Abstract
Purpose
To analyze the intraoperative usefulness and postoperative results of endoilluminator use during pediatric cataract surgery.
Methods
Medical records of children <8 years of age who underwent lens aspiration with primary posterior capsulectomy (PPC) and anterior vitrectomy (AV) with or without intraocular lens implantation (IOL) were studied. An endoilluminator was used intraoperatively as an external light source in all cases to ensure the completeness of PPC and adequacy of AV. All children were divided into three groups depending upon the age at surgery and presence of IOL. We included only the first operated eye in bilateral cases. We studied the intraoperative performance for all and postoperative complications for those with >6 months follow-up.
Results
The charts of 79 eyes of 46 children (26 boys, 20 girls: 33 bilateral, 13 unilateral) were reviewed, of which we analyzed 46 eyes of 46 children for intraoperative performance and 42 eyes of 42 children for postoperative complications. The intraoperatively adequate size of PPC was obtained in all cases with no vitreous in the anterior chamber. Two cases in the first group developed peaking of the pupil, and one case developed visual axis contraction requiring membranectomy. None of the cases in the other groups developed any complication.
Conclusion
An endoilluminator is a simple, safe, and powerful tool for better visualization of the posterior capsule and anterior vitreous during pediatric cataract surgery. It helps in confirming a good vitrectomy, ensuring its completeness and thereby reducing the chances of any complication due to inadequate AV.
Similar content being viewed by others
Introduction
Pediatric cataract surgery warrants a primary posterior capsulectomy (PPC) and anterior virectomy (AV) in children less than 6 years age to avoid visual axis opacification (VAO) during the postoperative period.1 PPC may be recommended even in older children due to co-morbidities like mental retardation. PPC can be done either manually (manual capsulorhexis), or by using a vitrector (vitrectorhexis) or with a bipolar diathermy. The major hurdles encountered during posterior capsular management in pediatric cataract surgery are inability to either initiate or complete a PPC, radial extension of the PPC, and disturbance of the anterior vitreous phase prior to its completion. Even with the new generation operating microscopes and high-end instrumentations, visualization of the shearing edge of the posterior capsule or the posterior capsulectomy rim may be difficult. Also, the vitreous gel is a transparent structure and owing to its invisible nature, it is often difficult to visualize it during the procedure of vitrectomy. In addition, it is difficult to decide upon the end point of vitrectomy as we are not able to confirm if the vitreous is completely cleared off from the anterior chamber and the pupillary plane under the microscope light alone. This may be true even for experienced surgeons. An endoilluminator was used in adult cataract surgery while performing phacoemulsification in a case of cataract complicated with corneal opacity2 and to facilitate anterior capsulorhexis when visualization is poor due to a mature cataract.3 We have previously described the technique of using the endoilluminator as a simple and easy method for better visualization of PPC and vitreous in pediatric cataract surgery.4 In the present study we evaluate the intraoperative performance of the endoilluminator in our series of pediatric cataract extraction surgeries and provide their postoperative results.
Patients and methods
A retrospective analysis of the charts of children who underwent cataract extraction with PPC and AV with or without intraocular lens (IOL) implantation was done. All charts were reviewed for intraoperative completeness while those with a minimum of 6 months follow-up were considered for postoperative outcomes. For the bilateral cases, only the first operated eye was considered for analysis. Children with traumatic or complicated cataracts and those who underwent cataract extraction without PPC or AV were excluded. As the risk of developing postoperative complications is commoner in younger children,5, 6, 7, 8, 9 we divided all the children into less and more than 2 years. As implantation of IOL can further influence intraoperative difficulties and postoperative complications like VAO, the children less than 2 years were further divided on the basis of IOL implantation. Finally, there were three groups depending upon the age at the time of surgery and insertion of IOL: Group 1 included those who underwent surgery below 2 years of age without IOL, Group 2 included children below 2 years of age with IOL, and Group 3 included those between 2 to 8 years of age.
