Abstract
Aim
Identify the incidence of vitreomacular traction (VMT) and frequency of reduced vision in the absence of other coexisting macular pathology using a pragmatic classification system for VMT in a population of patients referred to the hospital eye service.
Methods
A detailed survey of consecutive optical coherence tomography (OCT) scans was done in a high-throughput ocular imaging service to ascertain cases of vitreomacular adhesion (VMA) and VMT using a departmental classification system. Analysis was done on the stages of traction, visual acuity, and association with other macular conditions.
Results
In total, 4384 OCT scan episodes of 2223 patients were performed. Two hundred and fourteen eyes had VMA/VMT, with 112 eyes having coexisting macular pathology. Of 102 patients without coexisting pathology, 57 patients had VMT grade between 2 and 8, with a negative correlation between VMT grade and number of Snellen lines (r=−0.61717). There was a distinct cutoff in visual function when VMT grade was higher than 4 with the presence of cysts and sub retinal separation and breaks in the retinal layers.
Conclusions
VMT is a common encounter often associated with other coexisting macular pathology. We estimated an incidence rate of 0.01% of VMT cases with reduced vision and without coexisting macular pathology that may potentially benefit from intervention. Grading of VMT to select eyes with cyst formation as well as hole formation may be useful for targeting patients who are at higher risk of visual loss from VMT.
Similar content being viewed by others
Introduction
Vitreomacular traction (VMT) was first described in 1970 by Reese, Jones, and Cooper1 using ex vivo histological examinations of the vitreoretinal interface.
It is thought to occur following incomplete posterior vitreous detachment (PVD) when the posterior hyaloid face remains abnormally adherent to the inner retinal surface usually around the posterior pole and optic disc area.2, 3, 4, 5
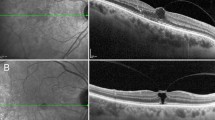
This gives rise to a hyper-reflective line anterior to the retinal surface visible on optical coherence tomography (OCT) scans, which is either not associated with any structural changes of the retinal parenchyma, so-called vitreomacular Adhesion (VMA) or VMT, where some effect of traction is visible.6, 7, 8
The ease with which VMT can be diagnosed using OCT has enabled accurate selection of patients for therapeutic interventions with surgery or pharmacological vitreolysis and also enabled detailed studies on classification, staging, and further understanding of the natural history of VMT.9, 10, 11, 12, 13
Although it has been widely recognised that VMT can occur in isolation or in association with common diseases of the macula such as diabetic macular oedema, retinal vein occlusion, posterior uveitis, and age-related macular degeneration,14, 15, 16 there have been no published data on the incidence of VMT in the general population or in the population of patients who have been referred to the hospital eye service. Information on how frequently VMT is encountered within the eye clinic setting and how frequently it causes reduced vision in the absence of other coexisting macular pathology are key outcomes, which may help clinicians and public health departments to understand the burden of the condition and to better plan for the provision of resources and delivery of diagnostic and treatment services. In this study, we conducted a detailed survey of consecutive OCT scans in a high-throughput ocular imaging service to ascertain the frequency of VMA and VMT presenting at a single centre and analysed the stages of traction, visual acuity, and association with other macular conditions.
Materials and methods
This non-interventional, retrospective study was conducted at a single site at Royal Wolverhampton Hospitals NHS Trust, UK. According to our institutional policy, ethics committee approval was not required for retrospective collection of anonymous data from patients’ clinical case records. The study setting was the retinal imaging department that provided, on-demand, multimodal retinal imaging services. Patients are usually referred from a catchment population of about 850 000 to our general ophthalmology service from the primary care sector in addition to patients referred into our secondary and tertiary macular referral service. All images from four networked OCT machines (Spectralis, Heidelberg Engineering GmbH, Heidelberg, Germany) were archived on a common server, enabling easy location of the records of individual imaging episodes. The default scanning mode of OCT was the 19 slice raster volume scan protocol, and the individual scans were viewed using the proprietary software (Heidelberg Eye Explorer, Heidelberg Engineering GmbH).
