Abstract
Purpose
To compare the diagnostic efficacy of wide-field digital retinal imaging (WFDRI) with binocular indirect ophthalmoscopy (BIO) for retinopathy of prematurity (ROP) screening.
Methods
Premature infants admitted for ROP screening were included in this prospective, randomized and double-blind comparative study. They were examined by using BIO and WFDRI.
Results
A total of 58 infants were enrolled in the study. The sensitivities of WFDRI in detecting any stage of ROP, treatment-requiring ROP and plus disease were 58.6, 100, and 100% respectively, with a specificity of 100% for all. The proportional agreement between WFDRI and BIO was 0.903 for detection of any stage of ROP, 1.0 for treatment-requiring ROP, and 1.0 for plus disease.
Conclusion
The sensitivity and specificity of WFDRI was excellent for the diagnosis of severe and treatment-requiring ROP. However, BIO was superior in mild ROP particularly for the ones in retinal periphery.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is one of the major causes of preventable childhood blindness. As early detection and treatment of threshold and high-risk prethreshold ROP have shown to significantly decrease the incidence of severe vision loss,1, 2 screening of high-risk premature infants is critical. American Academy of Pediatrics, American Academy of Ophthalmology, and American Association for Pediatric Ophthalmology and Strabismus state that infants with a birth weight of <1500 g or gestational age of ≤32 weeks and selected infants with a birth weight between 1500 and 2000 g or gestational age of >32 weeks with an unstable clinical course should be screened in order to detect ROP, which should be performed following pupillary dilation by using binocular indirect ophthalmoscopy (BIO).3
The conventional method, which is also accepted as the gold standard, for ROP screening is BIO with scleral indentation. ROP screening with this technique is difficult, particularly in developing countries, because it requires a specialized pediatric ophthalmologist experienced in ROP screening. Wide-field digital retinal imaging (WFDRI) is an alternative method for imaging the retina of prematures, and it has begun to be used widely for ROP screening.
The aim of the present study was to evaluate the diagnostic efficacy of WFDRI in detecting the severity (stage), localization (zone), and activity (plus disease) of ROP, and to compare these data with those of the BIO.
Materials and methods
This prospective, randomized, double-blind comparative study was carried out in ROP Screening, Treatment and Training Center of Etlik Zubeyde Hanim Maternity and Research Hospital in full accord with the principles laid out in the Declaration of Helsinki, upon approval of the Institutional Review Board. Consecutive infants admitted for routine ROP screening examination and born with a gestational age of <32 weeks or with a birth weight of <1500 g, as well as older and heavier infants with an unstable clinical course who were believed to be at high risk for ROP by their neonatologist, were recruited in the study. Verbal and written informed consent was obtained from parents. Infants with systemic malformations, structural ocular abnormalities beside ROP, and the ones with a previous history of laser photocoagulation or ocular surgery were all excluded from the study. The rendered data included the birth weight, gender, gestational age and age at screening examination, and the findings of consecutive BIO and WFDRI examinations.
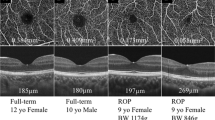
The schedule for the timing of initial screening examination and follow-up examinations, and the time to stop screening examinations were determined according to the recommendations of American Academy of Pediatrics, American Academy of Ophthalmology, and American Association for Pediatric Ophthalmology and Strabismus.3 Screening was performed by one of the two experienced pediatric ophthalmologists (MAS and EH). Each infant underwent a BIO examination by one of the authors (EH) for each eye with a 28 D condensing lens and scleral depression following a pupillary dilation, which was achieved with 2.5% phenylephrine and 0.5% tropicamide and after instillation of topical anesthetic proparacaine and application of an eyelid speculum. Following BIO examination, retinal photos were taken by another author (MAS), who was masked for the findings of BIO, by using wide-field digital retinal camera attached with a 130-degree field ROP lens (RetCam Shuttle, Clarity Medical Systems, Pleasanton, CA, USA). At least three photos, including the posterior pole, the temporal, and the nasal retina, were taken from each eye. The images were stored on the hard drive of RetCam Shuttle. The presence or absence of the ROP and plus disease and the zone, stage, and the extent of the ROP, if present, were separately recorded by each examiner according to the international classification of ROP (ICROP).4 Screening and data recruitment was continued until the retinal vasculature was mature or until the infant required treatment.
