Abstract
Purpose
To evaluate the effects of intravitreal autologous plasmin enzyme (APE) in patients with focal vitreomacular traction (VMT).
Methods
APE was obtained by incubation of patient-derived purified plasminogen with streptokinase, and intravitreally injected 5–12 days later. Twenty-four hours after injection, in case of incomplete VMT release, a pars plana vitrectomy was performed. The hyaloid internal limiting membrane adherence and removal of the posterior hyaloid were intraoperatively evaluated.
Results
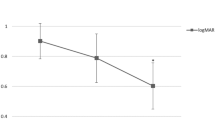
Thirteen patients were recruited. During preparation of APE, five patients had spontaneous release of VMT. Eight patients received APE injection (2 IU). In five patients, spontaneous resolution of VMT occurred before APE administration. Twenty-four hours after injection, persistence of VMT was detected in all the eight treated patients. Best-corrected visual acuity was 0.51±0.37 LogMAR at baseline, improving to 0.23±0.14 LogMAR at 6 months (P=0.002). Foveal thickness was 464±180 μm at baseline, reducing to 246±59 μm at 6 months (P<0.001). Hyaloid was intraoperatively judged ‘partially detached’ in seven cases and ‘totally detached’ in one case. Hyaloid peeling was evaluated ‘easy’ in six eyes and ‘very easy’ in two eyes.
Conclusions
In the current study, there was a large percentage of spontaneous resolution of VMT before an APE administration. A single intravitreal APE injection seems insufficient to induce a complete posterior vitreous detachment in these patients.
Similar content being viewed by others
Introduction
In some patients, incomplete posterior vitreous detachment (PVD) occurs causing vitreomacular traction (VMT). In several studies,1, 2, 3, 4, 5, 6 PVD has been reported using intravitreal plasmin, a serine nonspecific protease, which is able to degrade fibrin, laminin, and fibronectin,7 binding the vitreous cortex to the internal limiting membrane (ILM).
In this study, we evaluated the effects of intravitreal autologous plasmin enzyme (APE) in patients with focal VMT syndrome.
Materials and methods
In this prospective interventional case series, we investigated the effects of intravitreal APE in patients affected by focal VMT that presented consecutively between January and December 2010. Inclusion criteria were age >18 years, best-corrected visual acuity (BCVA) <20/40, and presence of a focal VMT (defined as incomplete PVD with part of posterior hyaloids attached to the macular area). Exclusion criteria were presence of any coincident ocular disease, previous retinal treatment in the study eye, and optical media opacities. All patients underwent a complete ophthalmological evaluation at baseline (before surgery). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
APE was obtained by incubation of patient-derived purified plasminogen with streptokinase. A quantity of 0.05–0.2 ml containing 2 IU of APE was intravitreally injected 5–12 days later. Twenty-four hours after the APE injection, all patients underwent a complete ophthalmological evaluation, including spectral-domain optical coherence tomography (SD-OCT) and ultrasound scan, to assess the effects of the enzyme and to check for adverse events. In case of incomplete release of the VMT, PPV was performed on the same day by a single surgeon (MC). The surgeon intraoperatively evaluated and recorded the status of the vitreous and the posterior hyaloid-ILM adherence. The entity of the posterior hyaloid detachment was classified as ‘totally adherent’, ‘partially detached’, or ‘totally detached’.6 The surgical removal of the posterior hyaloid was judged as ‘difficult’, ‘easy’, or ‘very easy’.6 All patients underwent a complete ophthalmological examination at 1, 3, and 6 months after APE injection+/−vitrectomy.
SD-OCT images were obtained using the Spectral OCT-SLO (OPKO/OTI Ophthalmic Technologies Inc., Toronto, Canada), and macular thickness was calculated (ILM and RPE lines automatically identified). Macular sensitivity was measured with the MP-1 Microperimeter (Nidek Technologies, Padova, Italy).
Statistical calculations were performed using GraphPad Prism version 5.00 for Mac (GraphPad Software, San Diego, CA USA). One-way ANOVA was performed to compare means of BCVA (LogMAR), macular thickness, and macular sensitivity during follow-up. The chosen level of statistical significance was P<0.05.
Results
Thirteen patients were enrolled (Table 1). In five patients, during the time required for APE preparation (mean 26.2±3.3 days; range 20–32 days), a spontaneous resolution of VMT was detected. Therefore, only 8 out of the 13 studied patients underwent intravitreal APE. No injection-related complications were reported.
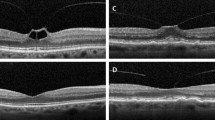
Twenty-four hours after APE injections, persistence of VMT was detected by fundus biomicroscopy and SD-OCT in all the eight patients. However, in one out of eight patients, SD-OCT showed a weakening of the VMT (Figure 1).
