Abstract
Purpose
To assess ranibizumab (Lucentis) penetration into the retina after topical administration in a rabbit model.
Methods
Ranibizumab was topically applied to the right eye of rabbits according to three regimens: every 2 h (q2hr), four times daily (qid), and twice daily (bid). Intraocular penetration of ranibizumab was assessed at 3, 7, 14, 21, and 28 days following initiation of drops. At each time point, the anterior chambers, vitreous cavities, and blood of one of the rabbits from each subgroup were sampled for ranibizumab detection using enzyme-linked immunosorbent assay (ELISA), and both eyes were then enucleated for ranibizumab detection in the retina by confocal immunohistochemistry (CI). Another group of rabbits received intravitreal ranibizumab and was similarly sampled for comparison.
Results
CI showed ranibizumab staining in the right retina after 7 and 14 days of q2hr topical administration in two out of four experiments. No ranibizumab was detected in the left retina at any of the sampling time points. ELISA was positive in the vitreous of the right eye at 14 and 21 days in the q2hr treated rabbits in one out of four experiments. No ranibizumab was detected in the qid and bid subgroups. CI and ELISA of the aqueous and vitreous were consistently positive in the intravitreal group. Mild ranibizumab levels were detected in the blood in both the topical and intravitreal groups.
Conclusions
Topically applied ranibizumab can be detected in the retina following high-frequency administration in a rabbit model. A trans-scleral route of penetration is suggested.
Similar content being viewed by others
Introduction
The outlook for retaining vision in neovascular age-related macular degeneration (NVAMD) has been greatly improved by the development of the anti-vascular endothelial growth factor (VEGF) therapies, such as ranibizumab (Lucentis) and bevacizumab (Avastin)1 (Genentech, Inc., South San Francisco, CA, USA). Ranibizumab is an engineered humanized monoclonal antibody fragment (48 kDa) that binds and interferes with VEGF function. Avastin is a whole antibody molecule (149 kDa) against VEGF. Both molecules have been shown to bind VEGF and inhibit new vessel growth, and therefore are effective treatments for neovascularization in NVAMD2 and also clinically significant macular edema seen in diabetic retinopathy.3 However, these anti-VEGF therapies are currently administered by intravitreal injection, often requiring monthly injections for extended periods of time resulting in a significant cumulative risk of endophthalmitis.4, 5, 6, 7 Therefore, alternative methods of administering these medications have been a recent focus of research.8, 9, 10 Administration of a topical medication in the form of eye drops would substantially decrease the ocular risks and discomfort associated with the current intravitreal route, but topical penetration into the eye is limited primarily by the relative impermeability of the cornea, especially against larger molecules.11 Bevacizumab, which is more than threefold larger than ranibizumab, has been shown to penetrate into the posterior segment of the eye after subconjunctival injection, but has minimal penetration to the eye when applied topically in a rabbit model.10 Previous studies using engineered antibody fragments demonstrated penetration into the vitreous with a topically applied 28 kDa antibody fragment and penetration into the anterior chamber with a 67 kDa antibody fragment in a rabbit model.12, 13 Other recent studies have demonstrated that a 26 kDa anti-TNF-α single-chain antibody, which has anti-inflammatory properties, was able to reach the retina with topical administration.14, 15 Moreover, these studies showed that penetration into animal and human eyes via topical application was independent of penetration enhancers and that the applied antibody fragments were resistant to ocular proteases.15 These studies suggest the feasibility of topical administration of antibody fragments for retinal disease, but there have been no published studies evaluating the potential for topical ranibizumab to penetrate to the retina. Using a rabbit model, this study assesses the ocular penetration of topically applied ranibizumab in an effort to elucidate its potential use for the treatment of VEGF-triggered retinal diseases.