The findings were analyzed and recorded by each author separately and regrouped for easier analysis based on the established criteria of Early treatment of ROP study (ETROP) and ICROP as follows:
Group A: no ROP (either completed retinal vascularization or not)
Group B: ROP less severe than high-risk prethreshold ROP (type 1 prethreshold ROP), which was defined in ETROP
Group C: high-risk prethreshold ROP (type 1 prethreshold ROP) of ETROP study
Group D: threshold ROP, which was defined in Cryotherapy for ROP study (CRYO-ROP study)
Group E: aggressive posterior ROP (APROP)
Group C, D and E regrouped as ‘treatment-requiring ROP’
Statistical analysis was performed by using SPSS software for Windows 15.0 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA). The sensitivity and specificity for WFDRI in detecting any stage of ROP, plus disease, and treatment-requiring ROP was determined by using the BIO findings as the gold standard. The Kappa coefficient and the proportional agreement were used to examine the level of agreement between two different methods of screening. Median and range were given as descriptive statistics for quantitative data. Categorical data were summarized using frequency and percentages. Independent samples t-test was used to compare two independent groups with normal distribution of quantitative data and Mann–Whitney test for abnormal distribution. Result was accepted as statistically significant when P was <0.05.
Results
A total of 58 infants (33 male, 25 female) who were admitted to our clinic for ROP screening between March 2012 and April 2012 were included in the study. Gestational age of those infants at birth ranged from 24 to 32 weeks, with a median gestational age of 30 weeks. Birth weight ranged from 760 to 2000 g, with a median weight of 1335 g. Eighteen (31%) of the infants developed any stage of ROP and eight (13.8%) required laser photocoagulation during follow-up. Seventeen infants were screened once, 22 infants twice, 14 infants thrice, four infants four times, and one infant was screened five times during the study period. A total of 124 eye examinations were carried out bilaterally; therefore, findings of 248 eyes were analyzed. Screening examinations were performed between 4th and 16th weeks of their life (median chronological age was 6 weeks), and at a postmenstrual age of 32 to 41 weeks (median postmenstrual age is 35 weeks). No BIO or WFDRI examinations had to be aborted because of infant stress (1–2 min were spent for imaging of each eye with both techniques).
Sixteen eyes of eight patients with plus disease and those who had treatment-requiring ROP were all detected by WFDRI (with 100% sensitivity, 100% specificity, 1.0 proportional agreement and 1.0 kappa value). Diagnostic accuracy of WFDRI for detecting ROP with respect to zones, stages and severity were summarized in Tables 1, 2, 3.
Discussion
The improvement in the survival rate of very premature babies and increased need of ophthalmologists skilled in ROP care resulted in a tendency towards digital imaging in ROP screening.5 For this purpose, we analyzed the efficacy of WFDRI in detecting any stage of ROP, treatment-requiring ROP and plus disease and we also compared these results with those of the BIO, which is accepted as the current gold standard method for ROP screening. The sensitivities of WFDRI in detecting any stage of ROP, treatment-requiring ROP and plus disease were 58.6, 100, and 100%, respectively, with a specificity of 100% for all. The proportional agreement between WFDRI and BIO was 0.903 for detecting any-stage ROP, 1.0 for treatment-requiring ROP, and 1.0 for plus disease.
Previous studies have also evaluated WFDRI for detecting ROP. Schwartz et al6 reported a suboptimal efficacy that may be related to the older camera model (RetCam 120) used for screening. Our results are comparable with the newer studies that are focused on detecting severe ROP. Wu et al7 evaluated 43 premature infants and reported a 100% sensitivity and a 97.5% specificity in detecting prethreshold and threshold ROP. Dai et al8 screened 108 premature infants and found a sensitivity of 100% and a specificity of 97.9% in detecting infants with treatment-requiring ROP. Dhaliwal et al9 analyzed 245 eye examinations of 81 infants. They reported that the sensitivities of WFDRI in detecting any stage of ROP, stage 3 ROP and plus disease were 60, 57, and 80%, respectively, and the specificities were 91, 98, and 98%, respectively. They found that the proportional agreement between WFDRI and BIO was 0.96 for detecting stage 3 disease and 0.97 for plus disease.