Preoperative and postoperative SD-OCT of patient no. 6. SD-OCT scan before intravitreal APE injection (a) showing the VMT. SD-OCT scan 24 h after APE injection showing a weakening of the VMT and a downshift of the detached small retinal fragment with partial restoration of the foveal contour (b). SD-OCT scans 1 month (c) and 6 months (d) after pars plana vitrectomy showing progressive restoration of the foveal contour.
As per protocol, all injected patients also underwent PPV. Posterior hyaloid was ‘partially detached’ in seven out of eight cases and ‘totally detached’ in one case. Posterior hyaloid peeling was ‘easy’ in six out of eight eyes and ‘very easy’ in two out of eight eyes.
BCVA was 0.51±0.37 LogMAR (≈20/63) at baseline and improved to 0.33±0.18 LogMAR (≈20/40), 0.28±0.17 LogMAR (≈20/32), and 0.23±0.14 LogMAR (≈20/32) at 1, 3, and 6 months after surgery (P=0.002), respectively (Figure 2). Retinal foveal thickness was 464±180 μm at baseline and improved to 238±70, 225±61, and 246±59 μm at 1, 3, and 6 months after surgery (P<0.001), respectively (Figure 3). Macular sensitivity in the fovea-centered 8° was 13.8±3.6 dB at baseline and improved to 14.4±3.2, 14.4±3.5, and 13.6±3.9 dB at 1, 3, and 6 months after surgery (P=0.48), respectively.
Discussion
In this study, we evaluated the effects of intravitreal injection of APE on focal VMT. We waited 24 h in order to enhance enzyme activity.2 None of the injected patients obtained a complete resolution of the VMT. However, benefits of APE were suggested by the intrasurgical evaluation of the vitreous cortex adherence. We hypothesize that, in our series, a single injection of APE may have not succeeded in releasing the VMT because of an early enzyme consumption (before reaching the posterior vitreoretinal interface).
To the best of our knowledge, this is the first study investigating intravitreal injection of APE in eyes affected by focal VMT, which makes difficult any comparison with previous published series.
Limitations of the current study are the lack of a control group, and the unmasked subjective evaluation of posterior hyaloid peeling. Further studies are needed to evaluate particularly if repeated injections of APE could succeed in releasing the focal VMT, and improving the surgical outcomes.
In conclusion, a single intravitreal APE injection seems to be insufficient to induce a complete PVD in patients affected by focal VMT.

References
Lopez-Lopez F, Rodriguez-Blanco M, Gómez-Ulla F, Marticorena J . Enzymatic vitreolysis. Curr Diab Rev 2009; 5: 57–62.
Verstraeten TC, Chapman C, Hartzer M, Winkler BS, Trese MT, Williams GA . Pharmacologic induction of posterior vitreous detachment in the rabbit. Arch Ophthalmol 1993; 111: 849–854.
Li X, Shi X, Fan J . Posterior vitreous detachment with plasmin in the isolated human eye. Graefes Arch Clin Exp Ophthalmol 2002; 240: 56–62.
Hikichi T, Yanagiya N, Kado M, Akiba J, Yoshida A . Posterior vitreous detachment induced by injection of plasmin and sulfur hexafluoride in the rabbit vitreous. Retina 1999; 19: 55–58.
Gandorfer A, Putz E, Welge-Lüssen U, Grüterich M, Ulbig M, Kampik A . Ultrastructure of the vitreoretinal interface following plasmin assisted vitrectomy. Br J Ophthalmol 2001; 85: 6–10.
Azzolini C, D'Angelo A, Maestranzi G, Codenotti M, Della Valle P, Prati M et al. Intrasurgical plasmin enzyme in diabetic macular edema. Am J Ophthalmol 2004; 138: 560–566.
Liotta LA, Goldfarb RH, Brundage R, Siegal GP, Terranova V, Garbisa S . Effect of plasminogen activator (urokinase), plasmin, and thrombin on glycoprotein and collagenous components of basement membrane. Cancer Res 1981; 41: 4629–4636.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Codenotti, M., Maestranzi, G., De Benedetto, U. et al. Vitreomacular traction syndrome: a comparison of treatment with intravitreal plasmin enzyme vs spontaneous vitreous separation without treatment. Eye 27, 22–27 (2013). https://doi.org/10.1038/eye.2012.248
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.248
Keywords
This article is cited by
-
The design and validation of an optical coherence tomography-based classification system for focal vitreomacular traction
Eye (2016)
-
A novel spectral-domain optical coherence tomography model to estimate changes in vitreomacular traction syndrome
Graefe's Archive for Clinical and Experimental Ophthalmology (2014)
-
Vitreomacular traction syndrome: the role of intravitreal plasmin injection is still not clear
Eye (2013)
-
Comment on ‘Vitreomacular traction syndrome: a comparison of treatment with intravitreal plasmin enzyme vs spontaneous vitreous separation without treatment’
Eye (2013)
-
Reply to Grzybowski and Ascaso
Eye (2013)