6
Statistical analysis
Demographic and lifestyle factors that could be associated with case status included maternal age group (younger than 35 years (referent group) vs. 35 years or older), maternal race/ethnicity (white (referent group), black, Hispanic, or “other”), maternal parity (total number of pregnancies lasting >20 weeks), maternal language (completed English-language version (referent group) vs. completed the Spanish-language version of the maternal questionnaire), and index infant sex (male (referent group) vs. female). Maternal history of alcohol consumption was also considered and was coded as both a dichotomous variable (consumed <50 alcoholic drinks (referent group) vs. consumed ≥50 alcoholic drinks in her lifetime before the birth of the index infant) and a continuous variable (the average number of alcoholic beverages consumed per week in the 2 years before the birth of the index infant). Similarly, maternal smoking was analyzed and was coded as both a dichotomous variable (smoked <100 cigarettes (referent group) vs. smoked ≥100 cigarettes in her lifetime before the birth of the index infant) and a continuous variable (pack-years: calculated by multiplying the number of packs smoked per day by the number of years the person smoked before the birth of the index infant).These variables were compared between cases and controls using χ2 tests for all variables except parity and continuous variables for history of smoking and alcohol use, for which we applied the nonparametric Mann–Whitney test. All variables that significantly differed (P < 0.05) between cases and controls were used as potential covariates in all models analyzing low SES variables as the main effect. These variables were then removed from the final models if they did not change the estimate of the OR of the SES variables of interest by >10%.
To test the hypothesis that low SES factors are associated with maternal chromosome 21 nondisjunction and to create an index similar to that used by Torfs and Christianson,22 we defined the following dichotomous variables to represent low SES based on information from the maternal questionnaire: total household income during the year before the birth of the index infant (≤$25,000 vs. >$25,000), level of education of the mother and father (neither parent completed high school vs. at least one parent completed high school), and level of education of the mother’s parents (maternal grandparents of the index child; neither grandparent completed high school vs. at least one grandparent completed high school). An SES index was created based on these variables to quantify the number of low SES “risk factors” present, where the value ranged from 0 (no low SES factors present: household income >$25,000, at least one parent completed high school, and at least one maternal grandparent completed high school) to 3 (three low SES factors present: household income ≤$25,000, neither parent completed high school, and neither maternal grandparent completed high school). Due to small numbers, the SES index was collapsed to create three values: 0 low SES factors present, 1 low SES factor present, and ≥2 SES low factors present.
Multivariate logistic regression models were used to determine an association between maternal history of low SES and case status. Separate models were run using SES index and individual SES variables of interest (household income, parent education, and maternal grandparent education) as the main predictors. Models were run for all case vs. control mothers, as well as for case mothers stratified by meiotic origin of the nondisjunction error, i.e., MI and MII. All demographic variables that differed between cases and controls were added to a model and removed in a backward-elimination process in which covariates were removed one at a time if they did not change the estimate of the OR of the SES variables of interest by >10%. Because the main model tested for the association between the SES index and chromosome 21 nondisjunction and all additional models were run as follow-up, we did not adjust for multiple testing and used P < 0.05 as a threshold for statistical significance.
We conducted follow-up analyses on significant associations between case status and low maternal SES detected in the main models outlined above. First, we tested whether any association was present in mothers of all ages or limited to older mothers by running models stratified by age group. We also tested whether maternal age significantly interacted with low SES to predict case status, coding the interaction term using the maternal age group indicator variable and using maternal age as a continuous variable. Second, we performed analyses stratified by maternal race/ethnicity to determine whether the observed association was present across all race/ethnicity groups. Finally, because the mother’s country of birth might confound an association between low maternal SES and case status, particularly if mothers were born in developing countries, we ran models stratified by maternal country of birth (born in the United States vs. born outside the United States). We also ran models that adjusted for the number of years that the mother lived in the United States and tested for an interaction between low maternal SES and the number of years the mother lived in the United States.
