Abstract
Objective
The objective of this study was to determine the prevalence of ocular complications and blindness among leprosy patients presenting in the United Kingdom.
Methods
Observational prospective study.
Results
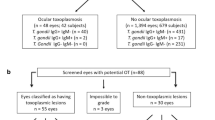
A total of 126 consecutive leprosy patients attending their ophthalmic visit were examined, out of which 18 patients were blind in one eye (14.3%) and five patients were blind in both the eyes (4.0%). Visual acuity of ⩾6/18 was present in 96 patients (76.2%). A total of 65 patients (51.6%) had an ocular complication and 28 patients (22.2%) had a sight-threatening leprosy complication (lagophthalmos, severe corneal, or iris disease). The most common ocular complications were impaired lid closure (24 patients, 19%), impaired corneal sensation (20 patients, 15.9%), cataract (20 patients, 15.9%), mild corneal opacity (17 patients, 13.5%), and iris atrophy (17 patients, 13.5%). Impaired corneal sensation was associated with vision <6/18 (P<0.001, OR 13.5, 95% CI 5.14–35.44) and vision <3/60 (P=0.01 OR 6.42, 95% CI 2.15–19.15). Impaired lid closure was significantly associated with increasing age (P=0.029, OR 1.039, 95% CI 1.0–1.08) and vision <3/60 (P=0.03, OR 6.06, 95% CI 1.81–20.24).
Conclusion
There is a significant rate of ocular complications and blindness seen in leprosy patients in the United Kingdom, and over one in five had a potentially sight-threatening ocular complication. Health professionals and all leprosy patients, including those cured of the disease, need to be aware that new eye symptoms and signs require prompt ophthalmology review to prevent avoidable blindness, due to the life-long risk of sight-threatening ocular complications.
Similar content being viewed by others
Introduction
Leprosy has been well recognised and feared for many centuries. The first known written mention of the disease is dated to 600 BC, and it has always been associated with horrifying images of disfigurement and exclusion from society.1 The causative organism, Mycobacterium leprae, mainly affects the skin, peripheral nerves, upper respiratory tract mucosa, and also the eyes. If untreated, or if treatment is delayed, the patient is left with permanent and often progressive physical deformities due to nerve damage. Treatment first appeared as late as the 1940s with the arrival of dapsone and its derivatives, but drug resistance meant that monotherapy had limited effectiveness. However, there have been important changes in the management of the disease and consequently in its epidemiology in recent times. In 1981, a World Health Organisation (WHO) Study Group recommended multidrug therapy (dapsone, rifampicin, and clofazimine), the first really effective drug combination that kills the pathogen and is curative. The widespread use of multidrug treatment (MDT) has had a significant impact on the disease burden and more than 14 million leprosy patients have since been cured.2 WHO is committed to elimination of the disease and this has been successful in many previously endemic countries. However, pockets of high endemicity remain in areas of Brazil, India, Nepal, and sub-Saharan Africa. Although treated patients are considered cured, many are still left with physical disabilities, and the stigma surrounding the disease remains in endemic countries, leading to unnecessary delays in presentation.
Ocular morbidity and blindness can be a devastating complication for leprosy patients who may rely on their eyes to protect their anaesthetic limbs. The ocular manifestations are varied, and Armauer Hansen (credited with discovering M. leprae) is quoted as saying ‘there is no disease that so frequently gives rises to disorders of the eye as leprosy.’3 The reported prevalence of ocular complications in leprosy, before the introduction of MDT, varied from 6.6 to 74.2%.4, 5, 6, 7, 8, 9, 10 Many of these studies had a lack of clear definitions of ocular complications, used non-ophthalmologically trained individuals as examiners and lacked adequate instrumentation to detect signs.11 Since the widespread use of MDT, the prevalence of ocular complications in patients still fluctuates and has been reported as high as 66%.12 Importantly, several studies have also shown that patients continue to develop new ocular complications after successful completion of treatment.13, 14, 15
Although the United Kingdom has not been an endemic country for centuries, historical references show reports of deaths from ‘active leprosy’ recorded in the UK newspapers in the early 1900s.16 This prompted an article in the BMJ in 1913 on ‘Leprosy in London’, which concluded that despite the headlines, only one patient had contracted leprosy in the United Kingdom and there was only a small number seen in London dermatology clinics.17 Since then, significant global changes in migration and travel have meant that many tropical diseases that are non-endemic to the United Kingdom are now seen here. There have been few studies on ocular complications in leprosy based in non-endemic countries, and none from the United Kingdom.7, 18, 19, 20 This study is the first review of ocular complications of leprosy seen in patients presenting in the United Kingdom.
