Abstract
Purpose
To correlate the response of topical dorzolamide (Trusopt; Merck) in patients with X-linked retinoschisis (XLRS) with genotype.
Methods
We carried out a retrospective evaluation of four patients (seven eyes) with XLRS, treated with topical dorzolamide. The change in best-corrected visual acuity (VA) and central macular thickness (CMT; central 1 mm subfield thickness) from optical coherence tomography (OCT) was analysed over the follow-up period, using Student's t-test. Each patient also had genetic analysis for mutations in the retinoschisisgene (RS1).
Results
The mean age at the start of treatment was 14.7±11 years, and mean follow-up duration was 21.7±7.7 months. Mean CMT at the final follow-up was significantly better than at baseline (291±123 vs352±119 μm, P=0.007); however, mean VA was worse (0.38±0.25 vs0.31±0.24 logMAR score, P=0.041). All four patients had a mutation in the RS1gene; there was no apparent association between the type of mutation and the response to topical dorzolamide.
Conclusion
Topical dorzolamide may have some effect in reducing central macular thickness in patients with XLRS, but this does not necessarily correlate with improvement in VA. In our case series, genotypic information did not predict the response to this treatment.
Similar content being viewed by others
Introduction
X-linked retinoschisis (XLRS) is a relatively rare retinal dystrophy, with a prevalence of up to 1 in 20 000.1, 2 It is however the most common cause of macular dystrophy in young males.3, 4, 5, 6 It usually presents in young boys in the first decade with reduced vision. Typical clinical features include macular schisis and peripheral bilateral infero-temporal retinoschsis.7 Vitreous syneresis and veils may also be present.8, 9
XLRS is associated with mutations in the retinoschisin (RS1) gene in Xp22.2, which encodes the protein retinoschisin.10 Retinoschisin is mainly secreted by the photoreceptors and also by the bipolar cells. It has a discoidin domain thought to have a role in cell adhesion.5, 11, 12 Mutation in RS1 results in schisis (splitting) of the neural retina within the superficial retinal layers, the inner limiting membrane, the nerve fibre layer, and the ganglion cell layer, leading to reduced visual acuity (VA) in affected males.13, 14, 15, 16
Three main underlying pathological mechanisms are presumed responsible for retinoschisin protein dysfunction. These include defective assembly of the disulphide-linked subunit, abnormal folding of the discoidin domain, and inability of retinoschisin to insert into the endoplasmic reticulum membrane (part of the protein secretion process).11, 17 XLRS mouse models have helped to explore underlying retinal pathology, with murine gene therapy studies showing promising results.6, 18, 19
As the nerve fibre layer splits at the macula, cyst-like structures develop in a cartwheel-like pattern (‘stellate’ or ‘bicycle-wheel’ maculopathy). This is the cardinal sign of XLRS.7 Unlike typical cystoid macular oedema, no late leakage is present on fluorescein angiography.20 Previously, macular schisis was regarded as untreatable. However, recent reports suggest that carbonic anhydrase inhibitors administered topically or systemically can treat maculopathy, improving vision in approximately two-thirds of patients.3, 21, 22, 23, 24
Only one other study has correlated genotype with response to topical carbonic anhydrase inhibitors in XLRS.23 In this study we present our findings of correlating phenotype (the response to therapy with carbonic anhydrase inhibitors) with underlying genotype (mutations in RS1) in this rare population group.
Materials and methods
Subjects were identified from the medical retina clinic of AJL at the Southampton Eye Unit. All patients had clinical X-linked retinoschisis with macular schisis, associated with mutations in the RS1 gene.
