Abstract
Purpose
To compare two ophthalmic viscosurgical devices (OVDs), DisCoVisc (viscous dispersive) and Healon5 (viscoadaptive), in terms of their overall clinical performance during phacoemulsification and intraocular lens (IOL) implantation.
Methods
In 323 patients (DisCoVisc; 157, Healon5; 166), the surgeons evaluated on a three-point scale, the maintenance of anterior chamber (AC) during continuous curvilinear capsulorhexis (CCC), maintenance of AC during IOL implantation, retention during phacoemulsification, ease of injection, facilitation of CCC, transparency during surgery, and ease of removal from the eye. The time needed to completely remove OVDs after IOL implantation was measured. Masked examiners measured intraocular pressure (IOP), corneal thickness, and corneal endothelial cell count up to 90 days postoperatively.
Results
DisCoVisc was assessed to be significantly better than Healon5 in maintenance of AC during CCC (P=0.0008, Cochran–Mantel–Haenszel test) and IOL implantation (P=0.0055), retention during phacoemulsification (P=0.0009), ease of injection (P<0.0001), facilitation of CCC (P<0.0001), transparency (P<0.0001), and ease of removal (P<0.0001). The washout time was 29.6±13.4 and 36.2±17.5 s in the DisCoVisc and Healon5 groups, respectively (P=0.0002, unpaired t-test). The mean endothelial cell loss was 1.8±8.7% in the DisCoVisc group and 3.8±8.3% in the Healon5 group (P=0.0358). There were no statistically significant between-group differences in IOP and corneal thickness.
Conclusion
DisCoVisc was better retained in the eye during phacoemulsification and was easier to remove after IOL implantation. The corneal endothelial cell loss was significantly less with DisCoVisc than with Healon5. It was indicated that the whole surgical process can be efficiently covered by DisCoVisc alone.
Similar content being viewed by others
Introduction
The introduction of ophthalmic viscosurgical devices (OVDs) for use in ophthalmic surgery has had a significant effect on the practise of ophthalmology. OVDs have become indispensable tools in a variety of ophthalmic surgical procedures, especially in cataract surgery. The most important functions of OVDs during cataract surgery are maintenance of the anterior chamber (AC) and protection of the ocular tissues, in particular the corneal endothelium. During phacoemulsification, OVDs can protect the corneal endothelium by preventing the direct contact of debris-bearing turbulence and surgical instruments.
The property of a viscoelastic formulation is closely tied to its physicochemical and rheological properties.1, 2 Higher viscosity cohesive OVDs and lower viscosity dispersive OVDs have their own unique advantages and disadvantages. High-viscosity cohesive OVDs help to maintain and preserve space as well as to displace and stabilize tissues. These materials, however, tend to easily flow out of the eye during phacoemulsification. Low-viscosity dispersive OVDs tend to remain in the eye adjacent to the corneal endothelium, providing potential protection during phacoemulsification. The disadvantage of this type of OVDs is that they poorly maintain space and are sometimes difficult to remove.
A viscoadaptive viscoelastic, Healon5, belongs to another class of OVDs.3, 4, 5 Its distinguishing characteristic is that the rheological behaviour changes under varying conditions of turbulence. It exerts an effect as a very viscous, cohesive viscoelastic agent at low flow rate and as a pseudodispersive viscoelastic agent at higher flow rate. A previous clinical study showed that the viscoadaptive OVD (Healon5) was superior to the cohesive OVD (Healon) in retention during phacoemulsification, AC maintenance during anterior capsulotomy, and facilitation of intraocular lens (IOL) implantation.6 On the other hand, injection and removal of the viscoadaptive OVD were judged to be more difficult than the cohesive OVD.6
Recently, a new class of OVD, DisCoVisc, has been developed and introduced in the market.7 DisCoVisc is a viscoelastic solution of sodium chondroitin sulphate and sodium hyaluronate, having a viscosity of 75 000±35 000 milliPascal-seconds (mPas) at a shear rate of 1/s and 25 °C. Each millilitre of DisCoVisc contains not more than 40 mg sodium chondroitin sulphate and 17 mg sodium hyaluronate. It has been claimed that DisCoVisc has an intermediate cohesive/dispersive index, facilitating both space maintenance and tissue protection. Experimental studies reported that DisCoVisc showed excellent retention during phacoemulsification.8, 9, 10 When compared with the viscoadaptive Healon5, DisCoVisc was retained better in the chamber and was easier to remove.9
The clinical usefulness of DisCoVisc in cataract surgery, however, has not been reported, except for one study that compared DisCoVisc and soft-shell technique using Viscoat and Provisc.11 We conducted the current prospective randomized clinical study to compare the performance of DisCoVisc and Healon5 regarding maintenance of the AC during continuous curvilinear capsulorhexis (CCC) and IOL implantation, retention during phacoemulsification, ease of injection, facilitation of CCC, transparency during surgery, and ease of removal from the eye. The time required to remove from the eye after IOL implantation was measured and compared. The intraocular pressure (IOP), corneal endothelial cell count, and corneal thickness were also assessed as safety-related parameters.
