Abstract
Purpose: The Alpha Coded Testing Study investigated the risks, benefits, and psychological impact of home genetic testing for α1-antitrypsin deficiency.
Methods: In the study, 996 adult individuals requested and returned a home-administered, confidential, fingerstick blood test.
Results: Individuals highly rated the benefits of establishing a diagnosis (82%), helping family members (86%), and anticipating peace of mind (79%). 78% of 239 current smokers reported a high likelihood of smoking cessation if diagnosed with AATD. After testing, more than 60% indicated that they would share the results with family and physicians but < 30% would share results with insurance companies.
Conclusions: Confidential home testing for genetic disorders requires a comprehensive program of participant support.
Similar content being viewed by others
Main
α1-Antitrypsin deficiency (AATD [MIM 107400]) is a genetic condition that can lead to early onset emphysema and hepatic impairment in some individuals.1 The gene that codes for α1-antitrypsin deficiency is located on chromosome 14 and more than 100 genotypic variants have been described. The serum levels of α1-antitrypsin are determined by each of 2 codominant genes. The most common phenotype in the US and world is PiMM (also called PiM) in which both AAT genes produce M protein. The two most common deficiency alleles S and Z produce proteins that are made in the liver but fail to fold properly for hepatic egress. At least one S or Z gene is found in 4% to 6% of the US population.2
Individuals with symptoms are usually severely deficient in AAT. The phenotypes associated with severe deficiency are most commonly PiZZ (also called PiZ) and PiSZ. PiZZ AATD is the most common cause of early onset emphysema with a mean age at time of pulmonary impairment at 35.3 Rarely, individuals with the carrier state PiMZ develop symptoms of lung or liver disease.4
Not all individuals with PiZZ AATD develop symptoms of lung and/or liver disease. In fact, there is substantial variability in the age of onset and severity of disease among PiZZ individuals even within families.5 Although some nonsmokers develop severe lung disease, the majority of pulmonary impairment occurs in ex-smokers or current cigarette smokers who develop emphysema. Therefore, identification of AATD allows targeted intensive smoking cessation efforts. Intravenous augmentation therapy to restore serum AAT levels to higher levels remains costly,6 but has been shown to slow the course of emphysema in some patients.7
Because early onset severe emphysema is a devastating illness for affected individuals, interest in testing other family members for the Z or S allele has increased. Because of concerns about genetic discrimination in the absence of clinical disease and the lack of confidentiality of medical records, particularly from medical and life insurance entities, the AATD patient community has proactively supported a mechanism to provide confidential testing.
Despite potential benefits of genetic testing, some studies report hesitation and fear associated with genetic testing. Telephone interviews within the general population have suggested that the issues are complicated by a lack of understanding of the science and anxiety that is often unfocused.8,9 The possibility of genetic discrimination related to insurance has been cited as a major external factor concerning individuals considering genetic testing.10,11 A 1996 survey of 332 genetic support groups found that 40% of respondents had been asked about genetic diseases or disabilities on an application for health insurance. Of those 47% were denied coverage, and 25% were denied life insurance compared to 3% denied coverage in the general population.12 The Health Insurance Portability and Accountability Act (HIPAA) prohibits certain uses of genetic information in determining insurance eligibility, but places no limits on rate setting.13 Uninsurability appears to be a valid concern for potential genetic test takers.
Other studies have shown public interest in genetic testing, especially among at risk populations.14–16 Eighty four percent of first-degree relatives of ovarian cancer patients who believed they were likely to be a gene carrier expressed interest in testing, compared to 63% of women who considered themselves unlikely to be carriers.17
Research is emerging evaluating other factors that may influence interest in genetic testing. Some studies have found no influence of demographic factors on the decision to perform a genetic test.18,19 Cost and convenience may play a role in motivation for testing. In one study, over 90% of women considering testing for breast cancer susceptibility genes expressed interest in testing if it was free, but interest dropped to 60% if testing involved cost.20 Among an HMO population, persons were more likely to undergo testing for cystic fibrosis if they could be tested upon initial approach with minimal effort.21
Although many studies have investigated interest in genetic testing, relatively few studies have evaluated specific beliefs about testing, such as anticipated risks and benefits. Furthermore, most studies examine beliefs a priori, without longitudinal follow-up after test results have been disclosed. The present study examines specific beliefs both before and after genetic testing for α1-antitrypsin deficiency (AATD), one of the most common yet misdiagnosed genetic disorders worldwide. The project was designed to provide a confidential, free, and convenient method of testing in order to reduce the potential confounding impact of these variables.