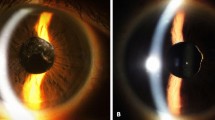
All surgeries were performed using a similar technique by one surgeon (JM) or under her supervision. The procedure4 involved superior rectus bridle suture, superior clear corneal tunnel (for foldable IOLs) or conjunctival peritomy with scleral tunnel (for rigid IOLs), two side ports, manual capsulorhexis, hydroprocedures, and bimanual irrigation and aspiration of the lens material. After lens aspiration, manual primary posterior capsulorhexis with microrhexis forceps was performed in all cases of IOL implantation, with the size being kept smaller than the anterior capsulorhexis opening. In patients that were left aphakic, the posterior capsulectomy was made with the vitrector. In the aphakic cases, both the capsulectomies were made of the same size of ∼≥5 mm. This was followed by AV. Thereafter the room and microscope light were switched off and the endoilluminator was held externally along the limbus to allow the light to fall tangentially to look for the completeness of the capsulectomy by following the cut edge of the posterior capsule and also to locate any vitreous tags (Figure 1) or strands that could be above the pupil or in the anterior chamber. In cases where an anterior chamber maintainer was used, the endoilluminator was held by the operating surgeon, but in its absence, an assistant held the light source during the procedure of vitrectomy. Vitrectomy was continued till the vitreous was below the posterior capsular opening as visualized directly under the oblique light of the endoilluminator. In all the cases AV was done by the limbal route. Once the AV was completed, an IOL was implanted in the capsular bag wherever indicated. Finally the incision was closed with 10-0 monofilament nylon or 10-0 polyglactin 910 sutures. All children received subconjunctival 2 mg dexamethasone and 20 mg gentamycin. Postoperatively all eyes received 1% topical prednisolone acetate, 1% cyclopentolate hydrochloride, and 0.5% moxifloxacin hydrochloride eye drops in tapering dosage over 6 weeks. No systemic medications were advised. The children were followed up postoperatively on day 1, after 1 week, 3 weeks and 6 weeks, and 3 monthly thereafter.
Outcome measures
The intraoperative completeness of PPC and AV (Figure 2) was confirmed by direct visualization under the microscope with the aid of the endoilluminator. Postoperative outcome measures included irregularities of the pupillary margins, vitreous in anterior chamber, contracture of the capsulectomy opening and VAO as seen with a hand-held or table-mount slit-lamp or having a poor glow when seen with a direct ophthalmoscope needing a secondary procedure. As all cases underwent surgery using the endoilluminator, there was no control group for comparison.
Results
Seventy-nine eyes of 46 children (26 boys and 20 girls) were studied (Table 1). Six eyes of 4 children (2 bilateral and 2 unilateral) that were analyzed for the intraoperative outcome were excluded from the analysis of the postoperative outcome owing to a short follow-up of <6 months. Thirty-three children had bilateral cataracts while 13 children presented with unilateral cataract. For the purpose of analysis, we included only the first operated eye of all bilateral cases. The etiology of the cataract was congenital in 32 eyes, developmental in 12 eyes, and steroid induced in 2 eyes.
In group 1, 20 eyes of 20 children were included; 16 children had bilateral cataracts and 4 had unilateral cataract. None of the children received any IOL implantation. All children were under 1 year of age, except for one child who was 15 months of age in whom the IOL was deferred as the child had microphthalmos with a microcornea of 8 mm. The mean age at the time of surgery was 4.75±3.45 months (range: 6 weeks to 15 months). The mean follow-up was 28.05±16.40 months (range: 7 to 71 months).
In group 2, 8 eyes of 8 children were included; 4 children had bilateral cataracts and 4 had unilateral cataract. IOL was implanted in all the children. The mean age at the time of surgery was 13.75±7.65 months (range: 4 to 22 months). The mean follow-up of six eyes was 21.33±12.56 months (range: 7 to 36 months). The remaining two eyes had a follow-up of <6 months and were included only as a part of the intraoperative outcome study.