Materials and methods
Treatment groups
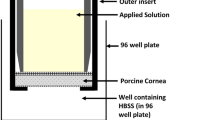
Ranibizumab eye drops (25 μl) were applied to the right eye of rabbits (topical group) according to three regimens of application: every 2 h for 12 h daily (q2hr), four times daily (qid), and twice daily (bid). Five rabbits were included in each subgroup. Intraocular penetration of the drug was assessed at 3, 7, 14, 21, and 28 days following continuous topical application of ranibizumab at the above dosing regimens (Table 1). At each time point, the anterior chamber and vitreous cavity of both eyes, in addition to the blood of one of the rabbits from each subgroup were sampled and analyzed by enzyme-linked immunosorbent assay (ELISA) for ranibizumab detection. The rabbit was then euthanized and both eyes were enucleated and evaluated with confocal immunohistochemistry (CI) to assess the penetration of ranibizumab into the retina. An additional rabbit for each treatment arm was given an intravitreal injection of 50 μl ranibizumab containing 0.05 mg into the right eye (intravitreal group) for comparison, and was similarly sampled for ELISA testing and enucleated at 28 days for confocal microscopy. The left eye of each rabbit in the topical and intravitreal groups was used as an internal negative control.
Sampling of animals
All the surgical procedures were performed under general anesthesia. The aqueous fluid was sampled through insertion of a 25-gauge needle on a tuberculin syringe into the inferior anterior chamber with aspiration of ∼200 μl of aqueous fluid. The vitreous fluid was sampled using a portable 3-port posterior vitrectomy device (Intrector, Insight Instruments, Inc., Stuart, FL, USA). The device was inserted into the vitreous cavity through the pars plana and ∼1 ml of vitreous was retrieved. A blood sample was also aspirated while the rabbits were under general anesthesia. The sampled rabbits were then euthanized and both eyes were enucleated and prepared for CI for ranibizumab detection.
Confocal immunohistochemistry
After enucleation, eyes were fixed in 4% paraformaldehyde at 4 °C for at least 2 days and then cryosectioned at 16 μm thickness. The rabbit eye tissue sections were then incubated with secondary antibody, Cy3-conjugated Fab2 fragment donkey anti-human IgG (Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA), at 1 : 200 dilution in phosphate buffered saline (PBS) solution containing 0.1% Triton X-100 (PBT), for 2 h at room temperature or 4 °C overnight. For positive control, rabbit tissue was incubated with ranibizumab at 1 : 200 in PBT at 4 °C overnight before incubation with secondary antibody. To measure background autofluorescence, tissue was imaged without incubation with secondary antibody and used as the negative control. The left eye of each rabbit was also used as an internal negative control. Samples were mounted to slides in 90% glycerol/2.5% DABCO. Imaging was done with Nikon eclipse E800 confocal microscope (Nikon Inc., Melville, NY, USA) ( × 10 and × 40) and recorded with Perkin-Elmer software (Perkin-Elmer, Waltham, MA, USA).
Enzyme-linked immunosorbent assay
Qualitative ELISA was performed to measure ranibizumab levels. Wells were coated with VEGF at 1 μg/ml overnight before addition of sample. To measure systemic antibodies against ranibizumab (rabbit immune response against the humanized antibody fragment ranibizumab), wells were coated with ranibizumab at 1 μg/ml before adding serum. A volume of 100 μl solution containing 100 μg ranibizumab, and 100 μl PBS were used as the positive and negative control, respectively. A volume of 100 μl of sample was incubated in each well for 1 h at 37 °C. After incubation, plates were incubated with HRP-conjugated secondary antibody (Zymax goat anti-human IgG HRP at 1 : 5000; Invitrogen Corporation, Carlsbad, CA, USA) for 1 h at 37 °C. 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulphonic acid; ABTS) solution was used for detection and optical density was read at 414 nm. The optical density was considered strongly positive if above 1, positive if 0.6–1, undetermined or weakly positive when between 0.3–0.5, and negative if <0.3. ELISA was able to consistently detect ranibizumab as low as 100 ng/ml and intermittently at 10 ng/ml.