A study period of two consecutive months (June and July 2013) was randomly chosen. All patients who had at least one visit for OCT scanning (during this period) identified from the Heidelberg Eye Explorer database were included. For those patients who had more than one visit during the study period, the earliest visit in the study period was chosen as the study visit. This avoided the error of double counting any VMT case who attended twice in the 2-month period. For each study visit, the scan of each eye was analysed as two separate scanning episodes, unless only one eye was scanned. Therefore, during the study period each patient can only be analysed for one visit and each visit could generate a maximum of two scan episodes, once for each eye. Two observers (WFR and MA) performed a first pass screen of all scanning episodes to exclude those scans in which the posterior hyaloid line was not visible. All remaining scan episodes, which detected the posterior hyaloid line as a distinctly visible line anterior to the retina, were then viewed and graded by a senior retinal specialist (YCY) using our departmental system for classifying VMA and VMT on OCT (Table 1). The data were analysed to obtain the overall frequency of VMA and VMT. The breakdown in terms of grade of VMT with and without coexisting pathology was evaluated. In the presence of more than one coexisting pathology, the most visually significant one (in the opinion of the senior retinal specialist) was recorded for the study. To ensure that the number of consecutive OCT scan visits that we looked at in this study was representative, we estimated the overall number of patients seen in the retinal service over 2 months from our electronic patient appointment system and checked whether the number of patients included in the study was of a sufficient high proportion when compared with this denominator.
For the eyes confirmed to have VMA/VMT by the senior retinal specialist, visual acuity documented at the time of the study visit was retrospectively obtained from the case notes. Visual acuities obtained from case notes as Snellen fractions (6/36) were converted to number of lines read (eg, 6/36=2 lines and 6/5=8 lines) to allow derivation of mean, median, and range of Snellen lines read as a measure of visual function. First, the distribution of visual acuity across all VMA and VMT grades in eyes with and without coexisting pathology were determined. To evaluate the impact of VMT on visual acuity, the analysis was repeated after excluding those eyes with coexisting macular pathology for patients with VMA and VMT together (grades 1–8) and also VMT only (grades 2–8).
To estimate the incidence of VMT being encountered in a hospital retinal service, we extrapolated our rate of encountering of VMT grades 1–8 over 12 months and then expressed this rate of encounter as a percentage of 100 000 retinal clinic appointments per year using as denominator, our own number of retinal clinic appointments per year.
To provide an indirect estimation of the annual incidence of VMT in the general population, we extrapolated the number of new cases of VMT grades 1–8 encountered in the study over a 12-month period and then calculated the annual incidence rate per million population using as denominator, the size of our catchment population of 850 000.
Results
During the study period, a total of 4384 OCT scan episodes of 2223 patients were performed. From these scans 554 eyes of 378 patients were identified to have suspected VMA or VMT on first pass grading. On second pass grading performed by a senior retinal specialist (YCY), only 358 eyes of 278 patients were found to have the VMA or VMT of grades 0–8 (Figure 1). A total of 214 eyes in 175 patients had VMA or VMT of grades 1–8. Of these 175 patients, 39 patients (22%) had bilateral VMA or VMT. Of the 214 eyes with VMA or VMT, 102 eyes had isolated VMA or VMT but 112 eyes (52%) had coexisting pathology in addition to VMA/VMT. The breakdown of coexisting macular pathologies found on macular OCT scans is shown in Figure 2. Of the 102 eyes with isolated VMA or VMT, only 60 eyes (57 patients) fell into grades 2–8.
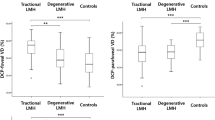
Of those eyes with VMA or VMT score of 0–8 (n=358), seven eyes had visual acuity of >0.5 lines and the remaining 351 eyes had median acuity of 6 lines (∼6/9) and a wide range between 0.5 and 8 lines. For the analysis of visual acuity owing to VMA or VMT alone, we excluded 144 eyes with Grade 0 (posterior hyaloid face not visible) and another 112 eyes with obvious coexisting macular pathology found on OCT scans. Of the remaining 102 eyes with VMA or VMT and no other macular pathology, 1 eye had visual acuity of count fingers, which was suspected to be due to a non-macular condition and 101 eyes had median acuity of 6 lines (mean 4.98 lines, range of 1–8 lines). The distribution of number of lines read across VMT grades of 1–8 in patients without coexisting macular pathology are shown in Table 2. In 60 eyes with VMT grade between 2 and 8 and no coexisting macular pathology, the relationship between VMT grade and number of Snellen lines read is shown in Figure 3. Generally, the higher the VMT grade the fewer Snellen lines were read by the eye. Using correlation analysis for continuous variables, there was a negative correlation between them (r=−0.61717).
We estimated from our electronic Patient Appointment System that the overall number of patient appointments into all retinal associated clinics in our department over any 2 month period was 2382 patients. Therefore, the cohort of 2223 patients we looked at who had at least one OCT over the 2-month study period represented 93% of this patient population.
Using the nominator of 175 patients with VMA or VMT grade 1–8 over the denominator of 2382 patients in 2 months, we derived the rate of encountering VMT to be 7346 patients per 100 000 retinal appointments (7.3%).