Materials and methods
Subjects
A multicentre randomized study was carried out to compare DisCoVisc and Healon5 during phacoemulsification and IOL implantation. Patients aged ⩾40 years with age-related cataract requiring surgery were enroled in the study. Exclusion criteria were: IOP of ⩾22 mm Hg, glaucoma in either eye, proliferative diabetic retinopathy, corneal endothelial damage (cell count of <1500/mm2), history of uveitis, and congenital eye diseases.
Six surgical centres participated in the study. The patients were randomly assigned to either of the two study groups according to a computer-generated, randomized list prepared by the case registration centre (ACRONET Co., Tokyo, Japan). The randomized list was stratified for multiple institutions and implemented for each block of patients within the individual institutions. On the basis of information provided by the surgeon, the case registration centre enroled the patients, after confirming that each patient met all inclusion criteria and did not violate any of the exclusion criteria. After registration, the surgeon was advised by the case registration centre about the registration number of each patient and the OVD assigned according to the randomized list.
A total of 323 eyes of 323 patients were included, 157 for the DisCoVisc group (male/female; 54/103, 70.3±8.2 years old, mean±SD) and 166 for the Healon5 group (66/100, 70.3±7.9 years old). Only one eye of each patient was included in the study.
The study protocol was approved by the institutional review board of each participating surgical centre, and the study was conducted in accordance with the Declaration of Helsinki. All patients provided informed consent in a written form before participation. The study was part of the phase III clinical trial under the Ministry of Health, Labor, and Welfare of Japan.
Surgery
The OVDs to be used were made known to the surgeons as it was difficult to maintain the blinding of the surgeons because of the different physicochemical properties of OVDs. All postoperative measurements and observations were conducted by investigators other than the surgeons, who were not informed about the allocated OVD.
Six surgeons at six surgical centres performed phacoemulsification and foldable IOL implantation. IOLs used were hydrophobic acrylic foldable three-piece IOLs (MA60BM; Alcon, Fort Worth, TX, USA) or single-piece IOLs (SA60AT; Alcon). Same products were used within each surgical centre. After IOL implantation, DisCoVisc was removed using the irrigation/aspiration (I/A) tip without any special washout techniques, whereas Healon5 was washed out using the behind-the-lens technique or Rock’n Roll technique.12, 13
Data collection
The surgeons subjectively assessed the clinical performance (efficacy) of DisCoVisc and Healon5 during surgery based on seven criteria: maintenance of the AC during CCC, maintenance of the AC during IOL implantation, retention during phacoemulsification, ease of injection, facilitation of CCC, transparency during surgery, and ease of removal from the eye. The surgeons evaluated each OVD on a three-point rating scale (1=good, 2=average, and 3=poor).
The time needed to completely remove the OVDs from the chamber with the I/A tip was recorded.
The IOP was measured using the Goldmann applanation tonometer preoperatively and at 5 and 24 h, and 7, 30, and 90 days postoperatively. The specular microscopy was performed preoperatively and 90 days after surgery. Corneal thickness was measured with an ultrasound pachymeter preoperatively and at 24 h, and 7, 30, and 90 days after surgery.
