Abstract
Purpose
To compare the intraocular pressure (IOP) after 23-gauge transconjunctival sutureless vitrectomy (TSV) and conventional 20-gauge vitrectomy for various vitreoretinal diseases.
Methods
This was a retrospective interventional case series including 338 cases of 23-gauge TSV and 476 cases of 20-gauge vitrectomy with minimum follow-up period of 1 month. Postoperative 1 day, 1 week and 1 month IOPs were compared. Multiple regression analysis to assess the actual effect of gauge of vitrectomy on postoperative IOP was performed including intraoperative and postoperative factors influencing postoperative IOP as covariates.
Results
The mean IOP of 20-gauge vitrectomy was significantly higher than that of 23-gauge TSV (20.6±8.02 mm Hg vs12.8±4.48 mm Hg, P<0.001) at postoperative day 1, but the differences were not significant at postoperative 1 week and 1 month. The IOP pattern of 23-gauge TSV demonstrated more stable course than that of 20-gauge vitrectomy. At 1 day post vitrectomy, the incidence of hypertony was higher in 20-gauge, whereas that of hypotony was higher in 23-gauge. Among risk factors, the 20-gauge vitrectomy showed the strongest association with postoperative 1 day IOP rise.
Conclusion
Twenty-three-gauge TSV has stable and lower IOP in the early postoperative period than the 20-gauge vitrectomy. In patients whose retina and optic nerves are vulnerable to higher or fluctuating IOP, 23-gauge TSV may be more beneficial.
Similar content being viewed by others
Introduction
Small incision transconjunctival sutureless vitrectomy (TSV), 25- and 23-gauge vitrectomy, is widely performed among retinal surgeons for reduced operation time, patient comfort, and earlier postoperative recovery, compared with 20-gauge conventional vitrectomy. Twenty-five-gauge TSV was introduced by Fujii et al1 and despite numerous beneficial features, it confers several disadvantages such as limited surgical instrument usage, a flexible cutter which sets limits on surgical approaches to the peripheral retina and vitreous, and a longer time for vitreous removal.2, 3
Subsequently, 23-gauge TSV was introduced by Eckardt et al4 to combine the beneficial features of both the 20- and 25-gauge vitrectomy systems.3 As it has only recently been developed, studies on the efficacy and safety of 23-gauge TSV have been limited,5, 6, 7, 8, 9, 10, 11 and few comprehensive comparisons with conventional 20-gauge vitrectomy for limited indications of vitrectomy have been performed.12, 13
Specifically, in regard to postoperative hypotony or hypertony, although those are the major complications of vitrectomy, there have been few comparative studies with inconclusive number of patients. These studies were also limited in that only the intraocular pressure (IOP) at postoperative day 1 was studied and compared.12, 13 According to previous studies, the rate of wound leakage and hypotony in a small gauge sutureless system is supposed to be higher than that of 20-gauge conventional vitrectomy, but the difference has not been extensively evaluated through a direct comparison between the two gauges including various indications of vitrectomy and convincingly large number of patients.
Accordingly, the present study, which included 338 cases of 23-gauge TSV and 476 cases of 20-gauge vitrectomy, aimed to compare postoperative IOP between 20-gauge vitrectomy and 23-gauge TSV. In this comparison, various intraoperative factors affecting postoperative IOP were considered and the actual effect of gauge (23- vs 20-gauge) on postoperative IOP were analyzed.
Patients and methods
Patients and data collection
This was a single-center, single-surgeon, comparative, retrospective interventional case series. The medical records of 617 cases of 20-gauge vitrectomy and 479 cases of 23-gauge TSV operated from January 2004 to December 2007 were reviewed. Informed consent was obtained from patients before the operation, and the study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital. Inclusion criteria were as follows: (1) pars plana 20-gauge vitrectomy or 23-gauge TSV performed by a single surgeon (KHP); (2) first vitrectomy; (3) a minimum follow-up of 1 month; and (4) no serious postoperative complications affecting IOP before 1 month post-vitrectomy such as failed or recurred retinal detachment. A total of 282 cases failed to meet the inclusion criteria and were excluded from the study (141 cases in 20-gauge (42 cases for previous vitrectomy, 84 for missing data from follow-up loss, 15 for failed or recurred cases), and 23-gauge group (48 cases for previous vitrectomy, 83 for missing data from follow-up loss, 10 for failed or recurred cases)).