MATERIALS AND METHODS
Study design received input from individuals with AATD, physicians, psychologists, and genetic counselors knowledgeable about AATD. It was reviewed by the Ethical, Legal, and Social Implications (ELSI) Committee of the Alpha-1 Foundation, received approval from the Institutional Review Board for Human Subjects at the Medical University of South Carolina (MUSC), and carried a Certificate of Confidentiality from the Department of Health and Human Services. Patients signed written informed consent before testing.
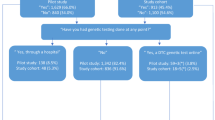
The ACT Study utilized the infrastructure of the Alpha-1 Foundation, an organization founded by AATD-affected individuals to promote research. The study was advertised through a patient registry, regional meetings, and web site. Advertisements began in July 2001 followed by enrollment beginning in January 2002. Individuals requesting a test kit were mailed a study packet that included (1) informed consent, (2) a pretest questionnaire, (3) a fingerstick blood-spot test kit (Fig. 1), (4) a brochure discussing the testing procedure, and (5) a postage-paid preaddressed return envelope. Returned test kits were coded at MUSC and mailed to the University of Florida’s Alpha-1 Genetics Laboratory. The blood spots were subjected to PCR analysis to determine if one or two copies of either the S or Z gene were present. Dried blood spot AAT concentration was matched to genotype. Results were returned to MUSC. Participants were then mailed a follow-up packet that consisted of (1) a letter detailing the results of the test, (2) a posttest questionnaire, and (3) a postage-paid preaddressed return envelope. In addition, all participants who tested either deficient for AATD (PiZZ or PiSZ) or were a carrier (PiMZ) received an informational support brochure addressing possible health concerns. Both deficient and carrier groups received an invitation to join the Alpha-1 Research Registry, and all participants were offered free telephone support including consultation with a genetic counselor if desired.
Participants
Between January 2002 and February 2003, 3551 kits were requested. Individuals could request kits for themselves and/or other family members. Of these pretest packets, 1159 (33%) were returned with completed blood tests and pretest questionnaires. Some 163 individuals under the age of 18 years were excluded from pretest questionnaire analysis leaving a study cohort of 996 persons. After testing, these individuals were sent a posttest packet including questionnaire and statement of genotype status. To date, 700 (63% of the pretest sample) participants have returned the posttest questionnaire with 512 first time testers, age 18 or over included in posttest questionnaire analysis.
Survey materials
Pretest
Pretest questionnaires included items pertaining to demographics, smoking, reasons for seeking testing, and referral source. Six potential risks and six potential benefits were presented in a Likert format (1 = no risk or benefit, 5 = high risk or benefit). Other questions concerning beliefs (improved health, improved psychological well-being, increased health care costs, and expected discrimination) were presented in Likert format. Additionally, participants were asked to indicate the likelihood of a PiZZ child if both parents are PiMZ. Participants could choose among responses of 0%, 25% (correct answer), 50%, 75%, 100%, or “I don’t know.”
Posttest
The posttest questionnaire queried plans to divulge results of genetic testing to others. Additionally, participants were asked to rate anticipated effects from genetic testing. These effects included both potential benefits and harms.