Using the nominator of 175 patients with VMA or VMT over 2 months and the denominator as our catchment population, we estimated the annual incidence to be 0.12% or 1200 patients per million per year.
Using the nominator of 14 patients with reduced vision due to VMA or VMT in at least one eye, encountered over 2 months, we estimated that an incidence of 0.01% in the population could be considered for therapeutic intervention.
Discussion
We surveyed scans of 2223 consecutive patients who were referred to our imaging department of OCT scans over a 2-month period when there were no departmental closures owing to public holidays or other reasons. We found 100 eyes with VMA only and another 114 eyes with various stages of VMT. We found a high percentage (52%) of eyes with VMA or VMT, which was associated with coexisting macular pathology. However, only 60 eyes had VMT of stages 2–8, which had some visible traction on the retina of which the majority were in the early stages between stage 2 and 4.
Using an indirect method of estimating the rate of encountering VMA or VMT, we found our rate to be 7.3% of all retinal referrals and retinal appointments and an annual estimated population incidence of 0.12%. As we did not sample a representative section of the population, these figures cannot be used to extrapolate for the estimation of prevalence of VMT in the overall population. However, because consecutive cases were sampled in our department over a 2-month period, this type of ascertainment method should give an indication of the incidence of VMA or VMT presenting to the hospital eye service over the period of 1 year. There are no published incidence studies of VMT to compare with, but the Beijing Eye study did use OCT to evaluate the completeness of PVD and found a prevalence figure of 2.3% with incomplete PVD.17 The prevalence of symptomatic VMT in patients with and without coexisting pathology was estimated by Jackson et al18 to be 0.35%. This discrepancy may not only be due to Jackson et al using combined numbers from smaller trials in tertiary referral centres compared with our general hospital setting but may also be due to the inevitable discrepancy in classification of VMA and VMT. Even with the help of OCT-grading systems, there may be variation in OCT interpretation of what actually constitutes early VMT. In this study, this error may be minimised by grouping VMA and VMT together for the estimations on the rate of encountering and annual incidence.
To our knowledge, there are no published studies correlating the grade of VMT to visual function. In terms of visual function expressed as number of lines read on the Snellen chart, the majority of eyes with stage 4 or better had good visual function, reading a median of 5–7 lines. However, in stages 5, 6, and 7 of VMT, the visual function was generally worse with median lines read of 1–3.5 lines only. From these figures, it is likely that not more than 14 eyes fall into the category of having VMT, which is visually symptomatic and not associated with other macular pathology. Extrapolating this over a period of 12 months would give an incidence of 84 new cases per year in a population of 850 000 or ∼100 eyes per year from a population of one million (0.01%). Although we found a correlation between visual function and grade of VMT, there was a large variability of visual function within each VMT grade (Table 2). This may be due to coexisting pathology that was not visible on the OCT scan such as cataract or it may be due to the inherent lack of correlation between OCT characteristics and visual function. It is worthwhile to note that even in the pivotal study for Ocriplasmin, anatomical rather than visual outcomes were reported.12 This observation of a relationship between visual function and VMT grade, therefore, supports the avoidance of a strict visual cutoff in the recent guidelines (TA 297) on use of ocriplasmin for symptomatic VMT.19
A potential weakness in our study is the use of visual acuity measured using the Snellen chart and collected retrospectively from case notes. To evaluate the correlation of VMT with visual function, it would be more ideal to use protocol best corrected visual acuity in eyes, which have no other coexisting pathology confirmed on full ophthalmic examination. However despite the noise, we were able to show a distinct cutoff in visual function when VMT grade was higher than 4, with the presence of cysts and sub retinal separation and breaks in the retinal layers. This would be in keeping with our understanding of the pathogenesis of VMT and macular hole formation.6
A potential strength of this study is the use of a very pragmatic and easy grading system for VMT features on OCT scan. This study revealed a potential cut-off when cysts are present near the fovea on OCT scans. Currently the International Classification System divides cases into VMA, VMT, and full thickness macular hole with subclassifications in each category according to size of macular hole and whether the adhesion width is </> 1500 μm.10 Further studies will be needed to evaluate whether the presence or absence of cyst formation could be usefully incorporated into criteria for predicting visual improvement following therapy for VMT. Another strong point of our study lies in the large number of consecutive scans surveyed over time, which allowed us to ascertain new cases, as they were referred and enabling an estimation of the incidence of VMT in a hospital population. To our knowledge this has not been studied in this way before and should be a useful public health resource.
In conclusion, we found that VMT was a very common encounter in our everyday retinal practice, and many cases were associated with other coexisting macular pathology. We estimated an incidence rate of 0.01% of VMT cases with reduced vision and without coexisting macular pathology that may potentially benefit from intervention. Grading of VMT to select eyes with cyst formation as well as hole formation may be useful for targeting patients who are at higher risk of visual loss from VMT.