Animal care
Throughout the experiment, systemic and ocular monitoring was performed to evaluate for potential ranibizumab side effects in the rabbits. With each topical ranibizumab application, rabbit eyes were examined for ocular reactions by the veterinarian technicians. In addition, the rabbit eyes were periodically examined using a portable slit lamp under anesthesia to evaluate for ocular side effects. The rabbits were also monitored for activity/signs of distress during and after anesthesia, including a charting of their vitals.
The standard Genentech ranibizumab drug product was used in the experiments, which is a preservative-free 10 mg/ml ranibizumab aqueous solution with 10 mM histidine HCl, 10% α,α-trehalose dihydrate, 0.01% polysorbate 20, pH 5.5.
We certify that all applicable institutional and governmental regulations concerning the ethical use of animals were followed during this research.
Results
Confocal microscopy, q2hr topical group
In the first set of experiments, CI of the right eye of the q2hr topical subgroup showed significant ranibizumab penetration into the retina in two out of the five time points tested when compared with the negative control (Figure 1). No ranibizumab signal was detected at 3 days of q2h application by confocal imaging (data not shown) or ELISA (please refer to ELISA results below, Figure 2). At 1 and 2 weeks of continuous q2h topical application, ranibizumab staining was noted in the retina (Figure 1). At 1 week, the staining was most prominent in the outer retina at the level of the photoreceptor layer whereas at 2 weeks the staining was more diffuse throughout the retinal thickness. Ranibizumab staining of the retina as seen by CI consistently disappeared by 3 weeks in all experiments performed despite continuous q2h topical application. This was associated with a reduction in the ranibizumab level detected by ELISA in the vitreous cavity, and with detection of rabbit antibodies against the humanized monoclonal antibody fragment ranibizumab by ELISA in the rabbit serum by 2 weeks (please refer to ELISA results below, Figure 2). Confocal imaging of the left eyes of all rabbits showed no ranibizumab detection at any of the sampling time points (Figure 1).
CI images of rabbit retinas. Top panels from left to right show images of the retina from the positive control incubated with ranibizumab at 1 : 200 before addition of secondary antibody (top left panel), negative control without incubation with secondary antibody (top middle panel), and intravitreal injection of 50 μl ranibizumab containing 0.05 mg (top right panel). Staining is seen in all layers of the retina incubated with ranibizumab (top left panel) whereas the staining is more prominent in the inner retina of the rabbit eye that underwent intravitreal injection ranibizumab (top right panel, arrow). Mild background autofluorescence of the photoreceptor layer (arrow) can be seen in the negative control, but all other layers of the retina show no background (top middle panel). Middle panels show images of the right eye retina after 1, 2, and 3 weeks of q2h ranibizumab drops from left to right. Ranibizumab is detected in the right eye retina at 1 and 2 weeks. Note strong positivity at the level of the photoreceptor layer at 1 week (arrow). At 2 weeks, the signal in the outer retina decreases but it increases in the inner retina (arrow). Ranibizumab staining is no longer present in the right eye retina at 3 weeks. The bottom left panel shows the left eye retina of the same rabbit treated with topical ranibizumab q2h to the right eye for 1 week. The untreated left eye did not show ranibizumab staining. The bottom right panel shows the right eye 4 weeks after intravitreal injection of ranibizumab. OD denotes right eye, OS denotes left eye, and q2h denotes every 2 h Ranibizumab drops. Scale bar, 100 μm.