Data Analysis
Demographic information is reported as a percent of the total response to each individual question. Likert scores of 4 and 5 were considered high. Values of P < 0.05 were considered significant for all analyses. Statistical analysis was performed using Stata (College Station, TX). Two sided t tests were used to compare age distributions between subgroups of participants. An overall median score for the risks and an overall median score for the benefits of testing at the pretest questionnaire were determined for those participants who answered all risk/benefit questions. The Wilcoxon signed rank test was used to compare the distribution of those median scores. The Wilcoxon rank sum test also was used to compare the distribution of responses to questions in Likert format between subgroups on the pretest questionnaire. The Chi-Square test for trend in binomial proportions was used to detect a trend in the proportion of correct answers to the genetic question with an ordered column variable. The Kruskal Wallis test and Wilcoxon rank sum test was used to compare the distribution of responses stratified by genotype to questions in Likert format on the posttest questionnaire. Fishers exact test was used to test for independence in 2 by 2 and 3 by 2 contingency tables.
RESULTS
The 996 participants averaged 42.4 ± 16.3 years (mean ± SD) with a range of 18 to 82 years. Consistent with known demographics of AATD, 93% of participants were Caucasian. Sixty one percent of participants were female. A total of 84% of participants reported having health insurance, and 89% of participants report believing they will receive very important information about their genes reporting the highest score of 4 or 5 on the Likert scale. The primary referral source for recommending testing for AATD was family, and reasons that the test was suggested are reported in Table 1. Genetic testing results indicated 520 negative results of genotype MM(464), MS(53), or SS(3), 407 carrier results of genotype MZ, and 68 deficient results of SZ(27) or ZZ(40). Rare alleles requiring serum phenotyping (PiZNull) were suspected because of low protein concentrations and confirmed in 2 cases.
Perceived risks on pretest questionnaire
Less than 40% of participants anticipated a high risk of increased insurance premiums (Table 2). Other potential risks included potential loss of insurance (31%), psychological risks (18%), and increased stress (13%). Younger participants were more likely to anticipate risks of losing health insurance (r = 0 0.13, P < 0.001), higher insurance premiums (r = 0.14, P < 0.001), losing employment (r = 0.12, P < 0.001), or psychological risks (r = 0.16, P < 0.001) than older participants. Education level was loosely correlated with anticipated risk of losing health insurance (r = 0.08, P < 0.03) and risk of higher insurance premiums (r = 0.1, P < 0.004). No other demographic variables predicted anticipated risks.
Perceived benefits on pretest questionnaire
In contrast to potential risks of genetic testing, participants anticipated significant benefits (Table 2). High scores were recorded for the effect of genetic knowledge on the family (86%) and for establishing a firm diagnosis (82%). Anticipated benefits did not significantly differ according to familial risk or demographic variables. Perceived benefits greatly outweighed perceived risks, as distribution of overall median scores for the six listed benefits of testing was greater than for the risks (P < 0.0001).
Confidentiality
Confidentiality was an important reason for testing through the ACT Study for the majority of participants with 61% rating its importance high. There was no difference in the rating of confidentiality depending on whether the test was recommended by a physician (N = 73), family member (N = 586), or other source(s). Confidentiality was more important to the participant if the test was suggested because a family member had AATD compared to those being tested because of symptoms (P < 0.001). Concern for confidentiality was inversely correlated with participant age (P = 0.03). Persons entering the test with high levels of concern about confidentiality were more likely to anticipate other risks than persons without this level of confidentiality concern (Table 3).
Smoking
Of 239 respondents who were current smokers (26% of the entire cohort), 78% report a high likelihood of quitting smoking if they were to be diagnosed with AATD. Current Smokers were younger (age 38 ± 14.5) than current nonsmokers (age 44 ± 16.6) (P < 0.0001). Thirty two percent of smokers did not have medical insurance compared to 11% of nonsmokers (P < 0.0001). Smoker’s family members were more likely to have recommended testing as compared to nonsmokers (P = 0.0003). Smokers were more concerned about the risk of a change in the identity of their biological parent (P = 0.03) and more likely to rate availability of a drug treatment as an important benefit of establishing a diagnosis (P = 0.048).