The reported sensitivity of 58.6% for detecting any stage of ROP in our study demonstrates that only 58.6% of infants with any stage of ROP can be detected with WFDRI. Nevertheless, a specificity of 100% means that no unnecessary referrals would happen within this group of patients. A hundred-percent sensitivity for detecting treatment-requiring ROP means that all infants with ROP requiring treatment would be promptly detected and referred for treatment, and a 100% specificity means that no unnecessary referrals would occur.
After the revised guidelines of ETROP study have emerged,2 plus disease has started to become the most important criteria for making the decision on treatment. This makes the examination of posterior retinal blood vessels more important during ROP screening. WFDRI has been found to be as sensitive as BIO in the detection of plus disease, which makes its use logical for ROP screening. ROP that requires treatment necessitates either zone I disease or plus disease, both are shown to be imaged easily with WFDRI. Therefore, it is rational to use WFDRI in the diagnosis of treatment-requiring ROP.
There are some advantages and disadvantages of both techniques. Advantages of BIO include better visualization of funds details by a well-trained ophthalmologist, whereas disadvantages consist of technical difficulty and time constraints of the ophthalmologist. Therefore, examination with BIO may be logistically difficult for neonatologists, especially in units where access to experienced ophthalmologists for ROP screening is not available. Also, scleral depression required during BIO may cause systemic complications such as bradycardia secondary to oculocardiac reflex10 and may cause some ophthalmic complications such as vitreous and subretinal hemorrhages.11 WFDRI can be advantageous in that it may be performed by a skilled technician and provides more flexibility in scheduling. When ophthalmic examination for screening of ROP is performed with WFDRI, infants experience less pain and stress compared with those who were examined with BIO12, but WFDRI can cause several ophthalmic complications such as retinal hemorrhages as well.13 More accurate documentation obtained with WFDRI may provide greater protection against medicolegal problems.14 Disadvantages of WFDRI include limitations of diagnosis of ROP, especially for mild and peripheral diseases and high initial cost of the equipment.
With regard to our findings, the peripheral retina could be visualized much more easily with BIO when compared to WFDRI. Visualization of the peripheral retina was inadequate probably due to technical limitations, particularly, the big camera size when compared with premature infant globe size. In our point of view, this problem can be overcome with the development of smaller-sized cameras that enables movement and rotation to see retinal periphery.
Difficulty of peripheral retinal examinations with WFDRI causes a secondary problem: when to stop ROP screening? Visualization of normal vascularization in zone 3 periphery was much more easily detected with BIO, which might result in an easier decision to discontinue screening for ROP. If only WFDRI was used for screening, uncertainty about the end-point of screening would require a prolonged course of screening for each infant. In the study of Dhaliwal et al,9 BIO was found to be superior to WFDRI in making decisions for discharging infants from ROP screening. They suggested that it may be more efficient to perform final discharge examination of an infant using BIO, even if WFDRI was used for earlier examinations. In order to fully assess whether the retina of an infant is completely vascularized or not, a BIO examination should be performed at least once, even prior to discharge from screening program.
The present study should be viewed in the context of some limitations. First of all, small number of infants and usage of eye as the unit of statistical analysis may influence the power of statistical outcomes. Secondly, as we examined a consecutive series of infants, a relatively high proportion of them had mild or no ROP. Therefore, this imbalance may partially explain the relative low sensitivity results in terms of detection of any stage of ROP. Finally, experience of the examiner may influence the outcomes. As ophthalmologists are more familiar in the use of BIO when compared with WFDRI, there may be a learning curve for mastering WFDRI techniques and, thus, a more experienced screener of ROP may obtain better results with WFDRI. Experienced screeners may not be able to see retinal periphery with WFDRI, even if they spend additional time and induce additional stress in the infants for documenting peripheral ROP. Despite all these limitations of the current study, there are important implications regarding the accuracy of WFDRI in terms of ROP screening. In light of the present data, we can suggest that this study is critical for developing some screening strategies with WFDRI before its incorporation into the routine ROP screening. A well-organized strategy for ROP screening with WFDRI may reduce the overall number of BIO examinations required.