Materials and methods
This was a prospective study of all patients attending the ophthalmology outpatient clinic at the Hospital for Tropical Diseases (HTD) in London between 1985 and 2006. The HTD is a tertiary referral NHS hospital specialising in tropical diseases and has dedicated leprosy clinics. Its patient population includes long- and short-term travellers, immigrants, and refugees in Britain.
All leprosy patients attending the HTD were referred to the eye clinic, irrespective of whether they had ocular complaints, and were examined by the same ophthalmic surgeon (T.ff). All clinical details were recorded at the ophthalmic consultation by a validated data collection proforma for analysis.21 Patients included those newly diagnosed (at the HTD), those diagnosed at other institutions, and patients under ongoing care at the HTD.
SPSS version 15 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis and the findings were analysed by patient, rather than by eye.22, 23 Ocular complications were divided into leprosy-related ocular complications (LROC) and general ocular complications (GOC), as used in other studies.12 Leprosy-related ocular complications included lagophthalmos, ectropion, entropion, trichiasis, episcleritis, scleritis, diminished corneal sensation, corneal opacity, acute/chronic iritis, iris atrophy, and synechiae. General ocular complications included pterygium, cataract, aphakia, and pseudophakia. Sight-threatening ocular complications were defined as lagophthalmos or severe corneal or iris disease. The definition of decreased vision was a corrected Snellen visual acuity of <6/18 and the definition of blindness used was <3/60, as classified by the WHO. The relationship of risk factors with incidence of complications was tested with univariable and, where appropriate, multivariable logistic regression.
Results
Patient characteristics
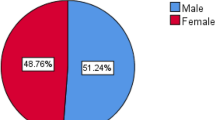
A total of 126 patients were studied, out of which 98 patients were male (77.8%). The age of the patients ranged from 5 to 85 years, with a mean of 50 years. The ethnic origin of patients varied widely, the most common being from the Indian sub-continent (40 patients, 31.7%), followed by Africa (16 patients, 12.7%), and SE Asia (11 patients, 8.7%). Other ethnic groups included Arab, Chinese, European, Latin American, and Polynesian. No patients who were born in the United Kingdom were seen. Occupational data was available for 54 patients (42.9%) and from this subgroup, 20 patients (37%) were professional, 8 patients (14.8%) were factory workers, 7 patients (13%) looked after the home, and 6 patients (11%) performed clerical jobs or were students. Other occupations included labourer, cook, seaman, and soldier.
A total of 76 patients (60.3%) had lepromatous disease, 15 patients (11.9%) had tuberculoid, 16 patients (12.7%) had borderline, and in 19 patients (15.1%) the disease classification had not yet been verified (as this was the initial presentation at HTD). The duration of disease ranged from less than 1 year to 54 years. The mean duration was 15 years. This was further subdivided into duration of <5 years for 59 patients (46.8%), 5–20 years for 14 patients (11.1%), and >20 years for 42 patients (33.3%).
Range and stage of patient treatment was wide, with 17 patients (13.5%) having completed MDT and 59 patients (46.8%) on MDT, at the time of examination. Detailed results are shown in Table 1.
