Abstract
Purpose
To describe a novel use of fibrin glue in managing leaking blebs and leaking wounds following trauma or surgery.
Methods
Interventional case series.
Results
We report eight patients, including three where intra-operative or immediate post-penetrating keratoplasty recalcitrant leaks from the graft–host junction and/or openings created by the needle pass, were noted. All three had thin recipient beds in the sector of leak. This was managed by intra-cameral injection of fibrin glue in the affected quadrant. This stopped the leak and allowed the defect to heal. One patient of Descemets-stripping-endothelial-keratoplasty had leak from the surgical wound, which was also sealed with fibrin glue. Two patients with leaking glaucoma-surgery-related blebs were treated with intra-bleb injection of fibrin glue to stop the leak. One patient with a penetrating corneal injury with a metal wire had a brisk leak upon removal of the wire. This was sealed with fibrin glue. Another patient of chemical burn with spontaneous leaks was managed by glue injection in the perforations. Transient rise of intraocular pressure in one patient with a leaking bleb was the only adverse event recorded.
Conclusion
This novel adaptation of the application of fibrin glue can help to deal with persistent intra-operative, post-operative and traumatic aqueous and air leaks.
Similar content being viewed by others
Introduction
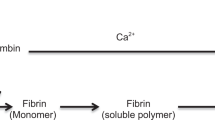
Fibrin glue consists of fibrinogen and thrombin. Fibrin is polymerised to form a haemostatic network and permits tissue adhesion. Commercially available fibrin glue (Tisseel, Baxter AG, Vienna, Austria) contains aprotinin, which is an antifibrinolytic agent that maintains the sealant effect for longer.
Fibrin glue has been used for pterygium excision, sealing scleral flaps after hypotony in glaucoma surgeries,1 conjunctival closure in trabeculectomy,2 repair of Ahmed valve tube exposure,3 buttonhole flap defect after LASIK,4 to attach the recessed peritomised conjunctiva in limbal stem cell transplantation where it also acts as a physical barrier to conjunctival cell migration,5 perforated corneal ulcers,6 open globe injury,7 and in deep anterior lamellar keratoplasty.8
Technique
For leaks with penetrating keratoplasty a 28 G blunt tipped cannula was attached to the double barrelled syringe of fibrin glue. The cannula was charged with the glue to expel air and the tip inserted through the graft–host junction into the AC. Glue was injected in the AC under the leaking site and in the graft–host junction while withdrawing the cannula. The total volume injected was up to 0.1 ml.
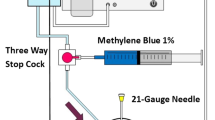
For leaking filtering blebs, a 30 G sharp needle was attached to the syringe, the needle was charged with glue and, at the slit lamp under topical anaesthesia, the conjunctiva adjacent to the bleb was pierced and the needle was advanced in a zig-zag manner to enter the bleb close to the leaking site. 0.1 to 0.2 ml of fibrin glue was injected in the bleb. In the patient with an Ahmed valve, some glue was seen to extrude from the leaking site.
In the patient with the corneal foreign body, there was profuse leakage from the track in the cornea with collapse of the AC. The AC was reformed by injecting balanced salt solution through the wound, a paracentesis was performed and fibrin glue was then similarly injected using a 28 G cannula as described for corneal grafts. This did not stop the leak, hence the two components of the glue (fibrinogen and thrombin solutions) were drawn separately in to 1 ml syringes. With a 30 G needle the more viscous fibrinogen component was injected first in the track followed by the thinner thrombin solution. The succeeded in arresting the leak. A bandage contact lens was applied. The total volume injected was less than 0.1 ml (Supplementary Videos 1 and 2).
Case reports
Case 1
A 35-year-old lady with chronic herpes simplex keratitis had undergone a penetrating keratoplasty (PK) 1 year prior to presentation. The graft was scarred and vascularised secondary to a bacterial infection (Figure 1a). She underwent fine needle diathermy occlusion of the vessels and a repeat PK. On day one post-operative there was aqueous leakage from the graft–host (G–H) junction in the inferonasal quadrant. Placement of additional sutures and a bandage contact lens did not stop the leak due to the disparity in the graft–host bed thickness and leakage from suture tracks (Figure 1b). Fibrin glue was injected in the anterior chamber (AC) through the G–H junction. Excess glue on the surface was excised. The leak had stopped immediately (Figure 1c) and the AC re-formed and maintained over the follow-up period of 6 months.