Statistical analysis
The time course of changes in numerical parameters was analysed using analysis of variance. Inter-group difference in numerical data was analysed with the unpaired t-test. The surgeons’ assessment scores of clinical performance of OVDs and the incidence of adverse effects, inducing IOP elevation, were analysed using the Cochran–Mantel–Haenszel test. Corneal endothelial count before and 90 days after surgery was compared with the paired t-test. A P-value of <0.05 was considered significant.
A prestudy power calculation based on the data of the International Organization for Standardization (ISO) 15798:2001(E) Annex D indicated that a sample size of 135 eyes in each group would be sufficient to examine the inter-group difference in incidence of IOP elevation over 30 mm Hg using a significance level of 10% (α) and a power of 80% (1−β). The calculation based on ISO 16671:2003(E) Annex F revealed that the lower limit of 95% confidence intervals will exceed −7.5% (non-inferiority margin) with a power of 80% (1−β) in a sample size of 135.
Results
Among the subjects enroled, 6 patients (3 in the DisCoVisc and 3 in the Healon5 groups) were excluded from the analysis because of intraoperative complication (1 in DisCoVisc), use of another IOL (1 in DisCoVisc and 1 in Healon5) or OVD (1 in Healon5), or lost to follow-up (1 in DisCoVisc and 1 in Healon5). Thus, the data in a total of 317 eyes (154 in DisCoVisc and 163 in Healon5) were analysed. The number of eyes evaluated at each predetermined examination point is shown in Table 1.
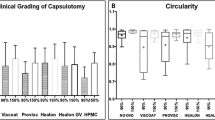
Intraoperative performance of DisCoVisc and Healon5 was evaluated by the surgeons (Table 2). DisCoVisc was assessed to be significantly better than Healon5 in terms of maintenance of the AC during CCC (P=0.0008), maintenance of the AC during IOL implantation (P=0.0055), retention during phacoemulsification (P=0.0009), ease of injection (P<0.0001), facilitation of CCC (P<0.0001), transparency during surgery (P<0.0001), and ease of removal from the eye (P<0.0001).
The time needed to completely remove the OVDs from the chamber with the I/A tip was 29.6±13.4 and 36.2±17.5 s in the DisCoVisc and Healon5 groups, respectively. There was a significant difference between the two groups (P=0.0002).
Safety-related parameters were evaluated by the investigators other than the surgeons. The time course of changes in IOP is shown in Figure 1. In both groups, IOP reached the peak at 5 h after surgery, followed by gradual decreases to the preoperative level by 7 days postoperatively. There was no significant inter-group difference in IOP at any examination points. At 5 h postoperatively, IOP above 30 mm Hg was observed in 11 eyes (7.2%) of the DisCoVisc group and 12 eyes (7.4%) of the Healon5 group. The incidence did not differ significantly (P=0.954). The IOP quickly returned to the normal level in all cases.
The mean corneal endothelial cell loss at 90 days postoperatively was 1.8±8.7% in the DisCoVisc group and 3.8±8.3% in the Healon5 group. There was a significant difference between the groups (P=0.0358).
The time course of changes in corneal thickness is shown in Figure 2. The thickness reached its peak at 24 h after surgery, and returned to the preoperative level by 7 days after surgery. There was no significant inter-group difference on any examination occasions.
There were no intraoperative complications related to OVDs, including thermal burn of the wound. Besides IOP elevation as mentioned above, there was one case of transient mild corneal oedema (0.6%) and macular oedema (0.6%) in the Healon5 group, but no other postoperative complications were encountered. There was no significant inter-group difference in the incidence of postoperative complications. No patients in either group lost best corrected visual acuity by one line or more compared with the preoperative level.