Finally, we performed sensitivity analyses to ensure that significant associations detected in the main models above were robust. First, in case samples for which fathers did not provide a biological sample, we relied solely on the mother’s genotyping to determine the origin of the error. Therefore, we performed analyses among father–mother–case infant families only to ensure that any association was robust to missing genotype data from the father. Next, we performed analyses to ensure that our results were robust to missing SES. First, we performed χ2 analyses to determine whether missing SES was significantly associated with case status, the significant covariates (maternal age, maternal race, and parity), or the mother’s country of birth. We also ran models with a new income variable coded to include mothers with missing income values (0 = missing, 1 = ≤$25,000, and 2 = >$25,000). Finally, we performed analyses using multilevel versions of dichotomous predictor variables to ensure that any significant results were robust to the coding strategy of variables. Specifically, we created an ordinal variable for income (1 = >$100,000; 2 = $75–100,000; 3 = $50–75,000; 4 = $25–50,000; 5 = $10–25,000; and 6 = <$10,000) to compare with the results of models that applied the dichotomous variable for household income to represent low SES (≤$25,000 vs. >$25,000). Statistical analyses were run using SAS 9.2 (Statistical Analysis Software Institute, Cary, NC).
Results
The distributions of demographic characteristics of the 714 case and 977 control families are shown in Table 1 . Case mothers differed from control mothers for maternal race/ethnicity (χ2 = 20.15; P < 0.01), maternal age group (χ2 = 207.62; P < 0.01), parity (Z = 7.79; P < 0.01), and language (χ2 = 9.88; P < 0.01). Similar patterns in ORs were observed when stratified by MI and MII errors (data not shown).
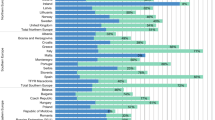
The distributions of SES predictor variables are provided in Table 2 . In initial multivariate logistic regression models, the SES index was used as the main predictor, and the results for these models are shown in Table 3 . These models were originally adjusted for maternal age, maternal race/ethnicity, parity, and language; however, language was removed from the final model because its removal did not change the OR of the main predictor variable by >10%. In models comparing all maternal cases and MI cases only to controls, the SES index was not a significant predictor of case status. However, the significantly increased OR for MII cases vs. controls indicated that mothers of infants with a maternal MII error had an increased history of low maternal SES (OR = 1.81; 95% CI = 1.07–3.05 for 1 low SES factor vs. no low SES factor; OR = 2.17; 95% CI = 1.02–4.63 for ≥2 low SES factors vs. no low SES factor). Next, in separate multivariate logistic regression models, each individual SES variable was used as the predictor variable to determine which SES factor contributed to the association observed between MII cases and controls. Only household income was a significant predictor of case status, with MII cases more likely to have a lower household income as compared with controls ( Table 4 ).
In follow-up analyses, we determined that the association between low household income and MII case status was a significant risk factor in both younger mothers (younger than 35 years: OR = 2.07; 95% CI = 1.15–3.71) and older mothers (35 years or older: OR = 2.28; 95% CI = 1.08–4.82). Consistent with these results, maternal age did not significantly interact with household income to predict MII case status using maternal age as either a dichotomous variable (Wald χ2 = 0.06; P = 0.81) or as a continuous variable (Wald χ2 = 1.81; P = 0.18). In addition, household income was a significant risk factor among all race/ethnicity groups (white: OR = 2.03; 95% CI = 1.01–4.12; black: OR = 4.97; 95% CI = 1.21–20.40; and Hispanic: OR = 2.23; 95% CI = 1.05–4.73). We also found that maternal country of birth (284 controls and 61 MII cases were born outside the United States) did not predict MII case status (OR = 0.87; 95% CI = 0.48–1.57) nor did maternal country of birth significantly interact with household income (Wald χ2 = 0.75; P = 0.39). In addition, the number of years that the mother lived in the United States was not a significant predictor of case status (OR = 1.00; 95% CI = 0.97–1.02) nor did it significantly interact with household income (Wald χ2 = 1.25; P = 0.26). We also performed analyses among MI cases and controls to ensure that this effect was indeed limited to MII cases. Despite a higher frequency of MI cases than MII cases ( Table 1 ), we found that low household income was not associated with MI case status among either mothers born in the United States (OR = 0.89; 95% CI = 0.60–1.32) or those born outside the United States (OR = 1.31; 95% CI = 0.78–2.19).
