Abstract
Purpose
To evaluate the agreement between event- and trend-based analyses to determine visual field (VF) progression in glaucoma.
Methods
VFs of 175 glaucoma eyes with ≥5 VFs were analyzed by proprietary software of VF analyzer to determine progression. Agreement (κ) between trend-based analysis of VF index (VFI) and event-based analysis (glaucoma progression analysis, GPA) was evaluated. For eyes progressing by event- and trend-based methods, time to progression by two methods was calculated.
Results
Median number of VFs per eye was 7 and follow-up 7.5 years. GPA classified 101 eyes (57.7%) as stable, 30 eyes (17.1%) as possible and 44 eyes (25.2%) as likely progression. Trend-based analysis classified 122 eyes (69.7%) as stable (slope >−1% per year or any slope magnitude with P>0.05), 53 eyes (30.3%) as progressing with slope <−1% per year, P≤0.05 (sensitive criteria), and 37 eyes (21.1%) as progressing with slope <−1% per year, P≤0.01 (specific criteria). κ between sensitive criteria of GPA (possible combined with likely progression) and trend-based analysis was 0.48, and between specific criteria of GPA (possible clubbed with no progression) and trend-based analysis was 0.50. In eyes progressing by sensitive criteria of both methods (42 eyes), median time to progression by GPA (4.9 years) was similar (P=0.30) to trend-based method (5.0 years). This was also similar in eyes progressing by specific criteria of both methods (25 eyes; 5.6 years versus 5.9 years, P=0.23).
Conclusion
Agreement between event- and trend-based progression analysis was moderate. GPA seemed to detect progression earlier than trend-based analysis, but this wasn’t statistically significant.
Similar content being viewed by others
Introduction
Glaucoma is a progressive optic neuropathy characterized by typical optic disc and retinal nerve fiber layer changes with correlating visual field (VF) defects. The standard method to detect glaucoma progression is to monitor the VF defects periodically for change. Two commonly used approaches to detect change in VF defects over time are the event-based and the trend-based progression analyses. Event-based analysis determines VF progression to be either present or absent depending on a predefined change in the VF parameters. Trend-based analysis provides the actual rate of change of VF parameters. In clinical practice, information from both these analyses is important because it is not only sufficient to identify VF progression in glaucoma but also to determine the rate of progression (ROP), so that the treatment can be more aggressive in fast progressors.
The recently introduced Guided Progression Analysis by the Humphrey VF Analyzer (Carl Zeiss Meditec, Inc. Dublin, CA, USA) provides both an event-based progression analysis and a trend-based analysis on the same printout. The event-based progression analysis, called the glaucoma progression analysis (GPA), is based on the criteria designed to identify VF progression in the Early Manifest Glaucoma Trial.1 Trend-based progression analysis is based on the ROP of the visual function of the eye through a linear regression model using a new global index, VF index (VFI).2 The VFI is the aggregate percentage of visual function for a given field at each point where the visual thresholds are estimated. VFI is calculated from pattern deviation plots in eyes with a mean deviation (MD) of better than −20 dB and from total deviation plots in eyes with a MD worse than −20 dB. The central points have more weight than peripheral points.
The purpose of this study was to evaluate the agreement between the event-based and the new trend-based analyses provided by the Guided Progression Analysis software to determine VF progression in glaucoma.
Materials and methods
In this clinic-based study, VF print outs of all patients of primary open angle (POAG) and primary angle closure glaucoma (PACG), who had undergone 5 or more Humphrey VF examinations (either full threshold or Swedish Interactive Threshold Algorithm-standard, either 24-2 or 30-2, or a combination of both) between 1989 and 2008 were examined. The methodology and the exclusion criteria have been described previously.3, 4 Informed consent was obtained from all participants and the Ethics Committee of L V Prasad Eye Institute approved the study.
For purposes of the study, POAG was defined in the presence of an open anterior chamber angle on gonioscopy, glaucomatous optic disc damage on clinical examination (focal or diffuse neuroretinal rim thinning, localized notching or nerve fiber layer defects), and corresponding VF defects. PACG was defined in the presence of an occludable angle on gonioscopy (posterior trabecular meshwork not seen in at least 180° of the total circumference of the angle in primary position), glaucomatous optic disc damage and corresponding VF defects. Gonioscopy was performed using a Goldmann’s two mirror lens or a Sussmann’s four mirror gonioscope under standard conditions. VF defects were considered glaucomatous if at least two of the three Anderson’s criteria (three or more non-edged points in a cluster depressed to P<5% and one of which depressed to P<1%, Glaucoma Hemifield Test outside normal limits and pattern SD depressed to P<5%) were fulfilled.5 A single physician (CSG) did the clinical examination of all patients.