Finally, 338 cases of 23-gauge TSV from 324 patients and 476 cases of 20-gauge vitrectomy from 443 patients were included in the analysis. Preoperative data included patient's age, sex, indications of vitrectomy, previous ocular surgery, IOP, history of glaucoma, and current topical and oral medications. In addition, intraoperative data consisted of gas or silicone tamponade, combined cataract extraction, combined buckling or encircling surgery, intravitreal triamcinolone injection at the end of vitrectomy, and suture placement at conclusion of surgery.
Postoperative data contained IOP measured twice by Goldmann applanation tonometer and postoperative inflammation indicated by grades of cells in the anterior chamber at postoperative day 1, 7, and 30. Grading of cells, from 0+ to 4+, in the anterior chamber was evaluated with a slit beam of 2 mm length and 1 mm width under maximal light intensity and magnification (0+: ≤5, 1+: 6–15, 2+: 16–25, 3+: 26–50, 4+: >50 cells). In addition, the number of IOP-lowering topical medications at the time of measurement was inspected at postoperative day 7 and 30. In cases of 23-gauge TSV, IOPs at postoperative 2 and 5 h were measured. Hypotony and hypertony were defined as IOP <6 mm Hg and IOP >24 mm Hg, respectively.
Surgical methods
Both 23-gauge TSV and 20-gauge vitrectomies were performed using the same Accurus vitrectomy system (Alcon, Fort Worth, TX, USA) along with either 23- or 20-gauge instruments. Twenty-gauge vitrectomy was performed by the conventional method and 23-gauge TSV was performed using the method described by Eckardt.4 When a visually significant cataract was present, cataract extraction was performed before sclerotomy. When performing sclerotomy, oblique scleral tunnel wounds were created at an angle of ∼15°relative to the sclera. Twenty-three-gauge instruments were introduced through microcannulas during vitrectomy. In cases that required an internal tamponade, gas (18% SF6) or silicone oil (SO, Arciolane 1300 CS, Arcadophta Inc., Toulouse, France) were infused intravitreally. In cases in which SO was injected, sclerotomy was broadened with a 20-gauge microvitreoretinal blade to permit faster SO injection. After the injection, enlarged sclerotomy wounds were sutured.
At the end of 23-gauge TSV, microcannulas were removed without suture on either the sclera or conjunctiva. In order to promote wound sealing, a cotton-tip applicator was used to compress the sclerotomy sites three consecutive times for 20 s and to relocate the displaced conjunctiva to the original position. In 23-gauge TSV, the sclerotomy wound was sutured only in cases with any visible sign of leakage such as gas bubble from the sclerotomy sites, formation of conjunctival bleb, or ocular hypotony on tactile examination. However, in 20-gauge vitrectomy cases, suture placement was routinely performed on all sclerotomy wounds. After all these procedures of vitrectomy, the presence of intraoperative hypotony or hypertony was approximately checked with tactile examination. When low IOP was detected, intravitreal injection of balanced salt solution (BSS) in BSS-filled eyes, SO in SO-filled eyes, and SF6 gas in gas-filled eyes was performed until IOP became normotensive by tactile examination. Antibiotics and steroids were injected subconjunctivally and topical administration of 0.5% levofloxacin and 1% prednisolone were prescribed for 1 month.