Finally, sensitivity analyses ensured that our results were robust to missing genotype and SES data. Analyses among father–mother–case infant families only (146 MII cases) indicated that the significant association between low maternal SES and MII case status was robust to missing genotype data from the father (OR = 1.78; 95% CI = 1.01–3.12). For missing income values, MII case status was significantly associated with missing household income (χ2 = 4.44; P = 0.04), with more controls missing income values (10.5%) than MII cases (5.5%). In addition, missing household income was significantly associated with maternal race/ethnicity (χ2 = 73.00; P < 0.01), a significant predictor of MII case status. Specifically, a value for household income was missing for 18.4% of Hispanic mothers, as compared with 4.6% of white mothers and 7.6% of black mothers. Among Hispanic mothers with missing values for household income, the vast majority (83.2%) responded that they did not know their household income, rather than refused to report. However, analyses among Hispanic mothers indicated that missing income was not associated with MII case status (χ2 = 0.62; P = 0.48), with 19.9% of control mothers and 15.6% of MII case mothers missing income. In addition, missing household income was associated with country of the mother’s birth (χ2 = 45.41; P < 0.01), with 6.2% of mothers born in the United States and 16.5% of mothers born outside the United States missing household income. However, the majority of mothers born outside the United States (87.8%) were Hispanic. Missing household income was not associated with maternal age or parity, two additional predictors of MII case status. In addition, the risk of an MII case was significantly increased for mothers in the low income group (≤$25,000; OR = 2.97; 95% CI = 1.36–6.44) as compared with those with missing income information (referent group), whereas the association was in the same direction but not significant for those in the high income group (>$25,000; OR = 1.57; 95% CI = 0.73–3.41). Finally, our results were robust to the dichotomous coding strategy of the income. Low household income was a significant predictor of MII case status whether it was coded as a dichotomous variable (OR = 1.79; 95% CI = 1.17–2.73; Table 4 ) or as an ordinal variable (OR = 1.18; 95% CI = 1.03–1.35), where those in increasingly lower income ranges were more likely to be MII cases.
Discussion
The goal of this study was to further investigate a previous report that maternal lifetime exposure to low SES is significantly associated with having a clinically recognized pregnancy with DS,22 and more specifically that this association is limited to cases with maternal MII nondisjunction error.23 We used the large and diverse case–control population from the NDSP to conduct our study. Using this independent data set, we confirmed that low maternal SES, best defined by low household income, was associated with having a live-born infant with DS due to a maternal MII nondisjunction error. Specifically, mothers whose household income the year before the birth of the infant was $25,000 or less were roughly 80% more likely to have an infant with DS as compared with control mothers. This association remained significant after adjustment for maternal age, race/ethnicity, and parity. Of note, this association between low maternal SES and a maternal MII nondisjunction error was not restricted to older mothers (35 years or older). In addition, this association was present among white, black, and Hispanic mothers.
Despite the larger sample size of MI cases (n = 532) as compared with MII cases (n = 182), a statistically significant association between MI case status and low maternal SES was not detected. However, it is important to note that the OR point estimates indicated that MI cases were more likely to have a history of 1 (OR = 1.11) or ≥2 (OR = 1.31) low maternal SES factors as compared with controls. Further studies with larger sample sizes could discern whether there is a similar association between maternal SES and MI cases as detected in MII cases but with a smaller effect.
A strength of this study lies in the large number of cases and controls, who were recruited from multiple states, including Arkansas, Iowa, New Jersey, New York, California, and Georgia. Therefore, this study extends the findings of the previously published studies on maternal SES and DS, which were limited to recruitment in California. In addition, we performed sensitivity analyses to ensure that our results were robust to potential biases, including those resulting from misclassification of nondisjunction errors due to the absence of a participating father as well as those resulting from missing household income information. In our data set, the majority of the 19.9% of Hispanic control mothers and the 15.6% of Hispanic case mothers with missing data for income were reported as “unknown,” not “refused.” Of note, missing income was not significantly associated with MII case status among Hispanic mothers. We further examined the potential influence of the mother’s country of birth and found that neither the mother’s country of birth nor the number of years the mother had lived in the United States were significant predictors of case status.