The VFs of all the patients were evaluated for reliability. Fields with fixation losses, false-positive or false-negative response rates of >20% were considered unreliable and excluded from the analysis. The reliable VFs of all these patients were analyzed by the new Guided Progression Analysis software, which provides both an event-based and a trend-based progression analysis. For both these analysis, the first two reliable tests were considered as the baseline and ROP on trend-based analysis as well as stability or progression on event-based analysis were determined from the 5th VF through the last follow-up VF.
The event-based progression analysis, GPA uses statistical criteria designed for the Early Manifest Glaucoma Trial to identify progression of VF defects.1 When significant (P<0.05) deterioration is evident on the pattern deviation probability maps at the same three or more points on two consecutive follow-up tests, the GPA flags this as ‘possible progression’; if significant deterioration is seen at the same three or more points in three consecutive follow-up tests, GPA flags this as ‘likely progression’. When both the above criteria are not met, the software flags as ‘no progression detected’. When the VF is severely depressed (MD <−20 dB), GPA doesn’t determine progression. For the purpose of analysis, we dichotomized the GPA classification results separately based on 2 criteria; a ‘sensitive criterion’ where the possible progression group was clubbed with the likely progression group and a ‘specific criterion’ where the possible progression group was clubbed with the no progression group.
Unlike the event-based analysis, the trend-based analysis of Guided Progression Analysis software only provides the slope of the change of VFI with time but no simple language interpretation of the same. This being a linear regression analysis, the software also provides a P-value associated with the magnitude of the slope. For the purpose of this study, we defined progression on trend-based analysis in terms of both the magnitude of the slope and the P-value associated with it. We considered a slope magnitude of −1% per year or worse as clinically significant. For the purpose of analysis, we dichotomized the trend-based analysis results separately based on two criteria; a ‘sensitive criterion’ when the magnitude of VFI slope was worse than −1% per year with a P-value of ≤0.05 and a ‘specific criterion’ when the magnitude of slope was worse than −1% per year with a P-value of ≤0.01. Any slope better than −1% per year or any slope magnitude with a P-value not meeting the above criteria was considered as stable.
Statistical analysis
Descriptive statistics included mean and SD for normally distributed variables and median and inter-quartile range (IQR) for non-normally distributed variables. Chance-corrected agreement between the event- and trend-based approaches to assess VF progression was assessed using kappa statistic (κ).6 Strength of agreement was categorized according to the method proposed by Landis and Koch:7 less than 0 was poor, 0–0.20 was slight, 0.21–0.40 was fair, 0.41–0.60 was moderate, 0.61–0.80 was substantial, and 0.81–1.00 was almost perfect. For eyes showing progression both by event- and trend-based methods, we calculated the time to progression detection by the two methods to identify the method that diagnosed progression early. Considering the event-based criteria as the standard, we also calculated the diagnostic accuracy of the trend-based criteria to detect progression. The diagnostic accuracy parameters calculated were sensitivity, specificity, predictive values, and likelihood ratios (LR). Statistical analyses were performed using commercial software (Stata ver. 11.1; StataCorp, College Station, TX, USA). A P-value of ≤0.05 was considered statistically significant.
Results
Five hundred and forty four eyes of 335 primary glaucoma patients treated by a single physician (CSG) at our Institute between 1989 and 2008 had five or more HVF examinations. The number of eyes excluded from the current analysis and the reasons for exclusion are briefly summarized in the flow chart (Figure 1). Two hundred and thirty eight eyes of 175 patients fulfilled the inclusion criteria for this study. From the patients whose both eyes were eligible, one eye was randomly chosen for analysis. Table 1 shows the demographic, clinical, and VF features of the 175 eyes of 175 study participants included for the final analysis.
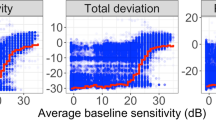
The median magnitude of VFI slope in the entire cohort was −0.7% per year (IQR: −1.9 to 0.1). We compared the VFI slopes of the study participants in the three GPA categories (stable, possible, and likely progression; Table 2 and Figure 2). The ROP of VFI was statistically significantly different between all the three GPA categories.