In group 3, 18 eyes of 18 children were included; 13 children had bilateral cataract and 5 had unilateral cataract. IOL was implanted in 17 children, while 1 patient was left aphakic owing to microcornea with microphthalmos. The mean age at the time of surgery was 47.0±16.88 months (range: 27 to 96 months). The mean follow-up of 16 eyes was 23.19±12.17 months (range: 6 to 43 months). The remaining two eyes had a follow-up of less than 6 months and were included only to study the intraoperative outcome.
The overall average follow-up of the patient was 25.23±14.52 months. Thirty four eyes (80.95%) were followed for more than 1 year, out of which 22 (52.38%) eyes were followed for more than 2 years.
Intraoperative outcomes
Intraoperative outcome was studied in all the 46 eyes of 46 children. The adequate size of PPC could be obtained from the limbal approach in all the children of the groups, even those with microcornea and at a very young age, using the endoilluminator. Thorough removal of vitreous from the anterior chamber was confirmed in all the cases using the endoilluminator.
Postoperative outcomes
Postoperative outcome was studied in 42 eyes of 42 children. In group 1, peaking of the pupil was noted in two children, but visual axis remained clear after 7 months of follow-up in one and 39 months in another. Capsulectomy contraction was noted in 1 child (5%), resulting in less than 1 mm of central visual axis clearance requiring membranectomy. All these complications were noted within the first 3 postoperative months. In groups 2 and 3, no complications were noted and the visual axis remained clear (Figure 3). Postoperative raised intraocular pressure was noted in two eyes, both in group 1. The first was a 7-month-old child in whom it was transient and resolved within 4 weeks of treatment, while the second one was a 15-month-old child who required surgical intervention for pressure control. No postoperative glaucoma was noted in groups 2 and 3.
Discussion
Posterior capsulectomy with or without AV is widely accepted as a primary procedure during cataract surgery, mainly in young children. Performing a good and perfect PPC can be technically difficult. For surgeries that require AV, it is mandatory that it be done thoroughly and completely, for, if left incomplete, the vitreous can act as a scaffold, resulting in a membrane formation and opacification of the visual axis postoperatively. Here again, the limiting step in any vitrectomy is visualization of the invisible vitreous and its strands. There have been few signs of anterior vitreous phase disturbance10 that have been described in the literature, which help to identify the presence of the vitreous in the anterior chamber and indicate an incomplete vitrectomy. These include presence of vitreous strands tugged to the capsule flap or pupil, distortion of the anterior and/or posterior capsulorhexis margins, and so on. These signs can sometimes be very subtle and be easily missed.
An endoilluminator is a simple and efficient instrument that has been used since long by the retinal surgeons, initially as an external slit illuminator in the 1970s.11 In 1976, for 3-port vitrectomy, Peyman12 for the first time used endoillumination with an optic fibre inserted in the vitreous cavity, after which it became a regular norm in retinal surgeries. Oyakawa et al13 in 1984 described the use of an irrigating endoilluminator called the May illuminated infusion needle for the purpose of AV. However, this instrument was expensive and did not get popularized.