Statistical analysis
Descriptive statistical analyses were performed on demographic data, indications for surgery, preoperative IOP, and intraoperative factors. The IOPs at postoperative day 1, 7, and 30 were compared between the 23- and 20-gauge groups using the Student's t-test. In order to explore the true effect of gauge on IOP (23- vs 20-gauge), additional analyses were performed to exclude possible confounding factors. First, one surgical indication (epiretinal membrane) of which the surgical technique is simple and identical between the two vitrectomies was selected. The postoperative IOP changes, defined as postoperative IOP minus preoperative IOP, at day 1, 7, and 30 were compared between 23- and 20-gauge vitrectomy using the Student's t-test. In order to exclude various possible confounding factors, all patients who underwent cataract surgery, encircling, or triamcinolone injection during vitrectomy were removed. Also, patients treated with silicone oil or gas and those with glaucoma were all removed in the comparison. Second, including various preoperative and intraoperative factors, multiple linear regression analysis was performed to elucidate the degree and significance of association between postoperative IOP and gauge of vitrectomy.
The incidence of hypotony and hypertony between 20-gauge vitrectomy and 23-gauge TSV was compared with the χ2 test. In order to reduce false positives attributable to multiple statistical tests, Bonferroni-adjusted P-values were used for evaluating statistical significance. Statistical analyses were performed using SPSS for Windows (Ver. 15.0, Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA).
Results
Clinical characteristics and surgical parameters are shown in Table 1. The frequency of intraoperative sclerotomy suture and combined cataract surgery were significantly different between the 20- and 23-gauge systems. Demographics, such as age and gender, and the use of tamponade with gas showed borderline significance between the two gauges of vitrectomy whereas silicone oil was used more frequently in 20-gauge vitrectomy (2.4% vs 7.4%, P=0.002). Regarding the indications of vitrectomy, the proportions of surgical indications were significantly different between 20-gauge and 23-gauge system in our study. However, there was no significant difference on preoperative IOP, the percentage of patients with preoperative glaucoma, and the number of postoperative IOP-lowering medications between 20-gauge and 23-gauge vitrectomy.
Figure 1 demonstrates the pattern of postoperative IOP in 20-gauge vitrectomy and 23-gauge TSV groups. The mean IOP was remarkably higher in the 20-gauge vitrectomy group at postoperative day 1 (20.6±8.02 vs 12.8±4.48 mm Hg) and the IOP change, calculated by postoperative IOP minus preoperative IOP, showed statistical difference between 20-gauge vitrectomy and 23-gauge TSV (7.5±8.4 vs 0.0±5.3 mm Hg, P<0.001 by Student's t-test) at the day. However, there were no significant differences in subsequent IOP changes between the two gauges (P=0.38 at postoperative day 7 and P=0.11 at postoperative day 30). An IOP spike was demonstrated in the 20-gauge vitrectomy group at postoperative day 1, whereas the IOPs in the 23-gauge TSV group remained stable for 1 month including the very early postoperative period such as postoperative 2 and 5 h.
Postoperative IOP changes after 20-gauge vitrectomy and 23-gauge transconjunctival sutureless vitrectomy. Error bars indicate 95% confidence interval. *IOP change, calculated by postoperative IOP minus preoperative IOP, was compared between the two gauges and the change was statistically significant only at postoperative 1 day (P<0.001 by Student’s t-test).
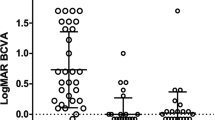
Postoperative IOP of ERM, in which the surgical technique is relatively simple with minimal variations, was compared between 20- and 23-gauge vitrectomy after removing cases with potential confounding factors on postoperative IOP. To exclude possible confounding factors, cases without preoperative glaucoma that underwent additional procedures such as cataract extraction, scleral buckling/encircling, intravitreal gas/silicone oil/triamcinolone injection, and intraoperative sclerotomy suture in 23-gauge TSV were excluded. Figure 2 demonstrates the IOPs before and after 23- (n=43) and 20- (n=34) gauge vitrectomy for ERM, and the IOP change was not significantly different between 20-gauge and 23-gauge vitrectomy except postoperative 1 day (2.3 vs −1.2 mm Hg, P=0.002 by Student's t-test), for which the comparison showed statistical significance.