Of note, the significant association of low maternal SES, specifically household income, was limited to MII cases and was not detected among MI cases. This pattern suggests that SES factors associated with access to prenatal health care, prenatal diagnosis, and differential use of diagnostic information by the health-care professionals or mothers cannot explain our results. If these were involved, the association would be significant among both types of maternal meiotic errors, not limited to MII errors. However, the biological mechanism underlying the effect of low maternal SES exposure on MII nondisjunction is unclear, and further studies are warranted. Because SES is a proxy for environmental exposures, our results suggest that some environmental factors have their influence on only specific stages of meiosis.22
Clearly, the importance of different components of the meiotic machinery and the specific processes involved in segregating homologues in MI and sister chromatids in MII differ significantly. For example, sister chromatid cohesion is released from chromatid arms at anaphase I to enable segregation of homologues and from sister centromeres at anaphase II to help properly segregate chromatids. It has been clearly shown that loss of centromere cohesion is one of the major causes of maternal age–dependent nondisjunction.24,25,26,27,28,29,30 In addition, the centromeric and pericentromeric regions are important for chromosome segregation, for which its alteration of associated processes (e.g., hypomethylation) lead to centromeric decondensation and genomic instability.31,32,33 Of note, De La Fuente et al. 34 has shown that ATRX, a chromatin-remodeling factor known to regulate DNA methylation at repetitive sequences of the human genome, binds to pericentromeric heterochromatin domains in mouse oocytes at the metaphase II stage. At that stage, it is involved in mediating chromosome alignment at the meiotic spindle. Later, Baumann et al. showed that transgenic ATRX–RNA interference oocytes showed a high rate of aneuploidy at MII due to chromosome nondisjunction, presence of single chromatids, and premature anaphase II onset. We have shown that recombination near the centromere is highly associated with maternal MII errors35,36 and that this association increases with maternal age.12,37
Several reported environmental exposures associated with chromosome 21 nondisjunction appear to differ between MI and MII errors, suggesting that different aspects of the meiotic machinery may be more or less vulnerable under different conditions. Two reports suggest that use of tobacco products may be exacerbated by oral contraceptive use around the time of conception and that such effects are limited to specific recombination configurations38 and meiotic errors.38,39 Similarly, Ghosh et al.40 have shown that total telomere lengths are shorter in older mothers who had MI or MII nondisjunction errors as compared with mothers with a normal meiotic outcome and, of importance, those with a MII error showed even shorter lengths than those with MI errors, adjusting for maternal age. Using this same NDSP population, we have recently found that lack of folic acid supplementation around the time of conception is associated with only MII errors among older mothers.41
For MII nondisjunction, the accumulation of environmental toxins over time may interact with the vulnerable pericentromeric recombination pattern to increase the occurrence of a nondisjunction event. This accumulation might be expedited among women with a history of low SES as compared with women with a higher SES, thus showing this effect among younger mothers in addition to older mothers. Therefore, future studies should investigate the interaction between recombination patterns and exposure factors associated with low SES (e.g., environmental toxins or poor nutrition).
Our study does have some potential limitations. First, families were recruited into the NDSP based on the birth of a live-born infant; therefore, our data set includes only mothers who either did not obtain a prenatal diagnosis of DS for the fetus or had a prenatal diagnosis of DS for the fetus and chose not to terminate the pregnancy. Clearly, a bias in SES could be present among those who obtained a prenatal diagnosis and those who chose or did not choose to terminate the pregnancy. However, the fact that our results are limited to MII cases makes this less likely. Another potential limitation of the study is the assessment of maternal SES factors. We analyzed data from SES factors that range from the mother’s fetal life (maternal grandparent education) to the conception of the case or control infant (household income the year before the infant’s birth). However, these SES factors are only snapshots of the full-lifetime SES picture. In addition, assessment of the SES factors relied on the mother to accurately report the information. Of note, the specific SES factor associated with MII cases was household income, a variable that assesses the SES status of the mother only the year before the birth of the index child, rather than the other variables that assess more of the lifetime SES status of the mother. Whether this pinpoints an important time point of vulnerability or is simply a spurious association remains unknown. Finally, the case mothers with maternal errors may not represent a random selection of all maternal errors leading to live births with DS because such case parents had to provide a biological sample and chromosome 21 markers had to be informative in order to determine the type of nondisjunction error.
Of note, this study confirms earlier reports that a maternal history of low SES, specifically low household income, is associated with having an infant with DS due to a maternal MII nondisjunction error. This finding was independent of the effect of maternal age and was detected among mothers younger and older than 35 years. The etiology of maternal nondisjunction is clearly multifactorial, and further studies are needed to discern the biological mechanisms involved in the association between maternal SES and nondisjunction.
Disclosure
The authors declared no conflict of interest.
References
Parker SE, Mai CT, Canfield MA, et al. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol 2010;88:1008–1016.
Sherman SL, Allen EG, Bean LH, Freeman SB . Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev 2007;13:221–227.
Freeman SB, Allen EG, Oxford-Wright CL, et al. The National Down Syndrome Project: design and implementation. Public Health Rep 2007;122:62–72.
Mikkelsen M, Hallberg A, Poulsen H, Frantzen M, Hansen J, Petersen MB . Epidemiology study of Down’s syndrome in Denmark, including family studies of chromosomes and DNA markers. Dev Brain Dysfunc 1995;8:4–12.