Index participants
Index participants are those whose test was suggested because of liver or lung disease symptoms (N = 136). Index participants were older than non-Index participants (N = 715) with mean age 52 ± 15 versus 40 ± 16, and were more likely to be recommended by a physician only (P < 0.0001). Index participants rated the benefit of establishing a diagnosis and the availability of a drug treatment with a diagnosis significantly more important than non-Index participants (P < 0.04). Non-Index participants are more concerned about confidentiality, losing health insurance, higher health insurance premiums, and psychological risks associated with genetic testing (P < 0.05).
Knowledge of α1 genetics
Each participant was asked to answer a question about the probability of having a child with PiZZ α1 if both parents have PiMZ. Overall 39% of participants answered the question correctly, 28% answered incorrectly, and 33% responded, “I don’t know.” The question was answered correctly by more participants who performed research on AATD before participating (OR 3.14 [95% CI 2.35, 4.22]) and by participants recommended for testing by a physician (OR 1.65 [95% CI 1.00, 2.75]). Participants who answered the question correctly were more educated and younger than participants who answered the question incorrectly (P < 0.0001 and P < 0.01).
Posttest questionnaire
The subset of respondents who returned the posttest questionnaire (n = 512) did not significantly differ from the 404 respondents who only completed the pretest with regard to race, gender, or age. Participants returning a posttest questionnaire were more educated than participants who did not return a posttest questionnaire (P = 0.005). We compared responses to the post-test questionnaire between participants receiving a first time negative (PiMM, PiMS, N = 277), carrier (PiMZ, N = 203), and deficient (PiZZ or PiSZ, N = 32) test result. Table 4 demonstrates willingness to disclose test results with others.
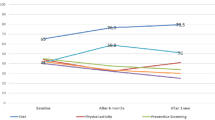
Results of subgroup responses to 10 questions about participant expectations of events or feelings after the test result are shown in Table 5. Carriers and participants with a deficient test result were more likely to anticipate depression and anxiety compared to participants with a negative result (P ≤ 0.0001). Of interest is that persons with deficient test results feel they rate the expectation of “improved health” more likely than persons with a carriers or negative test result.
DISCUSSION
The technology to provide home testing for genetic diseases remains in its infancy. In general, few participants reported difficulty with the use of home lancets to produce blood spots and most comments received at the coordinating center were highly favorable about the testing program. The high rate of nonreturned kits likely represents the combined effects of fear concerning the fingerstick, family members ordering test kits for other family members not interested in testing, anxieties concerning the testing process, and inertia related to the paperwork associated with testing. Technical aspects of the home test kit have been described elsewhere.22
We were surprised that the majority of participants dismissed most of the proposed risks of testing and reported that risks were not in general discussed with family members. The greatest benefits were anticipated for the helpful effect of genetic information for the family and for establishing firm diagnoses that assist with life planning.
Confidentiality was an important reason for testing through the ACT study. Persons most concerned about confidentiality were more likely to be concerned about risks associated with testing. Results from the current study indicated that younger age is related to greater perceived risk. This may reflect a belief or fear that a diagnosis of AATD could have long-term negative consequences. Many members of the AATD patient community are aware of the case of Terri Sergeant, recently awarded damages by the Equal Employment Opportunity Commission after being fired from her job as an office manager because she required extremely expensive medication to treat her AATD.13
The 24.4% prevalence of smoking among study participants is consistent with the current national statistic of 23.5%.23 One of the most important outcomes of establishing a diagnosis is to effect smoking cessation because smoking is the most common environmental factor associated with developing AATD related lung disease. More than 75% of ACT participants report a strong likelihood of smoking cessation if they are diagnosed with AATD. Little is known about smoking cessation among a newly diagnosed adult population predisposed for lung disease. Followup of this cohort may provide insight to success in quit attempts because smoking cessation intent does not equate with cessation. Results from the National Heart Lung and Blood Institute’s Registry of Patients with the deficiency of α1 antitrypsin suggest that the AATD population is amenable to smoking cessation since only 8.3% of that cohort reported current smoking.24 Also, previous studies indicate that screening at birth leads to a lower incidence of smoking among PiZZ individuals, suggesting that at-risk populations may benefit from early detection.25
Although < 40% of participants rated the likelihood of losing insurance or increased premiums a high risk at the pretest questionnaire, the posttest results were different. Overall 40% were unsure if they will tell their physician about their test result and 80% were unsure if they will tell their health insurance company. This discrepancy is interesting and worthy of further study to understand if it is unique to this study design.