Baseline was defined as the clinic visit in which topical dorzolamide (Trusopt; Merck, Whitehouse Station, NJ, USA) was commenced. The follow-up period was defined as the duration during which topical dorzolamide was administered. Best corrected VA measured by Snellen or logMAR charts was recorded at baseline and at each follow-up visit. For purpose of analysis, where used, Snellen VA was converted to an equivalent logMAR score, where 0.00 was equivalent to 6/6 and 1.00 was equivalent to 6/60. Central macular thickness (CMT) was measured at the majority of visits with Optical Coherence Tomography (Stratus OCT; Carl Zeiss Meditec, Dublin, CA, USA). OCT scans were all taken in the morning between 0900 and 1300 hours. CMT values were obtained from automated macular thickness map analysis, based on the central 1 mm subfield thickness.25
LogMAR VA and CMT at 3 months, 12 months, and the final visit were compared with baseline values using Student's t-test (Microsoft Excel, Redmond, WA, USA). Statistical significance was defined as P<0.05. Clinical significance was defined as a change in logMAR score of ≥0.12, and CMT of ≥19.6% (based on previously reported normal variability between visits in nontreated eyes).21, 26
All patients underwent mutation scanning in the RS1 gene. This was performed by the East Anglian Medical Genetics Service based at Addenbrooke's Hospital, Cambridge, UK. Fluorescent sequencing analysis of exons 1–6 of the RS1 gene was performed and analysed by Mutation Surveyor (Softgenetics, State College, PA, USA). All mutation nomenclature was described according to GenBank accession number AF014459 (where +1 is the A of the ATG translation initiation codon). Treatment response based on genotype was then investigated.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
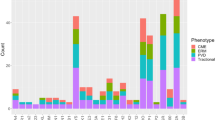
A total of seven eyes (four patients) were included. Each eye was treated with topical dorzolamide 2% three times a day. The findings are summarised in Table 1. VA and OCT CMT changes over the follow-up period for each eye are shown in Figure 1. All patients were treated bilaterally, except for patient 3 (right eye not treated because of irreversible macular damage from previous scarring). The mean age at baseline was 14.7±11.1 years, with a large range (7.9–31.2 years). Mean duration of follow-up was 21.7±7.7 months.
For all eyes, mean VA at the 3- and 12-month point was no different to baseline, although VA at the final visit was actually significantly worse (0.38±0.25 vs 0.31±0.24 logMAR score, P=0.041). No eyes demonstrated a significant clinical improvement in VA at the final visit, compared with baseline. One eye (patient 1, left eye) had clinically significantly worse VA at the end of follow-up.
Mean CMT at the 3-month visit was no different to baseline, but improved significantly by the 12-month point. CMT at the final visit was also significantly better compared with baseline (291±123 vs 352±119 μm, P=0.007). A clinically significant reduction in CMT was demonstrated in four eyes at the final visit compared with baseline (patient 1, left eye, patient 2, both eyes, and patient 3, left eye).
A more pronounced improvement in vision was noticed in two eyes at the first follow-up visit at month 1 (patient 4, both eyes). This was accompanied by a small corresponding drop in CMT in the left eye (21 μm); however, the right eye CMT worsened slightly (by 14 μm). Indeed, at month 3 this patient was advised to stop treatment in the right eye because of worsening of VA with associated increase in CMT. In the next follow-up visits following cessation of topical dorzolamide, VA and CMT appeared to recover. Otherwise, there were no adverse events.
When considering mean VA and CMT at all follow-up visits compared with baseline, VA was no different (0.33±0.23 vs 0.31±0.24 logMAR score, P=0.39); mean CMT was better, but not quite statistically significant (328±132 vs 352±119 μm, P=0.072). Both VA and CMT measurements demonstrated high levels of intervisit variability (Figure 2). Only one eye showed consistent reduction in CMT at all follow-up visits (patient 3, left eye). This happened to be the oldest patient. Figure 3 shows the OCT scan at baseline and final visit for all eyes.
Genotype data are summarised in Table 2. One patient (patient 2) harboured two mutations in the RS1 gene. However, no obvious relationship was observed between genotype and response to topical dorzolamide 2% eye drops.
Discussion
In our group of patients with XLRS treated with topical dorzolamide, there was statistically significant improvement in OCT CMT over the follow-up period, but this was not accompanied with a corresponding improvement in vision. Indeed, VA at the final visit was statistically significantly worse compared with baseline. Using our definitions of clinical significant change, four out of seven eyes demonstrated a clinically significant reduction in CMT. However, no eyes demonstrated clinically significant improvement in VA.