ELISA for ranibizumab detection in the aqueous, vitreous, and serum following q2h application to the right eye. High levels of ranibizumab are seen in the vitreous at 2 weeks in both eyes and in the vitreous of the right eye at 3 weeks. Low levels of ranibizumab are also detected in the aqueous chamber of the right eye at 2 weeks, but not seen in the aqueous at other time points. Low levels of ranibizumab are detected in the serum at 2 and 3 weeks. Beginning at 2 weeks, antibodies against ranibizumab are detected in the serum and remain high for the duration of the 4-week experiment. The optical density is considered strongly positive if above 1, positive if 0.6–1, undetermined or weakly positive when between 0.3–0.6, and negative if <0.3. OD denotes right eye, OS denotes left eye, AC denotes anterior chamber, and VC denotes vitreous cavity.
Reproducibility experiments with q2h ranibizumab application showed positive ranibizumab signal throughout the retina following 2 weeks of topical application in one out of three rabbits.
ELISA, q2hr topical group
ELISA was strongly positive in the vitreous chambers of the right eye of rabbits at 2 and 3 weeks (two out of the five time points tested) in the first set of q2hr treated rabbits (Figure 2). The aqueous chamber of the right eye of the rabbit at 2 weeks of continuous q2h topical application showed low ranibizumab levels, but the aqueous at other time points was negative. Low levels of ranibizumab were detected in the blood by ELISA starting at 2 weeks. Finally, high levels of rabbit antibodies against ranibizumab were detected by ELISA in the serum by 2 weeks and their levels remained high after this time period. This was associated with a reduction in the ranibizumab level at later time points, despite continuous q2h topical application. ELISA testing of the left eyes of all rabbits showed no ranibizumab detection at any of the sampling time points except at 2 weeks where the signal detected in the vitreous humor of the left eye was exactly the same as in the right eye (Figure 2), which suggests an error in sample labeling.
Repeat experiments that included three rabbits did not show positive ELISA for ranibizumab in the aqueous and vitreous chambers, although the findings were reproducible for ranibizumab and rabbit antibodies against ranibizumab in the serum.
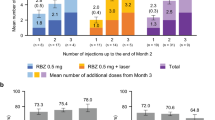
BID and QID topical groups
No significant amounts of ranibizumab were detected in the subgroups of rabbits receiving bid and qid ranibizumab drops either by confocal immunochemistry or by ELISA (Figure 3). Low levels of ranibizumab were detected in the serum as early as 3 days but the levels were variable at later time points. Rabbit antibodies against ranibizumab were consistently found in the serum beginning at 2 weeks, similar to what was noted in the q2hr ranibizumab application subgroup.
CI images and ELISA of rabbits receiving bid ranibizumab drops in the right eye. Top left panel shows an image of the right eye retina after 1 week of receiving bid ranibizumab drops compared with the untreated left eye (top right panel). No ranibizumab was detected in the retina of either eye, which is representative of all time points examined. The bottom graph shows the ELISA results for ranibizumab detection. No significant ranibizumab levels were detectable in the aqueous or vitreous at any time point. Low levels of ranibizumab were detected in the serum by 3 days and seen at varying low levels at later time points. Antibodies against ranibizumab were first detectable at 2 weeks and their level remained high for the duration of the experiment. OD denotes right eye, OS denotes left eye, AC denotes anterior chamber, VC denotes vitreous chamber, and bid denotes twice a day ranibizumab drops. Scale bar, 100 μm.
Intravitreal group
Intravitreal injection of ranibizumab into the right eye of each of three rabbits was performed for comparison. After 4 weeks intravitreal injection, confocal microscopy disclosed mild diffuse staining of ranibizumab throughout all the retinal layers (Figure 4). After 3 days intravitreal injection of ranibizumab, ELISA detected very high levels of ranibizumab in both the anterior chamber and the vitreous humor in the injected right eye of these rabbits, and also high levels of ranibizumab in the anterior chamber of the left eye and in the serum (Figure 4). The left eye ranibizumab signal was no longer detectable by 1 week and the signal in the right eye and serum decreased during the course of the 4-week experiments especially by 2 weeks following the injection. Similar to the topical groups, high levels of rabbit antibodies against ranibizumab were detected by ELISA in the serum at 2 weeks (Figure 4). The levels of the rabbit antibodies against ranibizumab remained high after this time period.