Participants receiving a deficient test result rate the expectation of improved health higher compared to participants with a negative test result. This finding may suggest that knowledge of genetic status may increase a sense of control and therefore serve as a stimulus for healthy behavior change for these participants.
Past studies show an interest and willingness to pursue genetic testing, especially within specific at risk populations.16,17 Although self reported interest might be high, this does not always translate into actual behavior. Among individuals who initially showed interest in testing for Huntington’s disease (about 2/3 of an at risk sample), only 15% engaged in testing.26 Return rates from the ACT Study are similar as only 33% of requesters returned a completed test. Factors influencing the decision to follow through with genetic testing are not well understood. Cost, perceived risk, convenience, and education level have all been linked to the decision to go forth with genetic testing.17,20,21 Although such factors may be influential, perhaps other social, emotional, and psychological issues play a role in this decision.
The majority of ACT testers did not report depression and anxiety after knowledge of genetic status. However, a subgroup was different with 4 of 31 deficient participants reporting high scores for these questions. This finding suggests that some participants with a deficient test result may perceive themselves as more psychologically vulnerable. We found 25% of persons with a deficient test result reported a moderate likelihood of depression with a score of 3% versus 12% of carriers and 7% of participants with a negative test result. Results were similar for anticipated anxiety. The findings from the present study indicate that knowledge of a deficient test does result in moderate distress for some people.
Limitations
The primary limitation of this study is its use of a self-selected sample. Participants sought out and/or volunteered for genetic testing, implying that they had some degree of comfort with the testing process and were perhaps well equipped to accept the results. Those truly anxious or fearful of genetic testing may have ignored the opportunity. The best methodology for studying interest and beliefs for genetic testing among the general population would use epidemiologic research.8,9 However, testing of the general population has not been recommended in the recently published Statement on Standards for the Diagnosis and Management of Individuals with AATD.27
Another limitation was the use of nonstandardized, researcher-adapted assessment measures to examine perceptions and beliefs about genetic testing. Prior research on interest in and anticipated outcomes from genetic testing has predominantly included nonstandardized assessment measures as well, including qualitative data derived from focus groups. As genetic testing becomes more widespread, formal assessment procedures will become necessary and will allow for cross-study comparisons.28
It is possible that risks and benefits of testing may have been scored differently if circumstances of testing were different. We provided a highly confidential testing environment in which patient identifiers could be removed after testing. These protections were essential to determine if anxiety about the testing was focused on confidentiality or other aspects of testing.
We were disappointed with the posttest questionnaire return rates despite intensive efforts with telephone calls, mailed reminders, and monetary stipends to improve return rates. Not all participants answered all questions. Although we found few differences between the pretest questionnaires of those who returned and did not return their posttest paperwork, the 63% return raises the possibility of selection bias and limited the numbers of PiZZ and PiSZ participant responses included in the posttest questionnaire analysis.
Finally, the posttest questionnaire assessed anticipated but not actual effects. Posttest questionnaires were delivered at the same time as test results. At best, these anticipated effects reflect initial reaction upon knowledge of genotype. Future research should examine the intensity and duration of both psychological and physical impact of AAT deficiency longitudinally, although one study has shown that general quality of life among AAT-deficient individuals remains fairly stable over a two-year period.29
Conclusions
As knowledge of genetics grows, so does the technology for quick and inexpensive testing. It is not inconceivable that the future will allow for home testing for a variety of genetic conditions. Public reaction and tolerance for the availability of such a market is unclear. Gaining more understanding toward motivators for genetic testing and the reaction to mailed results in the context of a comprehensive telephone support system will greatly influence the future of genetic testing. Evidence to date suggests that some people are receptive to home genetic testing.
