Abstract
Purpose
Pakistan, like many other developing countries, is caught in the vicious cycle of poverty, illiteracy, violence, and disease. Right from its inception, it has been facing serious challenges of fast growing population, longevity, unemployment, wars, floods, double burden of diseases including blindness, as well as earthquakes, insurgencies, and political instability. Despite such challenges, the country has managed to reduce the burden of blindness from 1.78% in 1987-88 to 0.9% in 2003.This paper will highlight the methods used to achieve such a difficult goal.
Methods
The country used the report of the World Health Organization (WHO) temporary consultant as the initial tool for advocacy to obtain political and professional commitment. Results from the first National Blindness Survey 1987–1990 were used as baseline for development of the programme. Under the Ministry of Health, national and provincial committees with respective coordinators were constituted. To ensure access and equity, the national programme was developed on the basis of district comprehensive eye care services. The concept was carefully tested in a laboratory and then piloted in a real district before it was rolled over to the country. Strong national institutes for human resource development, research and development, and service delivery were established. A strong network of high-quality national institutes was set up and run by powerful national non-governmental organizations. The second National Blindness Survey evaluated the achievements of the programme in 2001–2003.
Conclusion
National prevalence of blindness was reduced by 100% by improving the uptake of services at the district level, especially by females.
Similar content being viewed by others
Introduction
Pakistan, a developing country situated in the Eastern Mediterranean region (EMR) of the World Health Organization (WHO), is bordered by India, Afghanistan, Iran, and China.
At the time of independence, the country had inherited a very poor infrastructure for health delivery and health human resource development. The country inherited two medical colleges, 78 registered doctors, and very few nurses.1
Since its inception, the country has been facing problems of refugee2 influx, floods, earthquakes, rapidly growing population, ageing, double burden of diseases including blindness, wars, insurgencies, and political instability.
Health has never been a priority in the country's budgetary allocations.3 The country naturally suffered the worst health indicators in the region.4
At the time of partition, there was no organized system for eye health in the country. Most of the eye care services in the south of the country were provided by missionary hospitals in Shikarpur and Quetta under the able guidance of the legendary doctor Sir Henry Holland and his two sons.
In the northern part of the country, including Afghanistan, most of the eye care services were provided by another great missionary doctor, Dr Novel Christy, who headed the eye care team at Taxilla.
After 1950, few new eye care units were opened in the public sector at Multan, Peshawar, Dacca and Hyderabad. Few eye care units were also added to the military hospitals.
However, 80% of the population had no access to organized eye care services.5
Birth of the ophthalmological society of Pakistan
In the early 1950s, Dr William John Holmes of Honolulu, Hawaii, along with some close ophthalmologist friends, started thinking of creating a regional ophthalmic organization covering the vast area of the Asia-Pacific region.4
He wrote letters to all the countries of the region, urging them to constitute national societies and join the newly conceived regional society as and when it was formed. He wrote a similar letter to a young Pakistani ophthalmologist, Dr Raja Mumtaz Quli Khan, on 10 July 1957. In response to this letter, Dr Mumtaz convened a meeting of 32 ophthalmologists of the country, inviting them to approve the formation and constitution of the Ophthalmologic Society of Pakistan (OSP).
Thus, on 19 December 1957, OSP was formed with General WA Burki as its first elected president and Dr Mumtaz as its first secretary general.5
On 11 November 1958 in Brussels, on the occasion of the 18th International Congress of Ophthalmology, the International Council of Ophthalmology (ICO) approved the formation of the Asia-Pacific Academy of Ophthalmology (APAO).6 In 1960, the inaugural meeting of the Academy took place in Manila. The then President of ICO, Sir Stewart Duke Elder, sent the following message:
‘I know of no greater stimulus for the progress of ophthalmology in the vast area, which the APAO represent than the institution of a body such as yours’.6
The seventh congress of APAO took place in Karachi in 1979. The President of the country inaugurated it. He spent a lot of time with the international delegates and took keen interest in the aims and objectives of the Academy. He made the following announcements during his inaugural speech.
-
1
All sight-saving instruments and equipments imported to Pakistan will be exempted from import duty.
-
2
The Government will support Pakistani ophthalmologists who attend and present scientific papers in international conferences.
-
3
The President announced an annual Presidential gold medal in the name of Professor Ramzan Ali Sayyed, who was awarded the Jose Rizal medal in the congress.
In the background of the profound interest of the President of Pakistan in eye health, a year later, WHO invited a temporary consultant, Dr Hugh Taylor, to assess the current eye health status in Pakistan. His report proved to be a wake-up call for the country's ophthalmologists and health-care administrators.
Materials and methods
Situation analysis
The Hugh Taylor report made the following observations:7
-
1
The estimated prevalence of blindness in the country is about 2%.
-
2
Cataract is the most common cause of blindness.
-
3
There is gross mismatch of human resource in the country.
-
4
A total of 45 out of 64 districts are without an ophthalmologist.
-
5
Most of the ophthalmologists are urban based, whereas most of the blindness occurs in rural areas.
Advocacy
The WHO document was used for political and professional advocacy. The then President of Pakistan, General Muhammad Zia ul Haq, who already had a soft corner for disabled people, was sensitized about the issue through strong advocacy.
He created a national eye camp committee through a presidential order as a short-term measure for this purpose. This committee soon evolved into a national committee for prevention of blindness. The Ministry of Health notified the maiden committee in 1985 and appointed the first group of national and provincial coordinators.7 Professor Saleh Memon was appointed as the first national coordinator for prevention of blindness.
Epidemiological and operational research
The first pakistan national blindness survey
With assistance from WHO, the national committee took its first major undertaking in 1987 and conducted a nation-wide blindness survey under the chairmanship of Professor Saleh Memon. To assist in this process, ‘Sight Savers International’ (SSI) was requested to support the training of a young ophthalmologist in community eye health at the International Centre for Eye Health (ICEH), London.