(a) Clinical photograph of left eye showing the scarred and vascularised graft due to a bacterial infection. (b) Photograph of the additional sutures placed in the inferonasal quadrant (arrow) after repeating the penetrating keratoplasty. (c) Cobalt-blue light picture after the injection of fibrin glue in the anterior chamber at the G–H junction, showing the arrest of leakage (asterisk).
Case 2
A 43-year-old female had considerable G–H thickness disparity related to previous undetermined corneal scarring. Intraoperatively, despite additional sutures, there was leak of aqueous humour from the G–H junction and from the 3 suture tracks. Fibrin glue was injected in the area of leakage inside the AC, but spread to the entire corresponding quadrant. The leakage stopped. There was residual fibrin visible during two weeks post-operative but had completely dissolved at one month with no leak.
Case 3
A 77-year-old lady with anterior segment dysgenesis had multiple surgeries as a child leaving her with a very thin conjunctivalised superior cornea. She underwent a PK for corneal decompensation with scarring. On the first post-op day a leak was seen superiorly with a shallow AC. During attempted re-suturing of the G–H junction two distinct holes appeared in the host rim at the site of needle pass (Figure 2a). The sutures were removed and the G–H junction and holes sealed with fibrin glue injected in the AC superiorly. The leak stopped and the AC remained formed even after dissolution of the fibrin glue (Figure 2b).
Case 4
An 82-year-old lady with previous PK and pseudophakia underwent an Ahmed valve procedure for uncontrolled glaucoma. Three weeks post-operative she presented with hypotony and a brisk leak from the bleb suture line. The conjunctiva and Tenon’s capsule were re-sutured but at the one-week follow-up the leak persisted. At the slit lamp, fibrin glue was injected in the bleb. The leak stopped and at subsequent follow-up visits remained so without compromising the intraocular pressure.
Case 5
A 73-year-old man had a five year history of a functioning bleb following trabeculectomy. On a routine follow-up visit the bleb was Seidel positive in an area of very thin conjunctiva. Intra-bleb injection of autologous blood or fibrin glue were considered but the latter option was performed. The leak stopped and remained so. There was a transient rise of pressure (26 mm Hg), which had settled (18 mm Hg) at 6-week follow-up.
Case 6
A 48-year-old man presented with history of a foreign body in the right eye while polishing metal with a wire brush. A piece of wire had penetrated the cornea with less than a millimetre protruding outside the surface. The other end was just anterior to the iris, traversing the anterior chamber, which was formed. There was no leak (Figures 3a and b). Under the operating microscope (yellow light filter) with topical anaesthesia the protruding end of the foreign body (wire) was grasped firmly with a Hoskins tissue forceps and pulled swiftly out in one motion. It was feared that a collapse of the anterior chamber would risk the tip penetrating the iris and puncturing the anterior lens capsule. There was brisk leak from the track in the cornea. This was sealed by injecting fibrin glue in the track with a small amount entering the anterior chamber.
(a) Clinical picture, front view of right cornea showing the tip of the metallic (wire) foreign body (FB) (arrow). (b) Clinical picture, side view showing the wire FB traversing the length of the anterior chamber (white arrow=anterior end, black outlined arrow=posterior end). The posterior end of the FB is almost touching the surface of the iris. (c) Fluorescein instillation did not show any leak (Sidel negative).
Case 7
A 78-year-old woman underwent Descemets-stripping-endothelial-keratoplasty. On day 1 postoperatively the air had escaped under the conjunctiva. Exploration of the wound showed air leak, which was not stopped by placement of additional sutures. Fibrin glue was injected in the anterior chamber in the quadrant adjacent to the wound and in the lips of the wound. This stopped the leak and allowed the AC to be filled with air to support the DSEK graft, which attached successfully (Supplementary Video 1).
Case 8
A 56-year-old man presented with total limbal stem cell deficiency following chemical burn 4 years ago. The peripheral cornea in the inferonasal quadrant was very thin and showed to points of brisk leak. These were managed with cyanoacrylate glue application, which did not work. Subsequently the fibrovascular pannus at the leaking site was removed and the perforations were sealed by injecting fibrin glue through the holes in to the corresponding quadrant of the anterior chamber. The leak stopped immediately. The thin area was re-enforced with a 5 mm lamellar corneal patch graft, which was also attached with fibrin glue (Supplementary Video 2).
