Abstract
Purpose
The aim of this study is to assess the importance of magnetic resonance imaging (MRI) before surgery in highly myopic patients, evaluating the capability of imaging to identify muscles displacement and orbital pulley abnormalities and their role in the pathogenesis of heavy eye syndrome (HES).
Methods
We reviewed the medical records and high-resolution orbital MRIs of highly myopic adults with HES, who underwent surgery for strabismus at the Sant’Orsola-Malpighi University Hospital of Bologna from January 2007 to June 2016. The measure of the angle of dislocation between lateral rectus and superior rectus and lateral rectus–superior rectus band (LR–SR band) were evaluated on coronal MRI imaging.
Results
A total of 54 patients with HES were evaluated by MRI. Mean axial length was 30.5±3 mm. Mean distance esotropia was 49.2±14.4 prism diopters (PD) and the mean hypotropia was 4.3±4.4 PD. All subjects exhibited severe superotemporal globe prolapse that displaced the lateral rectus inferiorly and the superior rectus muscle medially with mean angle of dislocation of 167.5±12.9° on MRI. The LR–SR band was thinned in 56 eyes, ruptured in 8 and not evaluable in 1 case.
Conclusions
In our study, we detected muscles displacement in all subjects and we discovered alteration of the LR–SR band in patients with HES, suggesting a possible role in the pathogenesis of this disease. The evaluation of preoperative orbital MRI imaging in patients with highly myopic strabismus is helpful to detect different anatomical etiology and eventually to drive the choice of appropriate surgery.
Similar content being viewed by others
Introduction
Highly myopic patients can develop a form of strabismus named myopic strabismus fixus or heavy eye syndrome (HES). The term ‘heavy eye’ was used to convey the impression that the larger, or heavier, myopic eye resulted in a drop of its anterior half. These patients classically present a progressive esotropia and often hypotropia with limited abduction and elevation.1
In 1969 Hugonnier et Magnard were the first to report clinical features of this condition, suggesting a correlation with structural changes in the ocular muscle like the presence of fibrous tissue in the lateral rectus.2 Over the years, many pathogenetic hypotheses have been presented.
Bagolini et al suggested that the cause of the myopathy affecting the lateral rectus muscles was a progressive compression of the muscle against the lateral orbital wall.3 Demer and Von Noorden, using magnetic resonance imaging (MRI) showed a mechanical restriction with a contact between the posterior portion of the globe and the bones of the orbital apex.4
Krzizok et al suggested that the progressive prolapse of the posterior portion of the eyeball to the superotemporal quadrant of the orbit, outside the tissue with support function (pulley) and the muscular cone is the cause of the strabismus.5 According to this theory, Yokoyama and colleagues obtained satisfactory surgical correction by suture anastomosis of the posterior bellies of the lateral rectus and the superior rectus muscle to normalize the relative position of the dislocated myopic eye.6
In recent years, MRI has been used more and more in clinical diagnosis of different ocular motor disorders, like HES. High-resolution MRI with surface coil was essential to demonstrate etiology and suggest surgical treatment in this pathology.
The purpose of this study is to evaluate the importance of performing MRI before surgery in highly myopic patients, considering the role of MRI to identify a displacement of extraocular muscles and orbital pulley abnormalities and their role in the pathogenesis of HES.
Materials and methods
We reviewed the medical records and high-resolution orbital MRIs of highly myopic adults with HES, who underwent surgery for strabismus at the Sant’Orsola-Malpighi University Hospital of Bologna, Italy, from January 2007 to June 2016.
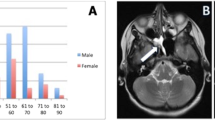
A total of 54 patients (65 eyes), 42 females and 12 males, were enrolled. Their mean age was 52.3±13.4 years, going from 31 to 80 years. Those with a history of childhood strabismus, strabismus surgery, and other possible causes of ocular movement limitation, such as retinal detachment surgery, abducens nerve palsy and Duane’s retraction syndrome, were excluded.
All subjects underwent visual acuity assessment, motility examination, slit-lamp and dilated fundus examination, cycloplegic refraction and photography of ocular versions. Ideally, measurements of the angle of deviation were obtained using prisms bars and alternating cover test at 5 and 0.33 m; however, when this proved impossible, Krimsky’s test was used. A Goldman perimeter was used to measure the maximal abduction, that is, the excursion expressed in degrees the eye is able to perform from the primary position to the position of maximum abduction. We measured the ocular axis five times in each eye using A mode echography (Carl Zeiss IOL Master; Jena, Germany).
High-resolution T1-or T2-weighted MRI was performed using a 1.5T scanner (Signa; General Electric, Milwaukee, WI) preoperatively in all patients to evaluate dislocation angle measurement. For dislocation angle measurement, the coordinates of the area centroids of the lateral rectus muscle and the superior rectus muscle globe were measured by use of Image J, public domain software available on the Internet (http://rsbweb.nih.gov/ij/), and the dislocation angle was defined as the angle formed by these and the centroid of the globe, in accordance with the method of Yokoyama et al6, 7 (Figure 1).