References
Reese AB, Jones IS, Cooper WC . Vitreomacular traction syndrome confirmed histologically. Am J Ophthalmol 1970; 69 (6): 975–977.
Sebag J . Anatomy and pathology of the vitreoretinal interface. Eye (Lond) 1992; 6: 541–552.
Smiddy WE, Michels RG, Green WR . Morphology, pathology, and surgery of idiopathic vitreoretinal macular disorders. A review. Retina 1990; 10: 288–296.
Miller B, Miller H, Ryan SJ . Experimental vitreous syneresis. Arch Ophthalmol 1985; 103: 1385–1388.
Sebag J . Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol 2004; 242: 690–698.
Steel DHW, Lotery AG . Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye 2013; 27: S1–S21.
Mirza RG, Johnson MW, Jampol LM . Optical coherence tomography use in evaluation of the vitreoretinal interface: a review. Surv Ophthalmol 2007; 52: 397–421.
Bottós JM, Elizalde J, Rodrigues EB, Maia M . Current concepts in vitreomacular traction syndrome. Curr Opin Ophthalmol 2012; 23 (3): 195–201.
Jackson TL, Nicod E, Angelis A, Grimaccia F, Prevost AT, Simpson AR et al. Pars plana vitrectomy for vitreomacular traction syndrome: a systematic review and metaanalysis of safety and efficacy. Retina 2013; 33 (10): 2012–2017.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013; 120 (12): 2611–2619.
Stalmans P, Duker JS, Kaiser PK, Heier JS, Dugel PU, Gandorfer A et al. Oct-based interpretation of the vitreomacular interface and indications for pharmacologic vitreolysis. Retina 2013; 33 (10): 2003–2011.
Stalmans P, Benz MS, Gandorfer A, Kampik A, Girach A, Pakola S et alMIVI-TRUST Study Group. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med 2012; 367 (7): 606–615.
Gallemore RP, Jumper JM, McCuen BW, Jaffe GJ, Postel EA, Toth CA . Diagnosis of vitreoretinal adhesions in macular disease with optical coherence tomography. Retina 2000; 20 (2): 115–120.
Jackson TL, Nicod E, Angelis A, Grimaccia F, Prevost AT, Simpson AR et al. Vitreous attachment in age-related macular degeneration, diabetic macular edema, and retinal vein occlusion: a systematic review and metaanalysis. Retina 2013; 33 (6): 1099–1108.
Gallagher MJ, Yilmaz T, Cervantes-Castañeda RA, Foster CS . The characteristic features of optical coherence tomography in posterior uveitis. Br J Ophthalmol 2007; 91 (12): 1680–1685.
Maier M, Pfrommer S, Burzer S, Feucht N, Winkler von Mohrenfels C, Lohmann CP . Vitreomacular interface and posterior vitreomacular adhesion in exudative age-related macular degeneration (AMD): an OCT-based comparative study. Klin Monbl Augenheilkd 2012; 229 (10): 1030–1035.
Shao L, Xu L, You QS, Wang YX, Chen CX, Yang H et al. Prevalence and associations of incomplete posterior vitreous detachment in adult Chinese: The Beijing Eye Study. PLoS One 2013; 8: e58498.
Jackson TL, Nicod E, Simpson A, Angelis A, Grimaccia F, Kanavos P . Symptomatic vitreomacular adhesion. Retina 2013; 33: 1503–1511.
NICE. Ocriplasmin for treating vitreomacular traction http://guidance.nice.org.uk/TA297. October 2013. Accessed on: 30 July 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The results of this manuscript have previously been presented at the Oxford Ophthalmological Congress Meeting July 2014.
Rights and permissions
About this article
Cite this article
Fusi-Rubiano, W., Awad, M., Manjunath, R. et al. Spectrum of morphological and visual changes due to vitreomacular interface disorders encountered in a large consecutive cohort of patients. Eye 29, 397–402 (2015). https://doi.org/10.1038/eye.2014.313
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.313
This article is cited by
-
Swept-source optical coherence tomography changes and visual acuity among Palestinian retinitis Pigmentosa patients: a cross-sectional study
BMC Ophthalmology (2021)
-
The effect of phacoemulsification performed with vitrectomy on choroidal vascularity index in eyes with vitreomacular diseases
Scientific Reports (2021)
-
Vitreo-macular interface disorders in retinitis pigmentosa
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
A retrospective cohort study in patients with tractional diseases of the vitreomacular interface (ReCoVit)
Graefe's Archive for Clinical and Experimental Ophthalmology (2016)