CI images and ELISA of rabbits after intravitreal injection of ranibizumab to the right eye. After 4 weeks the intravitreal injection in the right eye, significant ranibizumab staining was noted in the retina of the right eye (top left panel) compared with the left eye (top right panel). On ELISA (bottom graph), high levels of ranibizumab were measurable at 3 days in the right eye in both the aqueous and vitreous fluid, the left eye aqueous fluid, and in the serum. Ranibizumab was no longer detectable in the left eye by 1 week and the signal in the right eye and serum decreased during the course of the 4-week experiments especially by 2 weeks following the injection. Beginning at 2 weeks, a high level of antibodies against ranibizumab was detected in the serum and remained high for the duration of the experiment. OD denotes right eye, OS denotes left eye, AC denotes anterior chamber, and VC denotes vitreous chamber. Scale bar, 100 μm.
Complications
Ranibizumab eye drops were well tolerated and no signs of ocular or systemic toxicity were observed in any of the rabbits. One of the rabbits in the intravitreal group developed a conjunctival reaction that was successfully treated with a short course of a steroid/antibiotic ocular formulation.
Discussion
Confocal microscopy and ELISA findings in this study suggest that ranibizumab applied q2h may be able to penetrate into rabbit eyes. CI findings suggest that topical ranibizumab applied q2h may be able to reach the retina after 3–7 days of continuous administration, as indicated by the positive staining that was noted in the retina in the right eye at 7 and 14 days of q2h administration.
Entry through a trans-scleral route is the most likely route of entry to the posterior segment given the relatively large size of the ranibizumab molecule (48 kDa). Past studies indicate that molecules as large as whole antibodies (150 kDa) are permeable to the sclera.16, 17 These larger molecules are thought to pass through the limbal conjunctival epithelium and then diffuse through the sclera, which is 15–25 times more permeable than the cornea.17 Evidence for trans-scleral penetration to the posterior segment for smaller sized antibody fragments has been growing in recent literature.14, 15 Three pieces of evidence in this experiment support a trans-scleral rather than a trans-corneal route of entry into the rabbit eye following q2h application. First, ranibizumab was detected in the retina by confocal microscopy 1 week before its detection in the aqueous and vitreous by ELISA, which occurred at 2 weeks with a 1-week lag. In addition, ranibizumab signal was lost from the retina at 3 weeks when imaged with confocal microscopy, but the ranibizumab signal was still present in the vitreous humor at 3 weeks and was not lost until 4 weeks. Therefore, the appearance and disappearance of ranibizumab in the retina occurred 1 week before that in the vitreous humor. Second, ELISA signal was much higher in the vitreous than in the aqueous since its detection by ELISA at 2 weeks (Figure 2). Third, confocal microscopy for the topical group disclosed a more intense staining in the outer retina than in the inner retina at 1 week, and by 2 weeks, the confocal microscopy-staining pattern became more diffuse throughout the retina with a more intense signal in the inner retina than at 1 week (Figure 1, middle row). All these findings do not support an antero–posterior entry route into the eye, but rather suggest that ranibizumab was gradually building up in the eye cavity from posterior structures. This becomes even more evident by comparison to the staining pattern of the retina following intravitreal injection where the staining was more intense in the inner retina compared with the outer retina, particularly at the level of the ganglion cell and nerve fiver layers (Figure 1, top right panel).
Delivery to the retina via systemic absorption is a remote possibility although ranibizumab was detected in the serum at low concentrations even in the BID topical application group. Systemic delivery is less likely because the levels remain lower in the blood than those found in the vitreous humor of the q2h treated rabbits. Moreover, a systemic route would be expected to yield similar staining patterns in both eyes, which was not the case in the study. However, the detection of ranibizumab in the serum of the treated rabbits raises concerns regarding the systemic safety of topical application in humans. Although this ultimately requires safety studies, the finding of higher levels of ranibizumab in the rabbit serum in the intravitreal group compared with that in the q2h topical group (Figures 2 and 4) suggests that the systemic safety profile following topical administration should not be drastically different from that following intravitreal injection.
