Abstract
Purpose
To investigate long-term retinal changes after microincision pars plana vitrectomy surgery (MIVS) for macular hole (MH) in retinitis pigmentosa (RP) patients—retrospective and observational study.
Methods
Three RP patients suffering from MH were evaluated by means of best corrected visual acuity, anterior and posterior binocular examination, spectralis high-resolution optical coherence tomography, MP-1 microperimetry (MP-1), and full-field electroretinogram (ERG), before MIVS and during the 36-month follow-up. Patients underwent simultaneous MIVS and microincision cataract surgery; IOL was positioned in capsular bag. Patients were hospitalised for 2 days after the surgery. Surgical procedure was performed according the following schedule: surgical removal of crystalline lens, MIVS with 23-gauge sutureless system trocars, core vitreous body removal, peeling of the inner limiting membrane, and balanced sterile saline solution-air-micro-structured polydimethylsiloxane (PDMS) exchange. PDMS tamponade, after 6 months starting from MIVS, was removed.
Results
In all patients visual acuity increased after vitrectomy as a consequence of complete MH closure and restoration of retinal architecture. None of the patients developed ocular hypertension, or re-opening of MH during the 3-year follow-up. MP-1 bivariate contour ellipse area was reduced in its dimensions and improved in all patients demonstrating a better fixation.
Conclusions
MIVS could be an effective treatment in RP patients with MH if medical therapy is not applicable or not sufficient. Finally more studies will be needed to improve knowledge about this genetic disease.
Similar content being viewed by others
Introduction
Retinitis pigmentosa (RP) includes a wide group of different degenerative diseases of the outer retina caused by gene abnormalities on several chromosomes and that leads to legal blindness in 1/4000.1 An estimated 1.5 million people are affected around the world. Some patients become blind as early as age 30; the majority of the patients are legally blind by age 60 with a central visual field diameter <20 degrees.1, 2, 3 The outer segment of photoreceptors are usually damaged in very early stage of the disease, while the macula appears spared from the degenerative process for a long time.2 Frequently the presence of liquid leakage from retinal capillaries4 causes cystoid macular oedema (CME) and/or cells migration in the vitreous body.5
Oishi et al6 classified the status of the inner segment/outer segment junction (IS/OS) as being absent, discontinuous, or distinct. As a consequence of chronic blood retinal barrier breakdown, which is reported to occur in 8–50% of the instances, the inner surface of the retina may present irregularities of the inner limiting membrane (ILM) or iperreflectivity of vitreoretinal interface.4, 5 Macular cysts tend to be confluent in some cases and, in combination with ILM wrinkling, sometimes may lead to the formation of macular hole (MH) encompassing different stages (from I to IV according to Gass classification), that in RP patients is present in 4–8% of eyes with different shapes and gradation.5 Consequently few reports of MH surgical treatment in RP patients are present in the literature and usually involve small number of eyes treated with pars plana vitrectomy.7, 8
The purpose of this study was to evaluate the morphological and functional outcomes of microincision pars plana vitrectomy surgery (MIVS) associated to ILM peeling technique in RP patients with MH when medical therapy is not applicable or not effective.
Methods
The clinical charts of 3 RP patients suffering from MH secondary to chronic CME and tangential vitreoretinal tractions, who underwent 23-gauge MIVS (ACCURUS vitrectomy system ALCON Inc., Irvine, CA, USA) were evaluated retrospectively (Tables 1 and 2). These patients were unresponsive to conventional medical treatment based on carbonic anhydride inhibitors and non-steroidal anti-inflammatory drugs or steroids.
Surgical procedure was performed with a three-port pars plana vitrectomy, peeling of the ILM, and simultaneous cataract surgery by the same surgeon (EMV) under retrobulbar anaesthesia (Table 3). Betamethasone 0.1% eye drops were instilled for 10 days, followed by fluorometholone 0.1% for several weeks. After 6 months starting from MIVS, polydimethylsiloxane (PDMS) was removed. Patients were followed up for 36 months.
Patient G
A 34-year-old male suffering from RP since the age of 14. Baseline best corrected visual acuity (BCVA) was 6/20 Snellen in the right eye. Slit lamp examination only revealed a posterior subcapsular cataract. In addition, spectral-domain optical coherence tomography (SD-OCT) demonstrated partial thickness MH and MP-1 reported a parafoveal fixation area with bivariate contour ellipse area (BCEA) of 0.42 degrees.