We have previously described and reported the use of an endoilluminator in cataract surgery.4 The principle remains the same, except that this instrument is held externally over the limbus or the cornea, such that the light falls obliquely, thereby aiding in better visualization of the posterior capsule and the anterior vitreous (Figure 4) ‘seeing the invisible’. In pediatric cataract surgery, in addition to its use in checking the completeness of the PPC and adequacy of the AV, we even use it to perform PPC and AV in the following ways. During the procedure of PPC, it helps to identify the initial break, as at times it may not be visible under the microscope (Supplementary Video). It helps to differentiate the posterior capsular opening from the break in the vitreous phase (Supplementary Video), facilitating the completion of capsulorhexis (Supplementary Video), and to avoid an advertent pull on the vitreous strands. A similar principle has been used to perform anterior capsulorhexis in mature cataracts3 and for phacoemulsification in a case with poor visualization due to corneal opacity.2
The literature describes the use of certain medications for identifying the vitreous gel. Shah et al14 described preservative-free triamcinolone acetonide-assisted vitrectomy during pediatric cataract surgery as an effective way of ensuing complete vitrectomy. Praveen et al15 studied the use of preservative-free triamcinolone acetonide in 43 eyes of children and concluded that a thorough vitrectomy can be ensured with no adverse reactions up to 12 months. Though preservative-free triamcinolone may be a good technique in assisting AV, it is not without complications, which are related to the improper and inaccurate method of instillation16 into the eye, since this technique requires expertise or practice. Complications reported could range from secondary glaucoma17 to endophthalmitis.18
The endoilluminator is readily available and not expensive. No special expertise is needed to perform the procedure and it can be mastered easily. Since it has to be used externally over the cornea or limbus, unlike internal use by the retinal surgeons, there are no possibilities of getting any complications with this instrument.
In our study, we found that one child in group 1 developed contracture of the visual axis while none of the children in group 2 or 3 developed any contraction. Persistent peaking of the pupil was seen in two eyes of different patients from group 1 and could be related to the remnant vitreous strand in the anterior chamber; however, the visual axis remained clear and hence required no intervention for either, one being followed up for 7 months and the other for 39 months. Two eyes in group 1 developed postoperative raised intraocular pressure. The higher complication rate in group 1 can be related to the higher number of children with microcornea and aphakia in this group.
Children under 1 year have the maximum complications of surgery as regards the rate of VAO. Plager et al19 showed in their study the development of VAO in 12% of cases operated under 1 year without IOL implantation. Similarly, the Infant Aphakia Treatment Study20 showed that the rate of VAO in children operated under 1 year without IOL was 11.1%. In our study, the same group (without IOL implantation) encountered a low rate of complications, which we attribute to an adequate posterior capsulectomy and good AV facilitated by the use of endoilluminator. Moreover, the pars plana approach for vitrectomy is suggested21 as a better approach for a larger size of PPC and a good vitrectomy, but we observed that the same effect can be obtained even from a limbal route with the aid of the endoilluminator.
We do acknowledge our limitations as it is a retrospective study and it lacks a control group. In addition, triamcinolone acetonide could have been used intraoperatively to confirm the efficiency of the endoilluminator in identifying the disturbance of the vitreous phase. However, this is the first study to describe the effectiveness of the endoilluminator during pediatric cataract surgery in identifying not only the vitreous gel but also the posterior capsule.
In conclusion, endoilluminator use in pediatric cataract surgery acts as a safe method for better visualization of the posterior capsule and anterior vitreous, ensuring a good capsulectomy and complete removal of the prolapsed vitreous from the anterior chamber, thereby removing any scaffold. It thus reduces the chances of any posterior capsular opacification related to an incomplete AV, ensuring a clear visual axis.

References
Jensen AA, Basti S, Greenwald MJ, Mets MB . When may the posterior capsule be preserved in pediatric intraocular lens surgery? Ophthalmology 2002; 109: 324–327.
Nishimura A, Kobayashi A, Segawa Y, Sugiyama K . Endoillumination-assisted cataract surgery in a patient with corneal opacity. J Cataract Refract Surg 2003; 29: 2277–2280.
Akin T, Aykan U, Karadavi K, Aydin A, Yildiz TF, Bilge AH . Capsulorhexis in white cataract using a green-light endoillumination probe. Ophthalmic Surg Lasers Imagine 2007; 38: 520–522.
Matalia JH, Tejwani S, Murthy SI, Thomas R . Endoilluminator-assisted technique for visualization of vitreous during anterior vitrectomy. Asian J Ophthalmol 2008; 10: 395–397.