Discussion
DisCoVisc is a viscous-dispersive OVD, having the properties of both cohesive and dispersive OVDs.7 A previous experimental study showed that the retention and removal properties of DisCoVisc fell between cohesive Provisc and dispersive Viscoat, and DisCoVisc was retained in the AC during phacoemulsification better than Healon5, whereas removal of DisCoVisc with the I/A tip was easier than Healon5.9 We obtained similar results in the current clinical study. DisCoVisc was rated better than Healon5 in terms of maintenance of the AC during CCC and IOL implantation as well as retention during phacoemulsification. These results seem to reflect the more dispersive property of DisCoVisc, against the pseudodispersive nature of Healon5. On the other hand, removal time of OVDs with the I/A tip was significantly shorter with DisCoVisc than with Healon5. The surgeons’ subjective assessment also indicated that DisCoVisc is significantly easier to remove than Healon5 after IOL implantation. Clinically, it is known that Healon5 is difficult to be washed out at the end of surgery because of the presence of an IOL. Healon5 is often trapped behind the IOL,2 especially so with the acrylic foldable IOL.14 The viscoadaptive OVDs are so rigid to permit scrolling around obstacles in the eye (IOLs), resulting in interrupted contact with the aspiration port.2 The OVD fragment behind the IOL is exposed to too little turbulent flow to move towards the aspiration port, unless the I/A tip is placed behind the IOL or a special technique is used. DisCoVisc is not so rigid and has sufficient cohesion to stay together in the presence of aspiration and is supple enough to bend around obstacles. The behind-the-lens technique or Rock’n Roll technique is not necessary for the washout of DisCoVisc.
We found that corneal endothelial cell loss was significantly less in the DisCoVisc group than in the Healon5 group, most likely because of better retention of DisCoVisc than Healon5 during phacoemulsification. On the other hand, there was no inter-group difference in the mean corneal thickness after surgery. This was probably because this study was conducted in patients with simple age-related cataract without any other ocular and systemic complications. Our study population did not include those cases with small pupil, very shallow chamber, compromised endothelial cell function, corneal disorder, and blood-aqueous barrier dysfunction. It seems that the viscous-dispersive nature of DisCoVisc would be more beneficial in these difficult cases, in which clinically measurable differences in the surgical outcomes might be anticipated. Another prospective randomized study will be needed to prove this postulate.
In this study, it was found that DisCoVisc showed significantly better performance than Healon5 in terms of ease of injection and removal. Ease of injection is because of the lower viscosity of this product. Ease of removal is an important issue. If the OVD is not removed completely, IOP can increase postoperatively. In this study, the surgeons rated DisCoVisc favourably regarding the ease of removal against Healon5. This was partly because the behind-the-lens technique or Rock’n Roll technique was compulsory for the removal of Healon5 in this study, whereas no special technique was required for DisCoVisc. Another reason is that removal time was significantly longer in the Healon5 group than in the DisCoVisc group. This was primarily because it takes longer to aspirate a more viscous mass, of similar volume, through similar-sized aperture, and with similar vacuum force, compared with a less viscous mass. These factors seem to have contributed to the different scores for these OVDs. The postoperative IOP, however, did not differ significantly between groups, indicating that both OVDs were effectively and successfully washed out.
DisCoVisc was also assessed to be superior to Healon5 regarding transparency during surgery and facilitation of CCC. Transparency during surgery may be related to the appearance of interface between the aqueous humour and the OVD. Because Healon5 tends to be aspirated gradually during phacoemulsification, such interface may develop during surgery, which can somewhat interfere visibility within the eye. Meanwhile, when the AC is filled with OVD, there is no interface between the aqueous humour and the OVD, and the clarity of the AC is preserved. This will be the case of DisCoVisc, which is retained in the eye for a longer period of time during phacoemulsification than Healon5.9 The facilitation of CCC seems to be related to the viscosity of OVDs. Healon5 is thicker and heavier, leading to the surgeons’ review that CCC was more difficult to control when the chamber is filled with this agent.
This study has several limitations. First, only routine cataract cases were included in the subjects. In practise, the number of complicated cases has been increasing, at least not decreasing. Evaluation of OVDs in these tough cases will be important. Second, we only compared DisCoVisc and Healon5. In the market, there are many other OVDs with different properties. Comparison of DisCoVisc with other products will be interesting. Third, although all postoperative measurements were conducted by masked examiners, the surgeons were not masked to the type of OVDs. Because the physicochemical properties of DisCoVisc and Healon5 are so different, it was difficult to maintain the blinding of the surgeons.