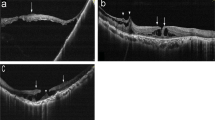
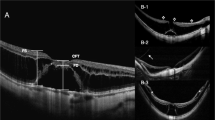
Due to the presence of MH (grade III/IV according to Gass classification), central retinal thickness was not considered, while parafoveal retinal thickness was 451 μm (Figure 1a). After vitrectomy, BCVA increased to 10/20 Snellen. SD-OCT showed a considerable reduction in parafoveal retinal thickness, and demonstrated a central retinal thickness of 295 μm (Figure 1b). BCEA decreased to a final value of 0.28 degrees.
Retinitis pigmentosa (RP) in G.O. patient. (a) Macular hole (MH) grade III/IV, according to Gass classification, as shown by spectral-domain optical coherence tomography (SD-OCT) before surgery. Parafoveal retinal thickness was 451 μm. (b) After surgery, the MH closed and the central retinal thickness was 295 μm.
Patient A
A 49-year-old male suffering from RP since the age 17. Baseline BCVA was 8/20 Snellen in the left eye. Nuclear and posterior subcapsular cataract was present at slit lamp examination. A partial thickness MH (grade II/III according to Gass classification) was demonstrated by SD-OCT. MP-1 reported a parafoveal fixation area with BCEA of 0.54 degrees at baseline. The parafoveal retina measured 350 μm in thickness. Postoperative VA increased to 14/20 Snellen. Central retinal thickness was 278 μm. BCEA after MH resolution was of 0.25 degrees.
Patient T
A 37-year-old woman with diagnosis of Usher syndrome. Baseline BCVA was 2/20 Snellen in the right eye. Posterior subcapsular cataract was observed biomicroscopically. SD-OCT showed a full thickness MH. A parafoveal fixation area with BCEA of 1.34 degrees at baseline was demonstrated with MP-1. Parafoveal retinal thickness was 440 μm. Postoperatively, VA increased to 4/20 Snellen. SD-OCT showed a reduction in parafoveal retinal thickness, and a central retinal thickness of 290 μm. BCEA decreased to 0.98 degrees.
Discussion
MH in RP patients is caused by chronic CME, incomplete vitreous detachment, and traction of condensed vitreous strands.7, 8 In exceptional cases, spontaneous resolution of a full thickness MH may occur.8, 9
Complete MH closure and restoration of retinal architecture in our patients lead to increased VA postoperatively and reduced BCEA with better fixation (Figure 1a and b).
Likewise an interesting study of Mahmoud et al10 showed that a combined lensectomy and vitrectomy procedure in P347L transgenic pigs was associated with retention of a significantly greater number of outer nuclear layer nuclei than in unoperated fellow eyes. Authors stated that consistent with the results obtained from other studies, the preservation of photoreceptors after surgery may be explained by the action of some diffusible substances or growth factors originating from the stimulated iris, ciliary body, and the retina.11 They could be: basic fibroblast growth factor (bFGF), neurotrophic growth factor (CNTF), brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), and lens-epithelium-derived growth factor (LEGF).11, 12, 13
Moreover, Mahomoud et al10 and Schori et al14 showed that an autoimmune response by lymphocytes and cytokines may be involved in the rescue process of retinal cells degeneration 8 weeks after surgery.
On the other hand, the development of narrow-gauge transconjunctival vitrectomy systems has improved the visual recovery following surgery. We think that, at this stage in our knowledge, removal of any vitreomacular traction with peeling of the ILM is probably the main reason for visual improvement and better fixation postoperatively. Recently Ocriplasmin, by degrading laminin and fibronectin at the vitreoretinal interface, may allow induction of posterior vitreous detachment in a non-invasive manner.
Furthermore, additional research is still needed for the greater understanding of the pathophysiology underlying the development of vitreomacular traction and idiopathic MH in RP patients too.15, 16 Even if the present report is on few patients, our limited experience suggests that MIVS could be an effective therapy for MH in tapetoretinal dystrophies, and according to Sandeep et al8, 17, 18, 19, 20 PDMS could be useful compared with air-gas tamponade since RP patients have visual field restriction that can cause movement and posture problems thus facilitating a recurrence of the disease. However, further evidence may be needed to confirm our preliminary findings.

References
Berson EL . Retinitis pigmentosa. The Friedenwald lecture. Invest Ophthalmol Vis Sci 1993; 34 (5): 1659–1676.
Grover S, Fishman GA, Anderson RJ, Alexander KR, Derlacki DJ . Rate of visual field loss in retinitis pigmentosa. Ophthalmology 1997; 104: 460–465.
Vingolo EM, Salvatore S, Belcaro G, Nebbioso M . Reduced retinal sensitivity and stereopsis in retinitis pigmentosa. Panminerva Med 2014; 56 (S2): 29–32.