As suggested by Rutar, the lateral rectus–superior rectus band (LR–SR band) was qualitatively assessed as robust, thinner or ruptured by examining adjacent quasicoronal image planes (Table 1).8
The study adhered to the tenets of the Declaration of Helsinki.
Results
Around 43 of 54 patients had unilateral strabismus and 11 had bilateral strabismus. All our subjects presented esotropia with or without hypotropia, accompanied by limited abduction and/or supraduction. Mean distance esotropia was 49.2±14.4 prism diopters (PD) and the mean hypotropia was 4.3±4.4 DP. High myopia was defined as an ocular axial length of ≥27 mm or as refractive values >−6 diopters (D). Mean axial length was 30.5±3 mm. Refractive values are not shown, because six eyes already had undergone cataract surgery.
All subjects exhibited severe superotemporal globe prolapse that displaced the lateral rectus inferiorly and the superior rectus muscle medially on MRI (Figure 2). The mean angle of dislocation was 167.5±12.9°.
(a) Preoperative pictures of the eyes in all gaze directions in a 58-years-old woman with bilateral Heavy Eye Syndrome. (b) Coronal MRI section of the same patient revealed a dislocation angles of 190° OD and 202° OS, nasal displacement of the bilateral superior rectus muscles and inferior displacement of the bilateral lateral rectus muscles.
The LR–SR band was thinned in 56 orbits and ruptured in 8 (Figure 3). Only in one case it was not possible to determine the LR–SR band for poor quality imaging.
Discussion
MRI provides high soft tissue contrast long with high spatial resolution achievable in multiple planes giving excellent anatomic detail of the visual pathways, the globe and soft tissues. T1 weighted images of dark muscle are satisfactory for viewing the extraocular muscles.
Restrictive ocular motility disturbances associated with high myopia have been described via the use of computed tomography and MRI;9 in particular, MRI plays now an important role in assessing HES.
In highly myopic eye with HES it is possible to demonstrate, on coronal MRI image just posterior to the equator, the inferior and medial displacement respectively of the lateral rectus and superior rectus with severe superotemporal prolapse of the myopic globe. As a consequence of this abnormal eye position, eye movements are limited in abduction and supraduction, which are general characteristic of this disease.4 Currently, this is the most accepted theory supported not only by imaging but also by surgical feedback.9, 10, 11, 12, 13
In our study, we detected muscle displacement in all subjects, confirming previous data.
Notably, we measured a mean angle of dislocation of eye with this disease of 167.5±12.9°. However, Kohmoto et al reported a dislocation angle of 113±9.7°, similar to Nakao et al with dislocation angle of 132±14°.14, 15 These different values between our study and the previous ones may be attributed to the inclusion of mild-moderate case in previous studies, and the inclusion of many severe cases of strabismus fixus in our study. In fact, our data are similar to those reported by Yamaguchi et al with a dislocation angle of 184±3.5°.7
Even if the muscles displacement is a well-recognized cause of strabismus in HES, clear explanations on how it happens have still not been provided.
Two major anatomic mechanisms have been proposed for this disease, and no consensus has been reached. One is Yokoyama’s theory, in which the disease is caused by dislocation of the posterior globe from the muscle cone because of globe elongation. On the basis of this theory, severe cases with a fixed eye position can be explained, but explanation of mild cases with relatively mild limitation of eye movement is difficult.6, 7
The other is Demer’s theory, in which degeneration of the LR–SR band is particularly marked in eyes with highly myopic strabismus, and this degeneration causes displacement of the rectus muscles, inducing eye position abnormalities.8, 16, 17 According to this theory, mild cases can be understood, but explanation of severe cases is difficult.
Recently, Nakao et al evaluated orbital pulley abnormalities in patients with highly myopic strabismus, suggesting to consider both theories to explain HES.15
Our study is the first with such as large number of patients with HES, in which MRI was performed. We detected in all eyes thinning or a rupture of the LR–SR band, confirming a role of connective tissue in the pathogenesis of this disease. However, it is not possible to determine if the degeneration of the LR–SR band is the first cause or the final stage of HES. Only a further prospective study in highly myopic patients could clarify this issue.
Anyhow, the evaluation of LR–SR band on MRI image is important to differentiate HES from sagging eye syndrome (SES). SES is a similar condition occurring in nonmyopic ederly patients, in which individuals develop esotropia for distance viewing and/or small-angle hypotropia with decreased supraduction but full abduction. In these patients imaging demonstrated that the LR–SR band degenerates during aging, producing inferior displacement of the pulley. While differential diagnosis is clear in absence of refractive error, the evaluation could be difficult in patient with high myopia.
Recently, Tan et al underline the importance of orbital MRI in differentiating SES from HES in patients with high myopia.18 They suggest that in HES on Orbital MRI there is an inferior lateral rectus displacement and medial superior rectus displacement with severe superotemporal prolapse of the myopic globe, whereas only inferior displacement of the lateral rectus results from degeneration of the LR–SR band is seen in SES.18 Our study confirms this theory: in fact, we evaluated a greater angle of displacement in patients with HES. It is possible that the patient group over 60 could be contaminated by age related issues, but it is noteworthy that the features of different age groups are homogeneous. This could suggest that the LR–SR band degeneration in our study is related to HES and not to only aging degeneration.