Gómez D, Solsona E, Guitart M, et al. Origin of trisomy 21 in Down syndrome cases from a Spanish population registry. Ann Genet 2000;43:23–28.
Allen EG, Freeman SB, Druschel C, et al. Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Hum Genet 2009;125:41–52.
Yoon PW, Freeman SB, Sherman SL, et al. Advanced maternal age and the risk of Down syndrome characterized by the meiotic stage of chromosomal error: a population-based study. Am J Hum Genet 1996;58:628–633.
Antonarakis SE, Petersen MB, McInnis MG, et al. The meiotic stage of nondisjunction in trisomy 21: determination by using DNA polymorphisms. Am J Hum Genet 1992;50:544–550.
Ballesta F, Queralt R, Gómez D, et al. Parental origin and meiotic stage of non-disjunction in 139 cases of trisomy 21. Ann Genet 1999;42:11–15.
Muller F, Rebiffé M, Taillandier A, Oury JF, Mornet E . Parental origin of the extra chromosome in prenatally diagnosed fetal trisomy 21. Hum Genet 2000;106:340–344.
Lamb NE, Yu K, Shaffer J, Feingold E, Sherman SL . Association between maternal age and meiotic recombination for trisomy 21. Am J Hum Genet 2005;76:91–99.
Oliver TR, Feingold E, Yu K, et al. New insights into human nondisjunction of chromosome 21 in oocytes. PLoS Genet 2008;4:e1000033.
Oliver TR, Tinker SW, Allen EG, et al. Altered patterns of multiple recombinant events are associated with nondisjunction of chromosome 21. Hum Genet 2012;131:1039–1046.
Warren AC, Chakravarti A, Wong C, et al. Evidence for reduced recombination on the nondisjoined chromosomes 21 in Down syndrome. Science 1987;237:652–654.
Ghosh S, Bhaumik P, Ghosh P, Dey SK . Chromosome 21 non-disjunction and Down syndrome birth in an Indian cohort: analysis of incidence and aetiology from family linkage data. Genet Res (Camb) 2010;92:189–197.
Ghosh S, Feingold E, Dey SK . Etiology of Down syndrome: evidence for consistent association among altered meiotic recombination, nondisjunction, and maternal age across populations. Am J Med Genet A 2009;149A:1415–1420.
Nagaoka SI, Hassold TJ, Hunt PA . Human aneuploidy: mechanisms and new insights into an age-old problem. Nat Rev Genet 2012;13:493–504.
Pacchierotti F, Eichenlaub-Ritter U . Environmental hazard in the aetiology of somatic and germ cell aneuploidy. Cytogenet Genome Res 2011;133:254–268.
Penrose LS . Genetical aspects of mental deficiency. Proceedings of the International Copenhagen Congress on the Scientific Study of Mental Retardation. 1964:165–172.
Susiarjo M, Hassold TJ, Freeman E, Hunt PA . Bisphenol A exposure in utero disrupts early oogenesis in the mouse. PLoS Genet 2007;3:e5.
Eichenlaub-Ritter U, Wieczorek M, Lüke S, Seidel T . Age related changes in mitochondrial function and new approaches to study redox regulation in mammalian oocytes in response to age or maturation conditions. Mitochondrion 2011;11:783–796.
Torfs CP, Christianson RE . Socioeconomic effects on the risk of having a recognized pregnancy with Down syndrome. Birth Defects Res Part A Clin Mol Teratol 2003;67:522–528.
Christianson RE, Sherman SL, Torfs CP . Maternal meiosis II nondisjunction in trisomy 21 is associated with maternal low socioeconomic status. Genet Med 2004;6:487–494.
Angell RR . Predivision in human oocytes at meiosis I: a mechanism for trisomy formation in man. Hum Genet 1991;86:383–387.
Angell RR, Xian J, Keith J, Ledger W, Baird DT . First meiotic division abnormalities in human oocytes: mechanism of trisomy formation. Cytogenet Cell Genet 1994;65:194–202.
Hodges CA, Revenkova E, Jessberger R, Hassold TJ, Hunt PA . SMC1beta-deficient female mice provide evidence that cohesins are a missing link in age-related nondisjunction. Nat Genet 2005;37:1351–1355.
Liu L, Keefe DL . Defective cohesin is associated with age-dependent misaligned chromosomes in oocytes. Reprod Biomed Online 2008;16:103–112.