In order to control the various clinical and surgical factors that may affect postoperative IOP, multiple regression analysis was performed with postoperative IOP as the outcome variable (Table 2). Clinical and surgical factors including age, sex, gauge of vitrectomy, silicone oil injection, gas tamponade, combined cataract extraction, combined buckling or encircling surgery, preoperative IOP, surgical indications, and intravitreal triamcinolone injection were analyzed. At postoperative day 1, the gauge of vitrectomy was the significant factor associated with postoperative increase of IOP showing the greatest coefficient (β) of linear regression. The 23-gauge TSV was significantly associated with a decrease in IOP by 7.31 mm Hg at postoperative 1 day independent of other clinical factors (P<0.001). However, the association was not significant at postoperative day 7 and 30 (β=−0.23, P=0.589 at postoperative day 7 and β=0.93, P=0.013 at postoperative day 30). In addition to the gauge of vitrectomy, gas tamponade and SO injection were factors showed notable coefficient of linear regression. For example, the coefficient of gas tamponade showed 1.02 and 1.16 at day 7 and 30. Additionally, that of SO was 2.70 and 2.75 at day 1 and 7.
The 23-gauge TSV group showed significantly higher incidences of hypotony (IOP <6 mm Hg) at postoperative day 1 than the 20-gauge vitrectomy group (10 of 338 (3.0%) vs 0%, P<0.001 by Fisher's exact test) although the incidence of preoperative hypotony was lower in the 23-gauge TSV group (Figure 3a). On the other hand, the incidence of hypertony (IOP>24 mm Hg) was considerably greater in the 20-gauge vitrectomy group at postoperative day 1 (103 of 476 (21.6%) vs 6 of 338 (1.8%), P<0.001 by χ2 test, Figure 3b). The incidences of hypotony and hypertony at postoperative day 7 and that of hypotony at postoperative day 30 were not significantly different between 20- and 23-gauge vitrectomy. The incidence of hypertony at postoperative day 30 was higher in 23-guage vitrectomy than that of 20 gauge vitrectomy, which showed borderline significance (18 of 338 (5.3%) vs 11 of 476 (2.3%), P=0.02, Figure 3b). However, this difference was not significant after the exclusion of steroid responders among the groups (1 of 338 (0.3%) vs 2 of 476 (0.4%), P=0.626).
Discussion
This study demonstrates that two methods of vitrectomy resulted in different patterns of postoperative IOP, with the difference being most marked during the early postoperative period. The IOP and its change, calculated by preoperative IOP subtracted from postoperative IOP, at postoperative day 1 was significantly higher in 20-gauge vitrectomy and the IOP pattern after 20-gauge vitrectomy showed an early postoperative IOP spike, which was absent in 23-gauge TSV. More specifically, the use of 20-gauge vitrectomy was associated with an increase in postoperative 1 day IOP by 7.3 mm Hg. Owing to higher and fluctuating postoperative IOP, our result suggests that 20-gauge vitrectomy may be unfavorable in eyes that are vulnerable to high and fluctuating IOP such as eyes with glaucoma or at risk of retinal ischemia and ischemic optic neuropathy.
A more controlled comparative analysis of 20-gauge and 23-gauge ERM cases also showed the IOP was significantly higher in 20-gauge vitrectomy at postoperative day 1. Subsequent differences in IOP and its change were not significant between the two gauges of vitrectomy. Multiple regression analysis also showed the gauge of vitrectomy to be the significant factor affecting IOP at postoperative day 1.
In this study, postoperative hypotony of 23-gauge TSV was 3.0%, which was comparable to 2.8% in Fine et al's study6 and that of 20-gauge vitrectomy was 0%, which was also similar to previous reports13. On the basis of statistically significant differences in the incidence of hypotony, our study confirmed the higher incidence of early postoperative hypotony in 23-gauge TSV, as previously reported. On the other hand, the incidence of hypertony was higher in 20-gauge vitrectomy (21.6%) compared with 23-gauge TSV (1.8%), demonstrating that 23-gauge TSV is more advantageous in preventing hypertony after vitrectomy.