Event-based analysis classified 101 eyes (57.7%) as stable, 30 eyes (17.1%) as possible progression and 44 eyes (25.2%) as likely progression. Trend-based analysis classified 122 eyes (69.7%) as stable, 53 eyes (30.3%) as progressing by the sensitive criteria and 37 eyes (21.1%) as progressing by the specific criteria. Table 3 shows the agreement separately for the sensitive and the specific criteria of the event-based and the trend-based progression methods. Table 4 shows the diagnostic accuracy parameters of sensitive and specific criteria of trend-based progression analysis considering the sensitive and specific criteria of event-based analysis, respectively, as the standard.
In eyes classified as progressed by the sensitive criteria of both, the event- and trend-based methods (42 eyes), median time to progression by event-based analysis (4.9 years, IQR: 3.9–6.9 years) was similar to (P=0.30, Wilcoxon-signed rank test) that by trend-based method (5.0 years, IQR: 3.9–7.2). In eyes classified as progressed by the specific criteria of both, the event- and trend-based method (25 eyes), median time to progression by event-based analysis (5.6 years, IQR: 4.0–7.5 years) was also similar (P=0.23) to that by trend-based method (5.9 years, IQR: 4.8–7.8).
Discussion
There is currently no consensus regarding the best approach to detect VF progression. The ideal method for detecting VF progression should be sensitive, detect progression with few examinations, maintain high specificity, and be resistant to fluctuation.8 Though a few studies have used progression judged by clinicians as standard,9, 10, 11, 12 Werner et al9 have reported that the agreement between clinicians was in fact worse than that between statistical analyses. The two most commonly used approaches to detect VF progression are the trend-based and the event-based analyses. But both of these are known to have a few unique limitations. One of the major limitations of the trend-based analysis is the length of the follow-up required to detect progression, which itself is influenced by a number of factors, including examination frequency, underlying rate and type of progression, the specific parameter being evaluated, the degree of variability, and position of the VF within the time series.8, 13 The ability of the event-based analysis to detect progression is dependent upon the degree of change exceeding test–retest variability of stable glaucoma patients, which is known to be already high for damaged locations. Therefore, the event-based approach is also likely to be less sensitive to smaller changes in the VF parameters. In addition, event-based analyses have also been shown to be vulnerable to threshold variability.8
In this study, we evaluated the agreement between the event-based and the new trend-based analysis, based on a new global index, VFI, to determine VF progression. Trend-based analyses, till date, have been largely applied to threshold sensitivities at individual points and to MD.8, 9, 14, 15 A limitation to this was the influence of media opacities like cataract on threshold sensitivities and MD.16, 17, 18 Unlike MD, the new global index, VFI has been reported to be less affected by cataract.2 We too have reported the effect of cataract on VFI previously, and found that nuclear cataracts had little effect on VFI while the posterior subcapsular cataracts tended to influence it.19 In the current study, we found that the agreement between the event-based and the trend-based analyses to determine progression was only moderate. Our results are similar to that by Casas-Llera et al,11 who also found the agreement between event-based GPA and trend-based VFI analysis to be 0.48. There, however, were a few differences between our study and the study by Casas-Llera, et al.11 They defined progression on trend-based analysis as any negative VFI slope with a P-value of <0.05. We, in addition to the P-value, also considered the magnitude of slope while defining progression. Though the test–retest variability of the slope of VFI is not known, we considered a slope magnitude of −1% per year as clinically significant. Comparing the results of our study with that of the study by Casas-Llera, we also found that no patients in the study by Casas-Llera had progression detected by the trend-based analysis when the event-based analysis indicated stability. In contrast, we found that 11 of 101 eyes with the sensitive criteria and 12 of 131 eyes with the specific criteria showed progression on trend-based analysis when the event-based analysis indicated stability. The not so good agreement between the two approaches, though both the methods are based on the same functional test, is because of the way each determines progression. VFI is a global index, which is center weighted and so less weight is given to changes happening in peripheral points. GPA requires the change to be consistent at the same locations and so can miss early changes at the other locations. The not so good agreement may also be due to the pattern of glaucomatous VF progression. Studies have shown that VF progression in glaucoma is focal, with either enlargement or deepening of an existing scotoma.20, 21 VFI being a global index is less sensitive to focal progression because of the ‘diluting’ effect of relative stability noted elsewhere in the VF. Future studies should evaluate if trend-based analyses evaluating focal areas, like the pointwise linear regression, show a better agreement with GPA.