Knight-Nanan D, O’Keefe M, Bowell R . Outcome and complications of intraocular lenses in children with cataract. J Cataract Refract Surg 1996; 22: 730–736.
Hiles DA, Hered RW . Modern intraocular lens implants in children with new age limitations. J Cataract Refract Surg 1987; 13: 493–497.
Oliver M, Milstein A, Pollack A . Posterior chamber lens implantation in infants and juveniles. Eur J Implant Refract Surg 1990; 2: 309–314.
Vasavada A, Chauhan H . Intraocular lens implantation in infants with congenital cataracts. J Cataract Refract Surg 1994; 20: 592–598.
O’Keefe M, Fenton S, Lanigan B . Visual outcomes and complications of posterior chamber intraocular lens implantation in the first year of life. J Cataract Refract Surg 2001; 27: 2006–2011.
Praveen MR, Vasavada AR, Koul A, Trivedi RH, Vasavada VA, Vasavada VA . Subtle signs of anterior vitreous face disturbance during posterior capsulorhexis in pediatric cataract surgery. J Cataract Refract Surg 2008; 34: 163–167.
Machemer R, Buettner H, Norton EW, Parel JM . Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol 1971; 75: 813–820.
Peyman GA . Improved vitrectomy illumination system. Am J Ophthalmol 1976; 81: 99–100.
Oyakawa RT, Lusby FW, Schachat AP, Brown RH . The use of an irrigating endo-illuminator for anterior vitrectomy. Ophthalmic Surg 1984; 15: 400–401.
Shah SK, Vasavada V, Praveen MR, Vasavada AR, Trivedi RH, Dixit NV . Triamcinolone-assisted vitrectomy in pediatric cataract surgery. J Cataract Refract Surg 2009; 35: 230–232.
Praveen MR, Shah SK, Vasavada VA, Dixit NV, Vasavada AR, Garg VS et al. Triamcinolone-assisted vitrectomy in pediatric cataract surgery: intraoperative effectiveness and postoperative outcome. J AAPOS 2010; 14: 340–344.
Burk SE, Da Mata AP, Snyder ME . Visualizing vitreous using Kenalog suspension. J Cataract Refract Surg 2003; 29: 645–651.
Burk SE, Da Mata AP, Osher RH, Cionni RJ . Triamcinolone-assisted anterior vitrectomy. The art of visualizing the vitreous. Cataract Refract Surg Today 2005; 61–64.
Scott IU, Flynn HW Jr . Reducing the risk of endophthalmitis following intravitreal injections. Retina 2007; 27: 10–12.
Plager DA, Yang S, Neely D, Sprunger D, Sondhi N . Complications in the first year following cataract surgery with and without IOL in infants and older children. J AAPOS 2002; 6: 9–14.
Plager DA, Lynn DA, Buckley EG, Wilson ME, Lambert SR, Infant Aphakia Treatment Study Group. Complications, adverse events, and additional intraocular surgery 1 year after cataract surgery in the infant Aphakia Treatment Study. Ophthalmology 2011; 118: 2330–2334.
Trivedi RH, Wilson ME Jr . Posterior capsulotomy and anterior vitrectomy for the management of pediatric cataracts. In Wilson ME, Trivedi RH, Pandey SK eds. Pediatric Cataract Surgery: Techniques, Complications, and Management. Lippincott Williams and Wilkins: Philadelphia, 2005 p 90 (table 16-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Matalia, J., Anaspure, H., Shetty, B. et al. Intraoperative usefulness and postoperative results of the endoilluminator for performing primary posterior capsulectomy and anterior vitrectomy during pediatric cataract surgery. Eye 28, 1008–1013 (2014). https://doi.org/10.1038/eye.2014.136
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.136
This article is cited by
-
Update on Pediatric Cataract Surgery and the Delphi Panel Paper
Current Ophthalmology Reports (2018)