This study clearly showed the advantageous features of DisCoVisc in cataract surgery; that is, greater retention in the eye during phacoemulsification and easier removal from the eye after IOL implantation. The former has been known as the characteristic of low-viscosity dispersive OVD, and the latter has been recognized as the feature of high-viscosity cohesive agents. Greater retention in the eye during phacoemulsification resulted in less damage to the corneal endothelial cells. The viscous-dispersive nature of DisCoVisc made it possible to combine these two different traits into one viscoelastic substance. Thus, the whole process of cataract surgery can be efficiently covered by one OVD, which can be of merit in ophthalmic practise both economically and medically.

References
Arshinoff SA . Dispersive-cohesive viscoelastic soft shell technique. J Cataract Refract Surg 1999; 25: 167–173.
Arshinoff SA, Wong E . Understanding, retaining, and removing dispersive and pseudodispersive ophthalmic viscosurgical devices. J Cataract Refract Surg 2003; 29: 2318–2323.
Schwenn O, Dick HB, Krummenauer F, Christmann S, Vogel A, Pfeiffer N . Healon5 vs Viscoat during cataract surgery: intraocular pressure, laser flare and corneal changes. Graefes Arch Clin Exp Ophthalmol 2000; 238: 861–867.
Dick HB, Krummenauer F, Augustin AJ, Pakula T, Pfeiffer N . Healon5 viscoadaptive formulation: comparison to Healon and Healon GV. J Cataract Refract Surg 2001; 27: 320–326.
Tetz MR, Holzer MP, Lundberg K, Auffarth GU, Burk RO, Kruse FE . Clinical results of phacoemulsification with the use of Healon5 or Viscoat. J Cataract Refract Surg 2001; 27: 416–420.
Oshika T, Eguchi S, Oki K, Yaguchi S, Bissen-Miyajima H, Ota I et al. Clinical comparison of Healon5 and Healon in phacoemulsification and intraocular lens implantation; randomized multicenter study. J Cataract Refract Surg 2004; 30: 357–362.
Arshinoff SA, Jafari M . New classification of ophthalmic viscosurgical devices—2005. J Cataract Refract Surg 2005; 31: 2167–2171.
Petroll WM, Jafari M, Lane SS, Jester JV, Cavanagh HD . Quantitative assessment of ophthalmic viscosurgical device retention using in vivo confocal microscopy. J Cataract Refract Surg 2005; 31: 2363–2368.
Oshika T, Okamoto F, Kaji Y, Hiraoka T, Kiuchi T, Sato M et al. Retention and removal of a new viscous dispersive ophthalmic viscosurgical device during cataract surgery in animal eyes. Br J Ophthalmol 2006; 90: 485–487.
Bissen-Miyajima H . In vitro behavior of ophthalmic viscosurgical devices during phacoemulsification. J Cataract Refract Surg 2006; 32: 1026–1031.
Praveen MR, Koul A, Vasavada AR, Pandita D, Dixit NV, Dahodwala FF . DisCoVisc versus the soft-shell technique using Viscoat and Provisc in phacoemulsification: randomized clinical trial. J Cataract Refract Surg 2008; 34: 1145–1151.
Tetz MR, Holzer MP . Two-compartment technique to remove ophthalmic viscosurgical devices. J Cataract Refract Surg 2000; 26: 641–643.
Zetterstrom C, Wejde G, Taube M . Healon5: Comparison of 2 removal techniques. J Cataract Refract Surg 2002; 28: 1561–1564.
Auffarth GU, Holzer MP, Vissesook N, Apple DJ, Völcker HE . Removal times and techniques of a viscoadaptive ophthalmic viscosurgical device. J Cataract Refract Surg 2004; 30: 879–883.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Oshika, T., Bissen-Miyajima, H., Fujita, Y. et al. Prospective randomized comparison of DisCoVisc and Healon5 in phacoemulsification and intraocular lens implantation. Eye 24, 1376–1381 (2010). https://doi.org/10.1038/eye.2010.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.47
Keywords
This article is cited by
-
Implantation of intraocular lens without viscoelastic agent in phacoemulsification cataract surgery
International Ophthalmology (2022)