Ocular complications
On examination, a visual acuity of 6/18, or better, in both eyes was observed in 96 patients (76.2%). Vision <3/60 in one eye was present in 18 patients (14.3%) and 3 patients were blind (<3/60) in both eyes (2.4%). A total of 28 patients (22.2%) had a sight-threatening leprosy complication (lagophthalmos or severe corneal or iris disease). Causes of visual acuity <3/60 (per eye) are shown in Table 2. Corneal opacity and cataract, or a combination of the two, were the most common causes.
Ocular complications were counted as present whether they were in one or both eyes and were observed in 65 patients (51.6%). The most common ocular complications were the following: diminished lid closure (24 patients, 19.0%), diminished corneal sensation (20 patients, 15.9%), cataract (20 patients, 15.9%), mild corneal opacity (17 patients, 13.5%), and iris atrophy (17 patients, 13.5%). The prevalence of all individual ocular complications is summarised in Table 3.
Primary ocular complications were tested with multivariable analysis against the potential confounders and risk factors of age, duration of disease, classification of disease, and decreased vision. Those found to have significant associations were diminished lid closure, diminished corneal sensation, and cataract. Impaired lid closure was significantly associated with increasing age (P=0.029, OR 1.039, 95% CI 1.0–1.08) and vision <3/60 (P=0.03, OR 6.06, 95% CI 1.81–20.24) but not with duration of disease or disease type. Impaired corneal sensation was associated with vision <6/18 (P<0.001, OR 13.5, 95% CI 5.14–35.44), vision <3/60 (P=0.01 OR 6.42 95% CI 2.15–19.15), and increasing age (P=0.01, OR 1.03, 95% CI 1.01–1.06) but not with duration and disease type.
A total of 59 patients (46.8%) had a LROC and 37 patients (29.4%) had a GOC. LROC was significantly associated with increasing age, duration of disease, decreased vision, and vision <3/60 but not with disease classification (Table 4). GOC was significantly associated with increasing age, duration of disease, decreased vision, and vision <3/60 but not with classification of leprosy. In a multiple regression model, increasing age remained significant (P=0.009, OR 1.07, 95% CI 1.02–1.12). When all documented complications were analysed together as one variable, then increasing age (P<0.0001, OR 1.045, 95% CI 1.02–1.07) and duration of disease (P=0.008, OR 1.035, 95% CI 1.01–1.06) were significantly associated with any complication occurring.
Discussion
This is the first review of ocular findings seen in leprosy patients presenting in the United Kingdom, and shows a significant rate of ocular complications and blindness. Half of all leprosy patients examined had an ocular complication and, although many of these were mild, in more than one in five patients, they were potentially sight threatening. The prevalence of blindness was 2.4% (both eyes), and the main causes were corneal opacity, cataract, or a combination of both. The most recent study based in a non-endemic country was carried out in 1994 and was based in the United States. It was also conducted in an outpatient setting and it found that 74% of the patients had some type of ocular complication, with 48% having a potentially sight-threatening complication.18 Another study based in the Netherlands in 1983 found that 20% of the patients had ocular complications.20 More recent studies based in India and Nepal found rates between 57 and 66% of patients having any type of ocular complication.12, 24, 25 Another study from India also showed that 24.3% of the patients still had sight-threatening ocular complications after completion of MDT.15
The higher prevalence of ocular complications in lepromatous disease and increased duration of disease, as seen in our study, has also been well documented previously.13, 25, 26 Daniel et al14 estimated that per year, 5.6% of patients with multibacillary leprosy, who had completed MDT, could develop new ocular complications of the disease, which in 3.9% of patients was potentially sight threatening. In the same study population, they found that ∼20% of patients could be expected to develop ocular complications of leprosy during the 2-year course of MDT, 11% of which are potentially sight threatening.27 In terms of blindness rates, a multicentre study found a rate of 3.2% and a recent study from India reported a prevalence of 2.9%.25, 28 Studies in the United States and in the Netherlands have found a relatively low prevalence of blindness in their leprosy patients.20 The relatively higher rate of sight-threatening ocular complications and blindness seen in our study may be because of the mixed patient population, some of whom had been suffering from leprosy for many years (duration of the disease range <0–54 years, mean 15 years). Lockwood et al29 have previously shown that leprosy patients from the HTD present late because of delay in diagnosis in the United Kingdom and have a high level of neurological impairment. Any delay in diagnosis could also contribute to more severe ocular complications and blindness.