This study sought to further examine perceived risks and benefits both before and after testing for AATD. Before testing, anticipated benefits appeared to outweigh anticipated risks. After testing, respondents who tested deficient or carriers for AATD anticipated some negative outcomes, including depression, anxiety, and increased health insurance costs. However, in agreement with expectations from the initial questionnaire, most reported feeling more in control of their lives and persons with an AATD diagnosis expected improved health. In the confidential setting of the ACT study, participants perceive the benefits of testing to greatly outweigh the risks.
References
OMIM. Online Mendelian Inheritance in Man. 2003. Available at: http://www.ncbi.nlm.nih.gov/entrez/Omim/mimstats.html.
de Serres FJ . Worldwide racial and ethnic distribution of alpha1-antitrypsin deficiency: summary of an analysis of published epidemiologic surveys. Chest 2002; 122: 1818–1829.
Stoller J, Smith P, Yang P, Spray J . Physical and social impact of alpha1 antitrypsin deficiency: results of a study. Clev Clin J Med 1994; 61: 461–467.
Sandford A, Chagani T, Weir T, Connett J, Anthonisen N, Pare P . Susceptibility genes for rapid decline of lung function in the Lung Health Study. Am J Respir Crit Care Med 2001; 163: 469–473.
Silverman E, Province M, Campbell E, Pierce J, Rao D . Family study of alpha1-antitrypsin deficiency: Effects of cigarette smoking, measured genotype, and their interaction on pulmonary function and biochemical traits. Genet Epidemiol 1992; 9: 317–331.
Mullins CD, Wang J, Stoller JK . Major components of the direct medical costs of alpha1-antitrypsin deficiency. Chest 2003; 124: 826–831.
Alpha-1 Antitrypsin Deficiency Study Group. Survival and FEV1 decline in individuals with severe deficiency of alpha1-antitrypsin. Am J Respir Crit Care Med 1998; 158: 49–59.
Andrykowski MA, Munn RK, Studts JL . Interest in learning of personal genetic risk for cancer: A general population survey. Prev Med 1996; 25: 527–536.
Andrykowski MA, Lightner R, Studts JL, Munn RK . Hereditary cancer risk notification and testing: How interested is the general populationJ Clin. Oncol 1997; 15: 2139–2148.
Hudson KL, Rothenberg KH, Andrews LB, Kahn MJE, Collins FS . Genetic discrimination and health insurance: an urgent need for reform. Science 1995; 270: 391–393.
Mehlman MJ, Kodish ED, Whitehouse P, Zinn AB, Sollito S, Berger J, et al. The need for anonymous genetic counseling and testing. Am J Med Genet 1996; 58: 393–397.
Lapham EV, Kozma C, Weiss J . Genetic discrimination: perspective of consumers. Science 1996; 274: 621–624.
Clayton E . Ethical, legal, and social implications of genomic medicine. N Engl J Med 2003; 349: 562–69.
Fries MH, Murphy KM, Flanagan J, Nunes M, McClellan D, Bartholomew D . Patient indications for mutation testing after referral for genetic counseling for breast/ ovarian cancer. Am J Hum Genet 1997; 61: A384.
Kash KM, Holland JC, Halper MS, Miller DG . Psychological distress and surveillance behaviors of women with a family history of breast cancer. J Natl Cancer Inst 1992; 84: 24–30.
Donovan KA, Tucker DC . Knowledge about genetic risk for breast cancer and perceptions of genetic testing in a sociodemographically diverse sample. J Behav Med 2000; 23: 15–36.
Lerman C, Daly M, Masny A, Balshem A . Attitudes about genetic testing for breast ovarian cancer susceptibility. J Clin Oncol 1994; 12: 843–850.