Interestingly, at 2 weeks of q2h ranibizumab application to the right eye, ranibizumab was also detected in the vitreous humor of the left eye by ELISA (Figure 2). It is believed that this finding reflects a mislabeled specimen because the optical density recorded from the left vitreous specimen was identical to that recorded from the right as Figure 2 indicates. It is also possible that this occurred through systemic absorption of ranibizumab into the serum, which was then delivered to the contralateral eye; however, the level of ranibizumab found in the left vitreous was far higher than levels found in the serum, making this less likely. Another possible explanation comes from previous studies that demonstrated accumulation of insulin and tropicamide in the contralateral eye in decapitated rats that involved a mechanism that does not involve systemic uptake.18 It was hypothesized that there is a direct route of communication between the two eyes that is independent of systemic uptake. Ranibizumab may have reached the left eye in the rabbit treated for 2 weeks with q2h ranibizumab in a similar route.
The ranibizumab signal in the retina disappeared at 3 weeks despite continued q2h drop application. This may be partially explained by the formation of antibodies against ranibizumab in the rabbit. Antibodies against ranibizumab were first detected in the blood by ELISA at 2 weeks, and concentrations of these antibodies remained at high levels after this time period. This was not unexpected because ranibizumab is a humanized monoclonal antibody fragment to which the rabbit was expected to mount an immune response. Similarly, high levels of rabbit antibodies against ranibizumab were detected by ELISA in the rabbit serum in the intravitreal group. This also may suggest that both topically and intravitreally administered ranibizumab are associated with a similar systemic immune response in the rabbit, which further supports a similar systemic safety profile between the two methods of administration. This immune response by the rabbit was not associated with ocular manifestations detectable by the screening methods used. Only one of the rabbits in the intravitreal injection group developed a conjunctival reaction that was successfully treated with a short course of a steroid/antibiotic combination.
Decreasing the frequency of topical ranibizumab administration to twice and four times a day resulted in failure of ranibizumab to penetrate into the eye as evidenced by confocal and ELISA studies. Furthermore, repeat experiments showed variable results with q2h ranibizumab drops, suggesting that a frequent dosing regimen of q2h application is likely at the threshold of topical penetration, which may be related to the size of the ranibizumab molecule (48 kDa). Past studies have shown that molecules as large as 28 kDa applied topically are able to penetrate to the posterior segment, whereas whole antibody molecules (>149 kDa), such as Avastin, are not able to penetrate across the ocular surface when delivered topically.10, 12 However, our findings are still promising because only small amounts of ranibizumab are likely required to have an inhibitory effect on VEGF activity. Previous studies indicate that only 11–27 ng/ml of ranibizumab is required to inhibit biological activity of VEGF by 50% in an in vitro cellular proliferation assay. A similar study demonstrated that a ranibizumab concentration as low as 120 ng/ml could inhibit VEGF activity.19 Therefore, although topical administration of ranibizumab in its current formulation is unlikely a feasible therapeutic means in humans because very high frequency of topical administration was required to achieve ocular penetration in our study, future alterations in the molecule or alternative vehicles may increase its permeability.