This review of ocular complications of leprosy patients in the United Kingdom highlights the importance of ongoing care for all leprosy patients, including those considered cured. Leprosy is a disease with chronic and disabling complications, and ocular involvement can be permanent and may progress long after treatment has been completed. Further knowledge on specific risk factors (eg, bacterial index, smear positivity, type 1 and type 2 leprosy reactions, grade of deformity) for ocular disease and blindness in leprosy patients would allow the identification of particularly vulnerable groups of leprosy patients during treatment for closer follow-up in ophthalmology clinics, rather than in general or leprosy clinics.
Significant global changes in population migration and travel have meant that many tropical and poverty-related diseases such as leprosy are seen in increasing numbers in non-endemic countries, including the United Kingdom. For the first time in history, effective treatment and a global strategy for the elimination of leprosy have led to a remarkable change in the fate of patients. The rate of ocular involvement and of potentially sight-threatening ocular complications in this study was significant. This highlights that leprosy is a chronic disease that leads to disability and possible visual impairment and blindness. Patients have a life-long risk of sight-threatening ocular complications and self-referral because of symptoms can often be delayed because of corneal insensitivity masking some of the symptoms. There is a need for good baseline ophthalmological examination for all leprosy patients and patient awareness to promptly seek ophthalmological review for any new eye symptoms or signs, wherever their country of residence. Regular follow-up for leprosy patients deemed to be higher risk is also appropriate.

References
Organisation WH. Factsheet number 101. http://www.who.int/mediacentre/factsheets/fs101/en/, 2005.
WHO. Report of the global forum on elimination of leprosy as a public health problem. Access at http://whqlibdoc.who.int/hq/2006/WHO_CDS_NTD_2006.4_eng.pdf.
Bull OB, Hansen GA . The Leprous Diseases of the Eye. Albert Cammermeyer: Christiania, 1873.
Prasad VN, Narain M, Mukhija RD, Bist HK, Khan MM . A study of ocular complications in leprosy. Indian J Lepr 1984; 56 (2): 241–250.
Reddy SC, Raju BD, Achary NR . Survey of eye complications in leprosy in Prakasam district (Andhra Pradesh). Lepr India 1981; 53 (2): 231–237.
Malla OK, Brandt F, Anten JG . Ocular findings in leprosy patients in an institution in Nepal (Khokana). Br J Ophthalmol 1981; 65 (4): 226–230.
ffytche TJ, Brandt F, Cerchez J, Stoicescu S, Stingl P, Filitis M . Ocular complications observed in leprosy patients in Romania. BMJ (Clinical Research Ed) 1992; 305 (6847): 240–242.
ffytche TJ . The American Peace Corps Survey of the ocular complications of leprosy in South Korea: an evaluation and appraisal. Lepr Rev 1984; 55 (3): 239–246.
Dethlefs R . Prevalence of ocular manifestations of leprosy in Port Moresby, Papua New Guinea. Br J Ophthalmol 1981; 65 (4): 223–225.
Ticho U, Sira IB . Ocular leprosy in Malawi. Clinical and therapeutic survey of 8,325 leprosy patients. Br J Ophthalmol 1970; 54 (2): 107–112.
Courtright PD . Defining the magnitude of ocular complications from leprosy: problems of methodology. Int J Lepr Other Mycobact Dis 1988; 56 (4): 566–573.
Daniel E, Koshy S, Rao GS, Rao PS . Ocular complications in newly diagnosed borderline lepromatous and lepromatous leprosy patients: baseline profile of the Indian cohort. Br J Ophthalmol 2002; 86 (12): 1336–1340.