Of the two methods, GPA has been better validated than the recently introduced VFI-based trend-based analysis and has been shown to be comparable to objective clinical assessment of VFs for progression.15 We therefore considered GPA as the standard and evaluated the diagnostic accuracy of the new trend-based analysis to determine VF progression. We found that the trend-based analysis had a high specificity of around 90% to determine progression. Very few eyes had VF progression on the trend-based analysis when the event-based analysis indicated stability. The sensitivity of trend-based analysis to determine progression was, however, lower and was only around 60%.
In eyes judged as progressing by both the methods, we evaluated the time to detect progression by each of the methods to determine which method detected progression early. Though the event-based analysis detected progression slightly earlier than the trend-based method, this was not statistically significant. Earlier studies have found that the event-based analysis detected progression significantly earlier than trend-based methods.8, 11 We might have failed to detect a significant difference in time to progression between the methods because of our sample size. It may also be because of our practice of getting frequent VF tests done in subjects suspected to be progressing. Though the median number of VFs done per year in our patients was 1 (IQR: 0.8–1.3), the range was from 0.5 to 3, which meant that some patients had VFs done once in 2 years and some had three VFs in a year. It is important to note here that glaucoma progression is a time related function with most patients showing evidence of VF progression if tested frequently enough and long enough.8, 22 However, the frequency of VFs performed in any patient depends on the level of suspicion for progression, and with the trend-based methods especially, depends on the variability of the monitored VF parameter and the amount of change in the parameter that is clinically significant.23
The important limitation of this study and in general of studies comparing event- and trend-based progression analyses is the dependency of the results on the criteria used to define progression. On the trend-based analysis, we defined progression as any negative slope worse than −1% per year with a P-value of <5%. Most of the previous studies evaluating trend-based analyses have ignored the magnitude of the slope and only considered the P-value associated with it.11, 24, 25, 26 Our approach appears to be less sensitive (and more specific) than other studies. Employing a criterion that did not consider the magnitude of the slope could have increased the sensitivity (at the cost of specificity) of the analysis to detect progression.
In conclusion, the agreement between event-based and trend-based analysis provided by the Guided Progression Analysis software to determine VF progression was only moderate. Considering the event-based analysis results as standard, the trend-based analysis of VFI had a high specificity but a low sensitivity to determine VF progression. Event-based GPA seemed to detect progression earlier than trend-based analysis, but this wasn’t statistically significant.

References
Leske MC, Heijl A, Hyman L, Bengtsson B . Early Manifest Glaucoma Trial: design and baseline data. Ophthalmology 1999; 106: 2144–2153.
Bengtsson B, Heijl A . A visual field index for calculation of glaucoma rate of progression. Am J Ophthalmol 2008; 145: 343–353.
Rao HL, Kumar AU, Babu JG, Senthil S, Garudadri CS . Relationship between severity of visual field loss at presentation and rate of visual field progression in glaucoma. Ophthalmology 2011; 118: 249–253.
Rao HL, Addepalli UK, Jonnadula GB, Kumbar T, Senthil S, Garudadri CS . Relationship between intraocular pressure and rate of visual field progression in treated glaucoma. J Glaucoma 2012 e-pub ahead of print 16 May 2012; doi:10.1097/IJG.0b013e318259b0c2.
Anderson DR, Patella VM . Automated Static Perimetry 2nd edn. Mosby: St. Louis, MO, USA, 1999.
Fleiss JL . Statistical Methods for Rates and Proportions. Wiley: New York, NY, USA, 1981; 212–236.
Landis JR, Koch GG . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Vesti E, Johnson CA, Chauhan BC . Comparison of different methods for detecting glaucomatous visual field progression. Invest Ophthalmol Vis Sci 2003; 44: 3873–3879.
Werner EB, Bishop KI, Koelle J, Douglas GR, LeBlanc RP, Mills RP et al. A comparison of experienced clinical observers and statistical tests in detection of progressive visual field loss in glaucoma using automated perimetry. Arch Ophthalmol 1988; 106: 619–623.
Katz J, Congdon N, Friedman DS . Methodological variations in estimating apparent progressive visual field loss in clinical trials of glaucoma treatment. Arch Ophthalmol 1999; 117: 1137–1142.