Although topically applied ranibizumab may be at the threshold of penetration, our experiments support the current use of intravitreal ranibizumab and demonstrate robust ranibizumab signal within the vitreous and retina following intravitreal injection with persistent signal within the vitreous and retina 4 weeks after intravitreal injection. This is a similar pharmacokinetic profile to that seen in previous studies that evaluated intravitreal ranibizumab and found a t1/2 of 2.88–3 days in monkeys and rabbits.20, 21, 22
One caveat with the study is the usage of rabbit as an animal model. The rabbit eye has a vitreous volume of ∼1.5 ml (one third the volume in humans), a larger lens, and a less vascular retina compared with humans; therefore, the pharmacokinetics of topically applied ranibizumab may slightly differ between the rabbit and humans. However, there are three lines of evidence that suggest that our findings in the rabbit may be extrapolated to the human. First, the rabbit is an established and often used model to study the pharmacokinetics of ocular drugs, including ranibizumab, bevacizumab, and other molecules.21, 22, 23, 24, 25 Second, the pharmacokinetics of intravitreally administered ranibizumab in the monkey is very similar to what was found in the rabbit, which further supports the rabbit as an animal model.20 Third, the sclera of the rabbit has fairly similar permeability to the human sclera, which is also permeable to molecules with a molecular weight of 70 kDa,16, 26 This last finding is especially pertinent to our study because we propose a trans-scleral route of penetration to the retina with topical ranibizumab.
Overall, our study provides evidence that topical ranibizumab in its current formulation may have the potential to penetrate into the eye, but appears to require an excessive frequency of administration that makes the topical route a less attractive option to pursue for the treatment of retinal vascular diseases such as diabetic macular edema and NVAMD in humans at this point. Further experiments are required to confirm the reproducibility of our findings, elucidate the frequency of ranibizumab drops required, and explore the route of entry to the retina. Perhaps future experiments will produce a vehicle or alteration in the molecule that will increase the permeability of topically administered ranibizumab, leading to a therapeutic alternative that efficiently penetrates the eye.

References
Rosenfeld PJ, Brown DM, Heier JS et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ . Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 2011; 364: 1897–1908.
Michaelides M, Kaines A, Hamilton RD et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: report 2. Ophthalmology 2010; 117: 1078–1086 e2.
Diago T, McCannel CA, Bakri SJ, Pulido JS, Edwards AO, Pach JM . Infectious endophthalmitis after intravitreal injection of antiangiogenic agents. Retina 2009; 29: 601–605.
Fintak DR, Shah GK, Blinder KJ, Regillo CD, Pollack J, Heier JS et al. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina 2008; 28: 1395–1399.
Pilli S, Kotsolis A, Spaide RF, Slakter J, Freund KB, Sorenson J et al. Endophthalmitis associated with intravitreal anti-vascular endothelial growth factor therapy injections in an office setting. Am J Ophthalmol 2008; 145: 879–882.
Wu L, Martinez-Castellanos MA, Quiroz-Mercado H, Arevalo JF, Berrocal MH, Farah ME et al. Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol 2008; 246: 81–87.
Thrimawithana TR, Young S, Bunt CR, Green C, Alany RG . Drug delivery to the posterior segment of the eye. Drug Discov Today 2011; 16: 270–277.
Hughes PM, Olejnik O, Chang-Lin JE, Wilson CG . Topical and systemic drug delivery to the posterior segments. Adv Drug Deliv Rev 2005; 57: 2010–2032.
Nomoto H, Shiraga F, Kuno N, Kimura E, Fujii S, Shinomiya K et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Invest Ophthalmol Vis Sci 2009; 50: 4807–4813.
Prausnitz MR, Noonan JS . Permeability of cornea, sclera, and conjunctiva: a literature analysis for drug delivery to the eye. J Pharm Sci 1998; 87: 1479–1488.
Williams KA, Brereton HM, Farrall A, Standfield SD, Taylor SD, Kirk LA et al. Topically applied antibody fragments penetrate into the back of the rabbit eye. Eye (Lond) 2005; 19: 910–913.
Thiel MA, Coster DJ, Standfield SD, Brereton HM, Mavrangelos C, Zola H et al. Penetration of engineered antibody fragments into the eye. Clin Exp Immunol 2002; 128: 67–74.