Among cases showing hypertony at postoperative day 30, 9 out of 11 cases in 20-gauge vitrectomy and 17 out of 18 cases in 23-gauge TSV proved to be steroid responders as IOP dropped to normal range within 2 weeks after topical steroid discontinuation. Excluding the steroid responders, the incidence of hypertony at postoperative day 30 was not significantly different between 20- and 23-gauge vitrectomy and, thus, the significant difference in the incidence of hypotony or hypertony between 20-gauge and 23-gauge vitrectomy was confined to postoperative day 1.
For the different courses of postoperative IOP between 23- and 20-gauge vitrectomy, we suggest two possible mechanisms. First, microleakage from sclerotomy sites may occur in 23-gauge TSV during the early postoperative period. The sutureless sclerotomy wound may function as a pressure-relief valve and prevent postoperative hypertony by permitting microleakage in cases of elevated IOP. Second, the different degree of inflammation after the two vitrectomies may be another causative factor. Postoperative inflammation has been shown to be more severe in the 20-gauge system than in smaller gauge systems,14 and the degree of inflammation was also more severe in 20-gauge vitrectomy than that in 23-gauge TSV at postoperative day 1 in our study (data not shown). As postoperative inflammation was most severe at day 1, the IOP spike observed in 20-gauge vitrectomy at the day may be explained by the pressure-raising effect of postoperative inflammation which alters the function of the trabecular meshwork and ciliary body.15
However, a previous study performed by Singh et al16 reported IOP instability after 23-gauge vitrectomy that demonstrated IOP spikes in early postoperative period. In the study, the percentages of IOP-raising intraoperative procedures such as sub-Tenon triamcinolone (31%) and intravitreal gas injection (30%) were higher than those of our study (0% and 25.4%, respectively). IOP pattern can differ as intraoperative factors which affect postoperative IOP vary in different studies. However, multiple regression was performed in this study to control the effects of other factors on IOP and it revealed that 20-gauge vitrectomy, compared with 23-gauge TSV, was associated with significant postoperative IOP increase at day 1. It indicates that 23-gauge TSV is beneficial to prevent early postoperative IOP spike, compared with 20-gauge vitrectomy. However, it is unknown whether the early postoperative IOP spike in 20-gauge vitrectomy indeed causes optic nerve damage. In the long run, the use of tamponade, either with gas or silicone oil, may have a greater impact on chronic IOP rise and optic nerve damage than gauge of vitrectomy as the tamponade factors were associated with IOP rise at day 7 and 30. However, the effect of gauge on IOP at day 1 was remarkable (7.3 mm Hg according to multiple regression analysis) and, thus, in predisposed eyes such as glaucoma or at risk of retinal ischemia and ischemic optic neuropathy, such a significant effect of gauge of vitrectomy should be considered for clinical decision making, although the effect persists only for a short term.
Some limitations of our study require consideration. First, its retrospective design has its intrinsic drawback regarding bias. Second, because of the relatively short follow-up period, we were unable to compare long-term postoperative IOP changes. In addition, the association between postoperative inflammation and IOP as well as that between postoperative IOP change after vitrectomy and long-term optic nerve damage should be further explored.
Despite these limitations, the present study is one of the largest case series undertaken to date comparing postoperative IOP of 20- and 23-gauge vitrectomy covering most indications of vitrectomy. These results represent not just selective indications of vitrectomy but an actual compilation of all indications for vitrectomy.
In conclusion, 23-gauge TSV produced a more stable pattern of early postoperative IOP and showed a lower incidence of early postoperative hypertony than conventional 20-gauge vitrectomy. In patients whose optic nerve or ocular perfusion are vulnerable to hypertony and IOP fluctuation, 23-gauge TSV may be a superior choice than 20-gauge vitrectomy although long-term consequence of early postoperative IOP spike is unknown.