Casas-Llera P, Rebolleda G, Munoz-Negrete FJ, Arnalich-Montiel F, Perez-Lopez M, Fernandez-Buenaga R . Visual field index rate and event-based glaucoma progression analysis: comparison in a glaucoma population. Br J Ophthalmol 2009; 93: 1576–1579.
Diaz-Aleman VT, Anton A, de la Rosa MG, Johnson ZK, McLeod S, Azuara-Blanco A . Detection of visual-field deterioration by glaucoma progression analysis and threshold noiseless trend programs. Br J Ophthalmol 2009; 93: 322–328.
Bergea B, Bodin L, Svedbergh B . Impact of intraocular pressure regulation on visual fields in open-angle glaucoma. Ophthalmology 1999; 106: 997–1004 discussion 1004–1005.
Gardiner SK, Crabb DP . Examination of different pointwise linear regression methods for determining visual field progression. Invest Ophthalmol Vis Sci 2002; 43: 1400–1407.
Arnalich-Montiel F, Casas-Llera P, Munoz-Negrete FJ, Rebolleda G . Performance of glaucoma progression analysis software in a glaucoma population. Graefes Arch Clin Exp Ophthalmol 2009; 247: 391–397.
Koucheki B, Nouri-Mahdavi K, Patel G, Gaasterland D, Caprioli J . Visual field changes after cataract extraction: the AGIS experience. Am J Ophthalmol 2004; 138: 1022–1028.
Carrillo MM, Artes PH, Nicolela MT, LeBlanc RP, Chauhan BC . Effect of cataract extraction on the visual fields of patients with glaucoma. Arch Ophthalmol 2005; 123: 929–932.
Rehman Siddiqui MA, Khairy HA, Azuara-Blanco A . Effect of cataract extraction on SITA perimetry in patients with glaucoma. J Glaucoma 2007; 16: 205–208.
Rao HL, Jonnadula GB, Addepalli UK, Senthil S, Garudadri CS . Effect of cataract extraction on visual field index in Glaucoma. J Glaucoma 2013; 22: 164–168.
Boden C, Blumenthal EZ, Pascual J, McEwan G, Weinreb RN, Medeiros F et al. Patterns of glaucomatous visual field progression identified by three progression criteria. Am J Ophthalmol 2004; 138: 1029–1036.
Pascual JP, Schiefer U, Paetzold J, Zangwill LM, Tavares IM, Weinreb RN et al. Spatial characteristics of visual field progression determined by Monte Carlo simulation: diagnostic innovations in glaucoma study. Invest Ophthalmol Vis Sci 2007; 48: 1642–1650.
Heijl A, Leske MC, Bengtsson B, Bengtsson B, Hussein M . Early Manifest Glaucoma Trial G. Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Ophthalmol Scand 2003; 81: 286–293.
Chauhan BC, Garway-Heath DF, Goni FJ, Rossetti L, Bengtsson B, Viswanathan AC et al. Practical recommendations for measuring rates of visual field change in glaucoma. Br J Ophthalmol 2008; 92: 569–573.
Ang GS, Mustafa MS, Scott N, Diaz-Aleman VT, Azuara-Blanco A . Perimetric progression in open angle glaucoma and the visual field index (VFI). J Glaucoma 2011; 20: 223–227.
Katz J, Gilbert D, Quigley HA, Sommer A . Estimating progression of visual field loss in glaucoma. Ophthalmology 1997; 104: 1017–1025.
Smith SD, Katz J, Quigley HA . Analysis of progressive change in automated visual fields in glaucoma. Invest Ophthalmol Vis Sci 1996; 37: 1419–1428.
Acknowledgements
This work was supported by Hyderabad Eye Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Rao HL is a consultant to Allergen. Garudadri CS is a consultant to Allergen, Alcon, and Merck. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rao, H., Kumbar, T., Kumar, A. et al. Agreement between event-based and trend-based glaucoma progression analyses. Eye 27, 803–808 (2013). https://doi.org/10.1038/eye.2013.77
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.77
Keywords
This article is cited by
-
A deep learning model incorporating spatial and temporal information successfully detects visual field worsening using a consensus based approach
Scientific Reports (2023)
-
Long-term evaluation of ocular hypertension with primary angle closure and primary open angles
International Ophthalmology (2019)
-
Comparison of visual field progression between temporally tilted disc and nontilted disc, in patients with normal tension glaucoma
Eye (2015)
-
Evaluation of Visual Field Progression in Glaucoma
Current Ophthalmology Reports (2014)