Several studies in the literature report the use of topical dorzolamide in XLRS. Apushkin and Fishman21 treated eight patients aged 21–47 years old with XLRS for up to 6 months. They found that seven had a noticeable reduction in CMT; five also had improvement in VA by ≥7 letters in at least one eye. Genead et al24 treated 15 patients (29 eyes) with XLRS aged 18–53 over a longer follow-up period (mean 16.5 months). They found that 17 eyes demonstrated a reduction of CMT, and 16 eyes had an improvement of VA of at least 7 letters. They also noticed that five eyes experienced a ‘rebound’ phenomenon, where CMT levels returned during the treatment period to at least baseline levels. They suggested patients receiving topical dorzolamide to be observed closely for lack of response or potential rebound. It is possible that patient 2 in our study experienced a rebound phenomenon in CMT at the 2-year point in both eyes, which resolved at the next visit. Alternately, this may have been because of inconsistencies in OCT measurement.
Walia et al23 treated 7 patients with XLRS aged 19–38 years with topical dorzolamide, for 2–26 months, and correlated this with genotype. A clinically significant improvement in CMT was observed in three of four patients with absence of protein secretion, in two with a lack of protein secretion, and in one patient with nonfunctional protein secretion. They concluded that response ‘to dorzolamide in patients with XLRS may be observed independent of the mechanism responsible for retinoschisin protein dysfunction’. However, the observed mutations in these were different to the ones observed in our patient group, with changes mainly occurring in exons 4 and 5 of the RS1 gene. Our report adds to the findings of Walia et al23 in this rare population group. The age, however, of our study population was noticeably younger than those previously reported.
A lack of relationship between improvement in VA and macula thickness in our study suggests that an anatomical improvement in macular thickness may not necessarily translate into patient subjective benefit. However, there may still be longer-term benefit in restoring anatomical integrity, to preserve retinal architecture, reduce permanent damage, and limit progressive atrophy.27 This, together with the lack of alternative options, was the rationale for continuing treatment with topical dorzolamide throughout the follow-up period, despite no obvious clinical benefit in VA.
Of interest, the patient who had consistently clinically significant improvement in macular thickness at each visit was the only adult of our case series. This suggests that compliance with daily drops three times a day in children may be an issue. In particular, the midday dose may be difficult to administer in the school environment, especially if teachers are not comfortable with eye drop installation. Compliance may be further affected by the local side effects of topical dorzolamide, which include localised burning, stinging, and redness.28 It may be preferable to use topical brinzolamide, an alternative topical CAOI (Azopt, Alcon, Hünenberg, Switzerland), which is administered twice a day, and may have a better side-effect profile.29, 30 Additionally, compliance may have also been an issue with VA measurements and OCT scanning, and this may have caused the large intervisit variability seen.
There are several possible mechanisms of the action that may explain any beneficial effect of topical dorzolamide in patients with XLRS. CAOIs may decrease the levels of subretinal fluid, either directly by active ion transport or indirectly by an increase in acidification, with secondary changes in ion and therefore fluid transport.31, 32, 33 CAOIs may also act by enhancing adhesiveness of the retina to the RPE, increasing production of otherwise deficient retinoschisin, or by stimulation of RPE removal of soluble retinoschisin within the cystic spaces.21, 32, 34, 35
In this case series, we did not notice any relationship between genotype and observed response to topical dorzolamide. However, it is difficult to draw any substantial conclusions from a small case series. Larger numbers with longer follow-up would be useful to investigate the influence of specific mutations further, especially as the exact effect of mutations on response to topical CAOIs in XLRS is still unclear. Longer-term follow-up would provide more detail on the long-term benefits/side effects of topical dorzolamide in XLRS. However, XLRS is a rare disease, and investigating a large case series may be practically difficult to carry out.
In conclusion, topical dorzolamide appears to have some effect in reducing central macular thickness in young patients with XLRS, but does not correlate with an improvement in VA. Patients on treatment should be observed for potential rebound phenomena. Compliance with drops may be an issue, especially with the typically young age of the patient population. There was no relationship between genotype and response to treatment in this study. However, this is only a small case series and further studies would be useful to examine this relationship.

Accession codes
References
de la Chapelle A, Alitalo T, Forsius H . X-linked juvenile retinoschisis. In: Wright A, Jay B (eds). Molecular Genetics of Inherited Eye Disorders, 1st edn., Harwood Academic Publishers: Switzerland, 1994, pp 339–357.
Sikkink SK, Biswas S, Parry NR, Stanga PE, Trump D . X-linked retinoschisis: an update. J Med Genet 2007; 44: 225–232.