Hajali M, Fishman GA, Anderson RJ . The prevalence of cystoid macular oedema in retinitis pigmentosa patients determined by optical coherence tomography. Br J Ophthalmol 2008; 92: 1065–1068.
Takezawa M, Tetsuka A . Tangential vitreous traction: a possible mechanism of development of cystoids macular edema in retinitis pigmentosa. Clin Ophthalmol 2011; 5: 245–248.
Oishi A, Otani A, Sasahara M, Kojima H, Nakamura H, Kurimoto M et al. Photoreceptor integrity and visual acuity in cystoid macular oedema associated with retinitis pigmentosa. Eye (Lond) 2009; 23: 1411–1416.
Hagiwara A, Yamamoto S, Ogata K, Sugawara T, Hiramatsu A, Shibata M et al. Macular abnormalities in patients with retinitis pigmentosa: prevalence on OCT examination and outcomes of vitreoretinal surgery. Acta Ophthalmol 2011; 89: e122–e125.
Jin ZB, Gan DK, Xu GZ, Nao-I N . Macular hole formation in patients with retinitis pigmentosa and prognosis of pars plana vitrectomy. Retina 2008; 28: 610–614.
Raja M, Goldsmith C, Burton BJ . Spontaneous resolution of full-thickness macular hole in retinitis pigmentosa. BMJ Case Rep 2011; 2011: bcr0320113999.
Mahomoud TH, McCuen BW 2nd, Hao Y, Moon SJ, Tatebayashi M, Stinnett S et al. Lensectomy and vitrectomy decrease the rate of photoreceptor loss in rhodopsin P347L transgenic pigs. Graefes Arch Clin Exp Ophthalmol 2003; 241: 298–308.
Cao W, Li F, Steinberg RH, Lavail MM . Development of normal and injury-induced gene expression of aFGF, bFGF, CNTF, BDNF, GFAP and IGF-I in the rat retina. Exp Eye Res 2001; 72 (5): 591–604.
Rush R . Immunohistochemical localization of endogenous nerve growth factor. Nature 1984; 312 (5992): 364–367.
Machida S, Chaudry P, Shinobara T, Singh DP, Reddy VN, Chylack LT Jr et al. Lens-epithelium-derived growth factor promotes photoreceptor survival in light-damaged and RCS rats. Invest Ophthalmol Vis Sci 2001; 42 (5): 1087–1095.
Schori H, Kipnis J, Yoles E, WoldMussie E, Ruiz G, Wheeler LA et al. Vaccination for protection of retinal ganglion cells against death from glutamate cytotoxicity and ocular hypertension: Implications for glaucoma. Proc Natl Acad Sci USA 2001; 98 (6): 3398–3403.
Steel DHW, Lotery AJ . Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye 2013; 27: S1–S21.
Malagola R, Iozzo N, Grenga P, Arrico L, Nebbioso M . Partial posterior vitreous detachment: new capabilities of improving diagnosis and surgical approach using SD-OCT. Ophthalmologica 2014; 232: 1–98.
Sandeep S, Carsten MH, Masahito O, Levent A . Vitreoretinal Surgery. JAYPEE highlights medical publishers: New Delhi, India, 2012. p 69.
Turano K, Herdman SJ, Dagnelie G . Visual stabilization of posture in retinitis pigmentosa and in artificially restricted visual fields. Invest Ophthalmol Vis Sci 1993; 34: 3004–3010.
Vingolo EM, Nebbioso M, Domanico D, Valente S, Frati P . Post-operative hospitalization in retinal detachment correlation to recurrences. Ann Ist Super Sanita 2013; 49 (4): 336–339.
Vingolo EM, Gerace E, Valente S, Spadea L, Nebbioso M . Microincision vitrectomy surgery in vitreomacular traction syndrome of retinitis pigmentosa patients. Biomed Res Int 2014; 2014: 537081.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vingolo, E., Valente, S., Gerace, E. et al. Macular hole in retinitis pigmentosa patients: microincision vitrectomy with polydimethylsiloxane as possible treatment. Eye 29, 699–702 (2015). https://doi.org/10.1038/eye.2014.344
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.344
This article is cited by
-
Flap technique-assisted surgeries for advanced retinitis pigmentosa complicated with macular hole: a case report and literature review
BMC Ophthalmology (2021)
-
Lamellar hole-associated epiretinal membrane is a common feature of macular holes in retinitis pigmentosa
Eye (2020)
-
Management of Full-Thickness Macular Hole in A Genetically Confirmed Case with Usher Syndrome
Ophthalmology and Therapy (2020)
-
Vitreo-macular interface disorders in retinitis pigmentosa
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)