Chiang T, Duncan FE, Schindler K, Schultz RM, Lampson MA . Evidence that weakened centromere cohesion is a leading cause of age-related aneuploidy in oocytes. Curr Biol 2010;20:1522–1528.
Fragouli E, Alfarawati S, Goodall NN, Sanchez-Garcia JF, Colls P, Wells D . The cytogenetics of polar bodies: insights into female meiosis and the diagnosis of aneuploidy. Mol Hum Reprod 2011;17:286–295.
Pellestor F, Andréo B, Anahory T, Hamamah S . The occurrence of aneuploidy in human: lessons from the cytogenetic studies of human oocytes. Eur J Med Genet 2006;49:103–116.
Tuck-Muller CM, Narayan A, Tsien F, et al. DNA hypomethylation and unusual chromosome instability in cell lines from ICF syndrome patients. Cytogenet Cell Genet 2000;89:121–128.
Dodge JE, Okano M, Dick F, et al. Inactivation of Dnmt3b in mouse embryonic fibroblasts results in DNA hypomethylation, chromosomal instability, and spontaneous immortalization. J Biol Chem 2005;280:17986–17991.
Baumann J . Down syndrome cell adhesion molecule–a common determinant of brain and heart wiring. Pediatr Res 2007;62:1.
De La Fuente R, Viveiros MM, Wigglesworth K, Eppig JJ . ATRX, a member of the SNF2 family of helicase/ATPases, is required for chromosome alignment and meiotic spindle organization in metaphase II stage mouse oocytes. Dev Biol 2004;272:1–14.
Lamb NE, Feingold E, Savage A, et al. Characterization of susceptible chiasma configurations that increase the risk for maternal nondisjunction of chromosome 21. Hum Mol Genet 1997;6:1391–1399.
Lamb NE, Freeman SB, Savage-Austin A, et al. Susceptible chiasmate configurations of chromosome 21 predispose to non-disjunction in both maternal meiosis I and meiosis II. Nat Genet 1996;14:400–405.
Oliver TR, Tinker SW, Allen EG, et al. Altered patterns of multiple recombinant patterns are associated with nondisjunction of chromosome 21. Hum Genet 2012;131:1039–1046.
Ghosh S, Hong CS, Feingold E, et al. Epidemiology of Down syndrome: new insight into the multidimensional interactions among genetic and environmental risk factors in the oocyte. Am J Epidemiol 2011;174:1009–1016.
Yang Q, Sherman SL, Hassold TJ, et al. Risk factors for trisomy 21: maternal cigarette smoking and oral contraceptive use in a population-based case-control study. Genet Med 1999;1:80–88.
Ghosh S, Feingold E, Chakraborty S, Dey SK . Telomere length is associated with types of chromosome 21 nondisjunction: a new insight into the maternal age effect on Down syndrome birth. Hum Genet 2010;127:403–409.
Hollis ND, Allen EG, Oliver TR, et al. Preconception folic acid supplementation and risk for chromosome 21 nondisjunction: a report from the National Down Syndrome Project. Am J Med Genet A 2013;161:438–444.
Acknowledgements
The authors thank Rupa Masse, Maneesha Yadav-Shaw, and Weiya He for their laboratory assistance. They also thank all personnel at each NDSP site. A very special thanks go to the families whose participation made this study possible. This work was supported by NIH R01 HD38979. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hunter, J., Allen, E., Shin, M. et al. The association of low socioeconomic status and the risk of having a child with Down syndrome: a report from the National Down Syndrome Project. Genet Med 15, 698–705 (2013). https://doi.org/10.1038/gim.2013.34
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2013.34
Keywords
This article is cited by
-
Population monitoring of trisomy 21: problems and approaches
Molecular Cytogenetics (2023)
-
Variations in chromosomal aneuploidy rates in IVF blastocysts and early spontaneous abortion chorionic villi
Journal of Assisted Reproduction and Genetics (2020)
-
The demographic data and the high frequency of chromosome/chromatid breaks as biomarkers for genome integrity have a role in predicting the susceptibility to have Down syndrome in a cohort of Egyptian young-aged mothers
Egyptian Journal of Medical Human Genetics (2019)
-
Risk factors for Down syndrome
Archives of Toxicology (2016)
-
Synthetic combinations of missense polymorphic genetic changes underlying Down syndrome susceptibility
Cellular and Molecular Life Sciences (2016)