The authors declare no conflict of interest.The assessment of these anatomical findings can also provide information to drive the choice of appropriate surgery. While HES responds to surgical union of the superior rectus and lateral rectus muscle bellies, an augmented medial rectus muscle recession seems to be appropriate for highly myopic patients with SES.19
The authors declare no conflict of interest.Limitations of our study lie in its retrospective nature and in the only preoperative evaluation of patients, but it also provides important information for understanding the pathophysiology of this disease.
In conclusion, we recommend performing preoperative orbital MRI imaging routinely in patients with highly myopic strabismus and evaluating its features, in particular, muscles displacement and LR–SR degeneration. This will be helpful to better clarify the etiology of this disease and eventually drive the choice of appropriate surgery.

References
Taylor R, Whale K, Raines M . The heavy eye phenomenon: orthoptic and ophthalmic characteristics. Ger J Ophthalmol 1995; 4: 252–255.
Hugonnier R, Magnard P . Les desequilibres oculo-moteurs observès en cas de myopie forte. Ann Oculist 1969; 202: 713–724.
Bagolini B, Tamburrelli C, Dickmann A, Colosimo C . Convergent strabismus fixus in high myopic patients. Doc Ophthalmol 1990; 74: 309–320.
Demer JL, vonNoorden GK . High myopia as an unusual causeo frestrictive motility disturbance. Surv Ophthalmol 1989; 22: 281–284.
Krizizok TH, Kaufmann H, Traupe H . Elucidation of restrictive motility in high myopia by magnetic resonance imagine. Arch Ophthalmol 1997; 115: 1019–1027.
Yokoyama T, Tabuchi H, Ataka S, Shiraki K, Miki T, Mochizuki K . The mechanism of development in progressive esotropia with high myopia. In: de Faber JT ed. Transactions of the 26th Meeting of European Strabismological Association. Barcelona, Spain. Swets & Zeitlinger Publishers: Lisse, The Netherlands, 2000; 218–221.
Yamaguchi M, Yokoyama T, Shiraki K . Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol 2010; 149: 341–346.
Rutar T, Demer JL . ‘Heavy Eye’ syndrome in the absence of high myopia. A connective tissue degeneration in elderly strabismic patients. J AAPOS 2009; 13: 36–44.
Kaynak S, Durak I, Canda T . Restrictive myopic myopathy: computed tomography, magnetic resonance imaging, echography, and histological findings. Br J Ophthalmol 1994; 78: 414–415.
Aoki Y, Nishida Y, Hayashi O, Nakamura J, Oda S, Yamade S et al. Magnetic resonance imaging measurements of extraocular muscle path shift and posterior eyeball prolapse from the muscle cone in acquired esotropia with high myopia. Am J Ophthalmol 2003; 136: 482–489.
Fresina M, Finzi A, Versura, Campos EC . Muscle belly union associated with simultaneous medial rectus recession for treatment of myopic myopathy: results in 33 eyes. Eye 2014; 28: 557–561.
Ahadzadeghan I, Akbari MR, Ameri A, Anvari F, Jafari AK, Rajabi MT . Muscle belly union for treatment of myopic strabismus fixus. Strabismus 2009; 17 (2): 57–62.
Godeiro KD, Kirsch D, Tabuse MK, Cronemberger M . Yamada’s surgery for treatment of myopic strabismus fixus. Int Ophthalmol 2009; 29: 305–308.
Kohmoto H, Inoue K, Wakakura M . Divergence insufficiency associated with high myopia. Clin Ophyhalmol 2010; 5: 11–16.
Nakao Y, Kimura T . Prevalence and anatomic mechanism of highly myopic strabismus among Japanese with severe myopia. Jpn J Ophthalmol 2014; 58: 218–224.
Kono R, Poukens V, Demer JL . Quantitative analysis of the structure of the human extraocular muscle pulley system. Invest Ophthalmol Vis Sci 2002; 43: 2923–2932.
Clark RA, Demer JL . Effect of aging on human rectus extraocular muscle paths demonstrated by magnetic resonance imaging. Am J Ophthalmol 2002; 134: 872–878.
Tan RJD, Demer JL . Heavy eye syndrome versus sagging eye syndrome in high myopia. J AAPOS 2015; 19: 500–506.
Yamada M, Taniguchi S, Muroi T . Rectus eye muscle paths after surgical correction of convergent strabismus fixus. Am J Ophthalmol 2002; 134: 630–632.
Acknowledgements
This study was performed in the Ophthalmology Unit, S. Orsola-Malpighi Hospital, University of Bologna, Bologna, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Maiolo, C., Fresina, M. & Campos, E. Role of magnetic resonance imaging in heavy eye syndrome. Eye 31, 1163–1167 (2017). https://doi.org/10.1038/eye.2017.48
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.48
This article is cited by
-
Inferior rectus displacement in heavy eye syndrome and sagging eye syndrome
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)