Lewallen S, Tungpakorn NC, Kim SH, Courtright P . Progression of eye disease in ‘cured’ leprosy patients: implications for understanding the pathophysiology of ocular disease and for addressing eyecare needs. Br J Ophthalmol 2000; 84 (8): 817–821.
Daniel E, ffytche TJ, Kempen JH, Rao PS, Diener-West M, Courtright P . Incidence of ocular complications in patients with multibacillary leprosy after completion of a 2 year course of multidrug therapy. Br J Ophthalmol 2006; 90 (8): 949–954.
ffytche TJ . Residual sight-threatening lesions in leprosy patients completing multidrug therapy and sulphone monotherapy. Lepr Rev 1991; 62 (1): 35–43.
Northern Advocate. Leprosy in London, Newspaper article 1906.
Editor. Leprosy in London. BMJ 1913; 2 (2761): 1449.
Dana MHM, Viana MAG, Hill CH, Sugar J . Ocular manifestations of leprosy in a noninstitutionalised community in the United States. Arch Ophthalmol 1994; 112: 626–629.
Spaide R, Nattis R, Lipka A, D’Amico R . Ocular findings in leprosy in the United States. Am J Ophthalmol 1985; 100 (3): 411–416.
Hogeweg M, Leiker DL . A survey on eye involvement among leprosy patients in The Netherlands. Doc Ophthalmol 1983; 56 (1–2): 69–76.
ffytche TJ . A computer form to aid in the collection of data on the ocular complications of leprosy. Lepr Rev 1983; 54 (4): 271–281.
Morris R . Bilateral procedures in randomised controlled trials. J Bone Joint Surg Br 1993; 75 (5): 675–676.
Murdoch I . People and eyes: statistics in ophthalmology. Community Eye Health 1998; 11 (27): 43.
Courtright P, Daniel E, Rao PS, Ravanes J, Mengistu F, Belachew M et al. Eye disease in multibacillary leprosy patients at the time of their leprosy diagnosis: findings from the Longitudinal Study of Ocular Leprosy (LOSOL) in India, the Philippines and Ethiopia. Lepr Rev 2002; 73 (3): 225–238.
Thompson KJ, Allardice GM, Babu GR, Roberts H, Kerketta W, Kerketta A . Patterns of ocular morbidity and blindness in leprosy—a three centre study in Eastern India. Lepr Rev 2006; 77 (2): 130–140.
Nepal BP, Shrestha UD . Ocular findings in leprosy patients in Nepal in the era of multidrug therapy. Am J Ophthalmol 2004; 137 (5): 888–892.
Daniel E, ffytche TJ, Rao PS, Kempen JH, Diener-West M, Courtright P . Incidence of ocular morbidity among multibacillary leprosy patients during a 2 year course of multidrug therapy. Br J Ophthalmol 2006; 90 (5): 568–573.
ffytche TJ . The prevalence of disabling ocular complications of leprosy: a global study. Indian J Lepr 1998; 70 (1): 49–59.
Lockwood D, Reid A . The diagnosis of leprosy is delayed in the United Kingdom. QJM 2001; 94 (4): 207–212.
Acknowledgements
Professor Diana Lockwood reviewed and commented on the paper. Munnazah Chou assisted with initial data entry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented as Oral presentation at the Royal College of Ophthalmologists meeting
Rights and permissions
About this article
Cite this article
Malik, A., Morris, R. & ffytche, T. The prevalence of ocular complications in leprosy patients seen in the United Kingdom over a period of 21 years. Eye 25, 740–745 (2011). https://doi.org/10.1038/eye.2011.43
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.43
Keywords
This article is cited by
-
Bilateral corneal perforation caused by neurotrophic keratopathy associated with leprosy: a case report
BMC Ophthalmology (2022)
-
Visual processing of color and shape in people with leprosy
Psicologia: Reflexão e Crítica (2020)
-
Anterior segment optical coherence tomography findings of iris granulomas in Hansen's disease: a case report
Journal of Ophthalmic Inflammation and Infection (2013)