References
Fujii GY, De Juan Jr E, Humayun MS, Chang TS, Pieramici DJ, Barnes A et al. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology 2002; 109: 1814–1820.
Chen E . 25-Gauge transconjunctival sutureless vitrectomy. Curr Opin Ophthalmol 2007; 18: 188–193.
Williams GA . 25-, 23-, or 20-gauge instrumentation for vitreous surgery? Eye (Lond) 2008; 22: 1263–1266.
Eckardt C . Transconjunctival sutureless 23-gauge vitrectomy. Retina 2005; 25: 208–211.
Tewari A, Shah GK, Fang A . Visual outcomes with 23-gauge transconjunctival sutureless vitr. Retina 2008; 28: 258–262.
Fine HF, Iranmanesh R, Iturralde D, Spaide RF . Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology 2007; 114: 1197–1200.
Tan CS, Wong HK, Yang FP, Lee JJ . Outcome of 23-gauge sutureless transconjunctival vitrectomy for endophthalmitis. Eye 2008; 22: 150–151.
Siqueira RC, Gil AD, Jorge R . Retinal detachment surgery with silicone oil injection in transconjunctival sutureless 23-gauge vitrectomy. Arq Bras Oftalmol 2007; 70: 905–909.
Kim MJ, Park KH, Hwang JM, Yu HG, Yu YS, Chung H . The safety and efficacy of transconjunctival sutureless 23-gauge vitrectomy. Korean J Ophthalmol 2007; 21: 201–207.
Gupta OP, Ho AC, Kaiser PK, Regillo CD, Chen S, Dyer DS et al. Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol 2008; 146: 193–197.
Lott MN, Manning MH, Singh J, Zhang H, Singh H, Marcus DM . 23-gauge vitrectomy in 100 eyes: short-term visual outcomes and complications. Retina 2008; 28: 1193–1200.
Misra A, Ho-Yen G, Burton RL . 23-gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparison. Eye (Lond) 2009; 23: 1187–1191.
Haas A, Seidel G, Steinbrugger I, Maier R, Gasser-Steiner V, Wedrich A et al. Twenty-three-gauge and 20-gauge vitrectomy in epiretinal membrane surgery. Retina 2010; 30: 112–116.
Inoue Y, Kadonosono K, Yamakawa T, Uchio E, Watanabe Y, Yanagi Y et al. Surgically-induced inflammation with 20-, 23-, and 25-gauge vitrectomy systems: an experimental study. Retina 2009; 29: 477–480.
Chang S . LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol 2006; 141: 1033–1043.
Singh CN, Iezzi R, Mahmoud TH . Intraocular pressure instability after 23-gauge vitrectomy. Retina 2010; 30 (4): 629–634.
Acknowledgements
This study was supported by grants from the Seoul National University Bundang Hospital (No. 02-2005-028 and 03-2009-008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ahn, S., Woo, S., Ahn, J. et al. Comparison of postoperative intraocular pressure changes between 23-gauge transconjunctival sutureless vitrectomy and conventional 20-gauge vitrectomy. Eye 26, 796–802 (2012). https://doi.org/10.1038/eye.2012.23
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.23
Keywords
This article is cited by
-
Early influence of endotamponade on corneal biomechanical parameters, central corneal thickness and accuracy of intraocular pressure measurement
Scientific Reports (2023)
-
Clinical outcomes of a beveled tip, ultra-high speed, 25-gauge pars plana vitrectomy system
BMC Ophthalmology (2022)
-
Treatment-Emergent Adverse Events in Gene Therapy Trials for Inherited Retinal Diseases: A Narrative Review
Ophthalmology and Therapy (2020)
-
Outcome of 2 cc pure sulfur hexafluoride gas tamponade for macular hole surgery
BMC Ophthalmology (2016)
-
Intra-orbital gas following sutureless small-gauge (23-gauge) vitrectomy masquerading as orbital cellulitis
Eye (2014)