In conclusion, although small number of patients limits the generalizability of the study, WFDRI showed relatively low sensitivity in detecting mild and peripherally located forms of ROP, but it was accurate, reliable and efficient in detecting severe and treatment-requiring ROP, which points to the fact that none of the infants who required treatment for ROP were missed with WFDRI examination. WFDRI imaging cannot completely replace BIO. Instead, WFDRI can be used as an adjunctive method to, rather than as a replacement for BIO in ROP screening.

References
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter Trial of Cryotherapy for Retinopathy of Prematurity: ophthalmological outcomes at 10 years. Arch Ophthalmol 2001; 119: 1110–1118.
Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the Early Treatment for Retinopathy of Prematurity randomized trial. Arch Ophthalmol 2003; 121: 1684–1694.
Section on Ophthalmology American Academy of Pediatrics; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2006; 117: 572–576.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123: 991–999.
Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A . Retinopathy of prematurity in middle-income countries. Lancet 1997; 350: 12–14.
Schwartz SD, Harrison SA, Ferrone PJ, Trese MT . Telemedical evaluation and management of retinopathy of prematurity using a fiberoptic digital fundus camera. Ophthalmology 2000; 107: 25–28.
Wu C, Petersen RA, VanderVeen DK . RetCam imaging for retinopathy of prematurity screening. J AAPOS 2006; 10: 107–111.
Dai S, Chow K, Vincent A . Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Exp Ophthalmol 2011; 39: 23–29.
Dhaliwal C, Wright E, Graham C, McIntosh N, Fleck BW . Wide-field digital retinal imaging versus binocular indirect ophthalmoscopy for retinopathy of prematurity screening: a two-observer prospective, randomised comparison. Br J Ophthalmol 2009; 93: 355–359.
Laws DE, Morton C, Weindling M, Clark D . Systemic effects of screening for retinopathy of prematurity. Br J Ophthalmol 1996; 80: 425–428.
Mavrofrides EC, Berrocal AM, Murray TG . Development of multiple subretinal hemorrhages during diode laser supplementation for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 2006; 43: 110–113.
Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF . Telemedicine for retinopathy of prematurity diagnosis: evaluation and challenges. Surv Ophthalmol 2009; 54: 671–685.
Adams GG, Clark BJ, Fang S, Hill M . Retinal haemorrhages in an infant following RetCam screening for retinopathy of prematurity. Eye (Lond) 2004; 18: 652–653.
Trese MT . What is the real gold standard for ROP screening? Retina 2008; 28: S1–S2.
Acknowledgements
The study was conducted in Etlik Zubeyde Hanim Maternity and Women’s Health Research Hospital, Department of Ophthalmology, Ankara, Turkey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sekeroglu, M., Hekimoglu, E., Sekeroglu, H. et al. Alternative methods for the screening of retinopathy of prematurity: binocular indirect ophthalmoscopy vs wide-field digital retinal imaging. Eye 27, 1053–1057 (2013). https://doi.org/10.1038/eye.2013.128
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.128
Keywords
This article is cited by
-
Diagnostic Accuracy of Pediatrician-performed Digital Retinal Imaging with 3nethra neo for ROP Screening
Indian Journal of Pediatrics (2024)
-
Retinopathy of prematurity detection: a retrospective quality improvement project before-after implementation of retinal digital imaging for screening
European Journal of Pediatrics (2023)
-
Neonatal eye screening for 203 healthy term new-borns using a wide-field digital retinal imaging system
BMC Ophthalmology (2021)
-
Development of 3D Printed Smartphone-Based Multi-Purpose Fundus Camera (MultiScope) for Retinopathy of Prematurity
Annals of Biomedical Engineering (2021)