Discussion
In the four patients where fibrin glue was injected in the AC the glue served the purpose of arresting the leak which remained closed even after the glue had absorbed. There was no untoward reaction in the eye or on the corneal endothelium. A plasmoid aqueous with a frank fibrin clot is known to develop spontaneously in cases of acute iritis and keratitis.9 The clot resolves over time with no adverse effect. It is likely that injected glue behaves in a similar manner though there is a definite risk of raised pressure and allergic reactions to the components of the glue. Fibrin glue should be avoided in individuals with known allergy to bovine proteins or to aprotinin.10
In the two glaucoma-surgery-related bleb leaks, the glue was injected in the cavity of the bleb. The principle is the same as in use of autologous blood for sealing bleb leaks.11 The scaffold provided by fibrin that bridges across the perforation, whether in the bleb or cornea, would allow fibroblasts to migrate across the defect and lay down collagen of wound healing to permanently close the site.
In the case with a metal wire impaled in the cornea, an initial paracentesis was avoided because of the risk of damage to the iris and lens by sudden shallowing of the AC. The brisk leak from the track in the cornea caused the AC to collapse and was unlikely to seal spontaneously. This was successfully sealed by the injection of fibrin glue. The DSEK case was unique in that air injected in the AC to support the graft against the recipient cornea was leaking through the wound. This caused the graft to detach. The wound was successfully closed with fibrin glue, which enabled the AC to be filled with air and attach the graft.
These cases illustrate that in difficult situations, following trauma, intraoperatively and as complications of surgery, fibrin glue can be a useful option to consider. However, as this report includes only a small number of cases, the technique should be used with caution and after other more simple interventions have been tried.

References
Bahar I, Lusky M, Gaton D, Robinson A, Avisar R, Weinberger D . The use of fibrin adhesive in trabeculectomy: a pilot study. Br J Ophthalmol 2006; 90 (11): 1430.
Martinez-de-la-Casa JM, Rayward O, Saenz-Frances F, Mendez C, Bueso ES, Garcia-Feijoo J . Use of a fibrin adhesive for conjunctival closure in trabeculectomy. Acta Ophthalmol 2013; 91: 425–428.
Choudhari NS, Neog A, Latka S, Srinivasan B . Fibrin sealant-assisted revision of the exposed ahmed tube. Middle East Afr J Ophthalmol 2015; 22 (1): 115–116.
He L, Manche EE . Fibrin glue for prevention of recurrent epithelial ingrowth under a LASIK flap with a central buttonhole defect. J Cataract Refr Surg 2012; 38 (10): 1857–1860.
Yeung AM, Faraj LA, McIntosh OD, Dhillon VK, Dua HS . Fibrin glue inhibits migration of ocular surface epithelial cells. Eye 2016; 30 (10): 1389–1394.
Dong N, Li C, Chen WS, Qin WJ, Xue YH, Wu HP . Fibrin glue-assisted for the treatment of corneal perforations using glycerine-cryopreserved corneal tissue. Int J Ophthalmol 2014; 7 (1): 62–65.
Kong GY, Henderson RH, Sandhu SS, Essex RW, Allen PJ, Campbell WG . Wound-related complications and clinical outcomes following open globe injury repair. Clin Exp Ophthalmol 2015; 43 (6): 508–513.
Por YM, Tan YL, Mehta JS, Tan DT . Intracameral fibrin tissue sealant as an adjunct in tectonic lamellar keratoplasty for large corneal perforations. Cornea 2009; 28 (4): 451–455.
Jones N . Uveitis 2nd edn. JP Medical: London, UK, 2013; 22–23.
Pramanik J, Pramanik T, Juntang L, Zhikun G . A mini-review: aprotinin in fibrin glue-a major concern!. BMJ 1994; 308: 933.
Wise JB . Treatment of chronic postfiltration hypotony by intrableb injection of autologous blood. Arch Ophthalmol 1993; 111: 827–830.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Rights and permissions
About this article
Cite this article
Scalcione, C., Ortiz-Vaquerizas, D., Said, D. et al. Fibrin glue as agent for sealing corneal and conjunctival wound leaks. Eye 32, 463–466 (2018). https://doi.org/10.1038/eye.2017.227
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.227
This article is cited by
-
Biological Materials Introduced to the Market for Blurred Cornea Regeneration
Regenerative Engineering and Translational Medicine (2023)
-
Fibrin
Reactions Weekly (2018)