Iannaccone A, Fung KH, Eyestone ME, Stone EM . Treatment of adult-onset acute macular retinoschisis in enhanced s-cone syndrome with oral acetazolamide. Am J Ophthalmol 2009; 147: 307–312.
Forsius H, Krause U, Helve J, Vuopala V, Mustonen E, Vainio-Mattila B et al. Visual acuity in 183 cases of X-chromosomal retinoschisis. Can J Ophthalmol 1973; 8: 385–393.
Grayson C, Reid SN, Ellis JA, Rutherford A, Sowden JC, Yates JR et al. Retinoschisin, the X-linked retinoschisis protein, is a secreted photoreceptor protein, and is expressed and released by Weri-Rb1 cells. Hum Mol Genet 2000; 9: 1873–1879.
Zeng Y, Takada Y, Kjellstrom S, Hiriyanna K, Tanikawa A, Wawrousek E et al. RS-1 gene delivery to an adult Rs1h knockout mouse model restores ERG b-wave with reversal of the electronegative waveform of X-linked retinoschisis. Invest Ophthalmol Vis Sci 2004; 45: 3279–3285.
Ewing CC, Ives EJ . Juvenile hereditary retinoschisis. Trans Ophthalmol Soc UK 1970; 89: 29–39.
Ando A, Takahashi K, Sho K, Matsushima M, Okamura A, Uyama M . Histopathological findings of X-linked retinoschisis with neovascular glaucoma. Graefes Arch Clin Exp Ophthalmol 2000; 238: 1–7.
Sarin LK, Green WR, Dailey EG . Juvenile retinoschisis. Congenital vascular veils and hereditary retinoschisis. Am J Ophthalmol 1964; 57: 793–796.
Sauer CG, Gehrig A, Warneke-Wittstock R, Marquardt A, Ewing CC, Gibson A et al. Positional cloning of the gene associated with X-linked juvenile retinoschisis. Nat Genet 1997; 17: 164–170.
Wu WW, Molday RS . Defective discoidin domain structure, subunit assembly, and endoplasmic reticulum processing of retinoschisin are primary mechanisms responsible for X-linked retinoschisis. J Biol Chem 2003; 278: 28139–28146.
Wu WW, Wong JP, Kast J, Molday RS . RS1, a discoidin domain-containing retinal cell adhesion protein associated with X-linked retinoschisis, exists as a novel disulfide-linked octamer. J Biol Chem 2005; 280: 10721–10730.
Manschot WA . Pathology of hereditary juvenile retinoschisis. Arch Ophthalmol 1972; 88: 131–138.
Yanoff M, Kertesz RE, Zimmerman LE . Histopathology of juvenile retinoschisis. Arch Ophthalmol 1968; 79: 49–53.
Brucker AJ, Spaide RF, Gross N, Klancnik J, Noble K . Optical coherence tomography of X-linked retinoschisis. Retina 2004; 24: 151–152.
Ozdemir H, Karacorlu S, Karacorlu M . Optical coherence tomography findings in familial foveal retinoschisis. Am J Ophthalmol 2004; 137: 179–181.
Wang T, Waters CT, Rothman AM, Jakins TJ, Romisch K, Trump D . Intracellular retention of mutant retinoschisin is the pathological mechanism underlying X-linked retinoschisis. Hum Mol Genet 2002; 11: 3097–3105.
Jablonski MM, Dalke C, Wang X, Lu L, Manly KF, Pretsch W et al. An ENU-induced mutation in Rs1h causes disruption of retinal structure and function. Mol Vis 2005; 11: 569–581.
Weber BH, Schrewe H, Molday LL, Gehrig A, White KL, Seeliger MW et al. Inactivation of the murine X-linked juvenile retinoschisis gene, Rs1h, suggests a role of retinoschisin in retinal cell layer organization and synaptic structure. Proc Natl Acad Sci USA 2002; 99: 6222–6227.
Deutman A, Hoyng C, van Lith-Verhoeven J . Macular dystrophies. In: Ryan S, Hinton D, Schachat A (eds). Retina, 4th edn. Elsevier/Mosby: Philadelphia, PA, 2006, pp 1165.
Apushkin MA, Fishman GA . Use of dorzolamide for patients with X-linked retinoschisis. Retina 2006; 26: 741–745.