Bratt O, Damber J-E, Emanuelsson M, Kristoffersson U, Lundgren R, Olsson H, et al. Risk perception, screening practice and interest in genetic testing among unaffected men in families with hereditary prostate cancer. Eur J Cancer 2000; 36: 235–241.
Kinney AY, Choi Y-A, DeVellis B, KobetzE, Millikan RC, Sandler RS . Interest in genetic testing among first-degree relatives of colorectal cancer patients. Prev Med 2000; 18: 249–252.
Chaliki H, Loader S, Levenkron J, Logan-Young W, Hall J, Rowley P . Womens receptivity to testing for a genetic susceptibility to breast cancer. Am J Pub Health 1995; 85: 1133–1135.
Tambor E, Bernhardt B, Chase G, Faden R, Geller G, Hofman K, Holtzman N . Offering cystic fibrosis carrier screening to an HMO population: factors associated with utilization. Am J Hum Genet 1994; 55: 626–637.
Brantly M . Laboratory diagnosis of alpha1AT deficiency. In: RG C, ed. Alpha1-Antitrypsin Deficiency. Vol 88. New York: Marcel Dekker, Inc., 1996; 211–226.
Porter S, Jackson K, Trosclair A, Pederson LL . Prevalence of current cigarette smoking among adults and changes in prevalence of current and some day smoking: United States, 1996-2001. MMWR 2003; 52: 303–307.
McElvaney NG, Stoller JK, Buist AS, Prakash UB, Brantly ML, Schluchter MD, et al. Alpha-1 Antitrypsin Deficiency Registry Study Group. Baseline characteristics of enrollees in the National Heart, Lung and Blood Institute registry of alpha 1-antitrypsin deficiency. Chest 1997; 111: 394–403.
Thelin T, Sveger T, McNeil TF . Primary prevention in a high risk group: smoking habits in adolescents with homozygous alpha-1 antitrypsin deficiency. Acta Paediatr 1996; 85: 1207–1212.
Bloch M, Fahy M, Fox S, Hayden MR . Predictive testing for Huntingtons disease: II. Demographic characteristics, life-style patterns, attitudes, and psychosocial assessments of the first fifty-one test candidates. Am J Med Genet 1989; 48: 217–224.
Silverman HJ, DeRenzo E, deSerres FJ, Everett SE, Fallat RJ, Mullins CD, et al. Genetic testing for alpha-1 antitrypsin deficiency: ethical, legal, psychologic, social, and economic issues. Am J Respir Crit Care Med 2003; 168: 874–896.
Cella D, Hughes C, Peterman A, Chang C-H, Peshkin BN, Schwartz MD, et al. A brief assessment of concerns associated with genetic testing for cancer: the multidimensional impact of cancer risk assessment (MICRA) questionnaire. Health Psychology 2002; 21: 564–572.
Knebel AR, Leidy NK, Sherman S . Health related quality of life and disease severity in patients with alpha-1 antitrypsin deficiency. Qual Life Res 1999; 8: 385–391.
Acknowledgements
The authors extend their appreciation for funding to the Alpha-1 Foundation and to Kathy Valenti, Marc Yarborough, and Ann Knebel who assisted in study design.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Strange, C., Dickson, R., Carter, C. et al. Genetic testing for Alpha1-antitrypsin deficiency. Genet Med 6, 204–210 (2004). https://doi.org/10.1097/01.GIM.0000132669.09819.79
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/01.GIM.0000132669.09819.79
Keywords
This article is cited by
-
Relationship between alpha-1 antitrypsin deficiency and obstructive sleep apnea
Sleep and Breathing (2021)
-
Detection of alpha-1 antitrypsin deficiency: the past, present and future
Orphanet Journal of Rare Diseases (2020)
-
Alpha-1 Antitrypsin Deficiency and Accelerated Aging: A New Model for an Old Disease?
Drugs & Aging (2019)
-
α1-Antitrypsin deficiency
Nature Reviews Disease Primers (2016)
-
The Alpha‐1 Association Genetic Counseling Program: An Innovative Approach to Service
Journal of Genetic Counseling (2011)