Furrer E, Berdugo M, Stella C, Behar-Cohen F, Gurny R, Feige U et al. Pharmacokinetics and posterior segment biodistribution of ESBA105, an anti-TNF-alpha single-chain antibody, upon topical administration to the rabbit eye. Invest Ophthalmol Vis Sci 2009; 50: 771–778.
Ottiger M, Thiel MA, Feige U, Lichtlen P, Urech DM . Efficient intraocular penetration of topical anti-TNF-alpha single-chain antibody (ESBA105) to anterior and posterior segment without penetration enhancer. Invest Ophthalmol Vis Sci 2009; 50: 779–786.
Ambati J, Canakis CS, Miller JW, Gragoudas ES, Edwards A, Weissgold DJ et al. Diffusion of high molecular weight compounds through sclera. Invest Ophthalmol Vis Sci 2000; 41: 1181–1185.
Koevary SB . Pharmacokinetics of topical ocular drug delivery: potential uses for the treatment of diseases of the posterior segment and beyond. Curr Drug Metab 2003; 4: 213–222.
Patsiopoulos G, Lam V, Lake S, Koevary SB . Insulin and tropicamide accumulate in the contralateral, untreated eye of rats following ipsilateral topical administration by a mechanism that does not involve systemic uptake. Optometry 2003; 74: 226–232.
Klettner A, Roider J . Comparison of bevacizumab, ranibizumab, and pegaptanib in vitro: efficiency and possible additional pathways. Invest Ophthalmol Vis Sci 2008; 49: 4523–4527.
Gaudreault J, Fei D, Rusit J, Suboc P, Shiu V . Preclinical pharmacokinetics of Ranibizumab (rhuFabV2) after a single intravitreal administration. Invest Ophthalmol Vis Sci 2005; 46: 726–733.
Gaudreault J, Fei D, Beyer JC, Ryan A, Rangell L, Shiu V et al. Pharmacokinetics and retinal distribution of ranibizumab, a humanized antibody fragment directed against VEGF-A, following intravitreal administration in rabbits. Retina 2007; 27: 1260–1266.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Ezzat MK, Singh RJ . Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology 2007; 114: 2179–2182.
Scholes GN, O′Brien WJ, Abrams GW, Kubicek MF . Clearance of triamcinolone from vitreous. Arch Ophthalmol 1985; 103: 1567–1569.
Fauser S, Kalbacher H, Alteheld N, Koizumi K, Krohne TU, Joussen AM . Pharmacokinetics and safety of intravitreally delivered etanercept. Graefes Arch Clin Exp Ophthalmol 2004; 242: 582–586.
Iyer MN, He F, Wensel TG, Mieler WF, Benz MS, Holz ER . Clearance of intravitreal moxifloxacin. Invest Ophthalmol Vis Sci 2006; 47: 317–319.
Olsen TW, Edelhauser HF, Lim JI, Geroski DH . Human scleral permeability. Effects of age, cryotherapy, transscleral diode laser, and surgical thinning. Invest Ophthalmol Vis Sci 1995; 36: 1893–1903.
Acknowledgements
We thank Barry Condron for his expertise and assistance with the confocal microscopy, and Iggy Provencio and the UVA Research Histology Core for their help with cryosectioning. This work was supported by the Richmond Eye and Ear Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented at ARVO 2009.
Rights and permissions
About this article
Cite this article
Chen, J., Ebmeier, S., Sutherland, W. et al. Potential penetration of topical ranibizumab (Lucentis) in the rabbit eye. Eye 25, 1504–1511 (2011). https://doi.org/10.1038/eye.2011.225
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.225
Keywords
This article is cited by
-
Safety Assessment of Formulation Vehicles Following Intravitreal Administration in Rabbits
Pharmaceutical Research (2018)
-
A comparative study of different concentrations of topical bevacizumab on the recurrence rate of excised primary pterygium: a short-term follow-up study
International Ophthalmology (2016)