Ghajarnia M, Gorin MB . Acetazolamide in the treatment of X-linked retinoschisis maculopathy. Arch Ophthalmol 2007; 125: 571–573.
Walia S, Fishman GA, Molday RS, Dyka FM, Kumar NM, Ehlinger MA et al. Relation of response to treatment with dorzolamide in X-linked retinoschisis to the mechanism of functional loss in retinoschisin. Am J Ophthalmol 2009; 147: 111–115.
Genead MA, Fishman GA, Walia S . Efficacy of sustained topical dorzolamide therapy for cystic macular lesions in patients with X-linked retinoschisis. Arch Ophthalmol 2010; 128: 190–197.
Leung CK, Cheung CY, Weinreb RN, Lee G, Lin D, Pang CP et al. Comparison of macular thickness measurements between time domain and spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci 2008; 49: 4893–4897.
Grover S, Fishman GA, Gilbert LD, Anderson RJ . Reproducibility of visual acuity measurements in patients with retinitis pigmentosa. Retina 1997; 17: 33–37.
George ND, Yates JR, Bradshaw K, Moore AT . Infantile presentation of X linked retinoschisis. Br J Ophthalmol 1995; 79: 653–657.
Joint Formulary Committee. British National Formulary, 59 ed. British Medical Association and Royal Pharmaceutical Society of Great Britain: London, 2010. www.bnf.org/bnf. BNF 56.
Silver LH . Ocular comfort of brinzolamide 1.0% ophthalmic suspension compared with dorzolamide 2.0% ophthalmic solution: results from two multicenter comfort studies. Brinzolamide Comfort Study Group. Surv Ophthalmol 2000; 44 (Suppl 2): S141–S145.
Stewart WC, Day DG, Stewart JA, Holmes KT, Jenkins JN . Short-term ocular tolerability of dorzolamide 2% and brinzolamide 1% vs placebo in primary open-angle glaucoma and ocular hypertension subjects. Eye 2004; 18: 905–910.
Marmor MF, Abdul-Rahim AS, Cohen DS . The effect of metabolic inhibitors on retinal adhesion and subretinal fluid resorption. Invest Ophthalmol Vis Sci 1980; 19: 893–903.
Marmor MF, Maack T . Enhancement of retinal adhesion and subretinal fluid resorption by acetazolamide. Invest Ophthalmol Vis Sci 1982; 23: 121–124.
Wolfensberger TJ, Chiang RK, Takeuchi A, Marmor MF . Inhibition of membrane-bound carbonic anhydrase enhances subretinal fluid absorption and retinal adhesiveness. Graefes Arch Clin Exp Ophthalmol 2000; 238: 76–80.
Kita M, Marmor MF . Effects on retinal adhesive force in vivo of metabolically active agents in the subretinal space. Invest Ophthalmol Vis Sci 1992; 33: 1883–1887.
Wang T, Zhou A, Waters CT, O’Connor E, Read RJ, Trump D . Molecular pathology of X linked retinoschisis: mutations interfere with retinoschisin secretion and oligomerisation. Br J Ophthalmol 2006; 90: 81–86.
Acknowledgements
We acknowledge the East Anglian Molecular Genetics Laboratory at Addenbrooke's Hospital, Cambridge, UK, for performing molecular genetic testing and for providing genotype data for the patients. We also thank Frimley Park Hospital NHS Trust, the TFC Frost Charitable Trust, and the Gift of Sight Appeal for providing funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was previously presented as an abstract at ARVO 2009.
Rights and permissions
About this article
Cite this article
Khandhadia, S., Trump, D., Menon, G. et al. X-linked retinoschisis maculopathy treated with topical dorzolamide, and relationship to genotype. Eye 25, 922–928 (2011). https://doi.org/10.1038/eye.2011.91
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.91
Keywords
This article is cited by
-
Cystoid macular oedema without leakage in fluorescein angiography: a literature review
Eye (2023)
-
Outcome measures in juvenile X-linked retinoschisis: A systematic review
Eye (2020)
-
Genetic analysis and clinical features of X-linked retinoschisis in Chinese patients
Scientific Reports (2017)
-
Topical dorzolamide treatment of macular cysts in the enhanced S-cone syndrome patient
Documenta Ophthalmologica (2013)