Laboratory testing of the concept of district comprehensive eye care services
The concept of district comprehensive eye care services (DCECS) was conceived as a result of a situation analysis conducted to identify barriers to the uptake of cataract surgery from the provider's perspective at the district level.
Thus, a new concept of a national programme based on DCECS was developed.
The concept was carefully tested in a laboratory, that is, in a mobile operation theatre, before piloting it at a district level.
Pilot testing of DCECS in Bannu 1996–1997
The concept of DECS was then piloted in a real district with a population of 0.7 million for 2 years. After an external evaluation, the team declared the pilot district project as highly successful, and recommended that the pilot may be extended to more districts.
Consolidation of the concept of DCECP and its extension to 10 districts
The committee then prepared a 10-priority-district project, including seven units of FATA, and submitted it to SSI UK and the European Union for support.8 This project was also externally evaluated and found to be very successful. This project clearly demonstrated a significant increase in uptake of services especially by females in rural Pakistan.
Partnership development and the first 5-year national plan for prevention of blindness
For financial and technical support, a consortium of important international non-government developmental organizations (INGDOs) was formed, which included the WHO, ICEH, London, SSI, CBMI, Fred Hollows Foundation of Australia (FHF), and a few others.9
In 1994, the author had the privilege of being appointed as the second chairman of the national committee.
Under the new chairmanship, the national committee developed the first 5-year national plan for prevention of blindness on the basis of the results of the first nation-wide blindness survey. Salient features of the plan are given later in the paper.
The second 5-year plan (1999–2004)
After the successful implementation of the first plan, the national committee prepared the next 5-year plan on the basis of the emerging new demands of the country and the new guidelines provided by Vision 2020 (V2020).10
In the background of V2020 guidelines, various task forces were created within the national committee to address V2020 priority diseases, such as cataract, trachoma, refractive errors, childhood blindness, diabetic retinopathy, and so on.
The second pakistan national blindness survey (2002–2003)
A national blindness and low-vision survey was planned and executed in 2002–2003 to measure the prevalence of blindness and low vision, and the impact of the national programme.
Results
Results of the first survey
The prevalence of blindness was confirmed at 1.78%.11
Cataract turned out to be the major cause of blindness.
Figures 1 and 2 show the national and provincial distribution of causes of blindness in Pakistan.
Conclusions of the Bannu evaluation report
-
The project has been successful in providing primary eye care to most sections of populations in an accessible and affordable manner.12 Although the project has not yet achieved all its targets, it is now making major contributions towards meeting the incidence of bilateral blindness. If all districts/agencies in the province could match this performance, the incidence of bilateral blindness could be met.
-
The project has been able to establish a referral system from primary to secondary and thereafter to a tertiary level, thus especially facilitating female patients to access these facilities. This system needs further rectifications.
-
The project has not yet been able to establish a proper ophthalmic health education system. This will require additional efforts on the part of the project staff and Pakistan Institute of Community Ophthalmology (PICO).
-
The resources available to the project have not been utilized to produce optimal performance, but the performance has still improved substantially since its start and is significantly better than in most eye care units within the government structure.
-
The removal of obstacles, such as inadequate infrastructure, equipment, and manpower, has been a major contributory factor in the improved performance of the eye unit.
-
This particular project is not directly replicable at present. However, lessons have been learnt that will be relevant in its future replications.
Conclusions of the 10-district evaluation report
-
The 10-district comprehensive eye care (CEC) programme has had great success in creating a practical platform for eye care service delivery at the district level.13 The 10 eye care teams are committed to a district-based approach using systematic outreach services; use of services by the population continues to grow.
-
This programme also provides a replicable and sustainable model for the development of district eye care plans within a government structure. Effective advocacy, by PICO in particular, has led to wide acceptance of and commitment to CEC at district, provincial, and federal levels.
-
The evaluation has concluded that to a very large extent CEC has been institutionalized at the district level within the government structure. After clear and detailed planning, direct project management (currently by PICO) should be handled by district CEC committees. Additional capacity building for district CEC committees will be important.
-
There is tremendous opportunity for CEC to be sustained at the district level, if the strategies outlined at the provincial level are shared and embedded. Provincial stakeholders such as PICO and donors need to support the established district and provincial administrative, and political structures within a single provincial coordination structure.
Achievements of the first 5-year plan
-
Budget for the prevention of blindness was approved by the Government.
-
Primary eye care was integrated into primary healthcare.
-
PICO was established.
-
Provincial PBL committees were constituted and provincial CEC cells established.
-
National low-vision initiative was taken.
-
DCECP was initiated.
Achievements of the second 5-year plan
-
Expansion and consolidation of the CEC programme took place.
-
National task forces were created on V2020 priority diseases such as cataract, refractive errors, diabetic retinopathy, glaucoma and, nutritional and childhood blindness.
-
Strategies for control of nutritional blindness were evolved. Vitamin A distribution was made part of the national immunization programme.
-
The national trachoma programme was initiated. The WHO SAFE strategy was used as the method for control of blinding trachoma.
-
The second national blindness survey was successfully conducted.
Results of the second national survey
All-age prevalence of blindness was estimated at 0.9% (5% CI 0.8–1%)14 and cataract was identified as the major cause of blindness (Figure 3).15
The outcomes of cataract surgery are explained in Figure 4.16
Results of the 10-district CEC programme
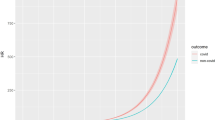
The impact of the district CEC programme on the access of eye care services, surgical output, and gender is explained in Figures 5, 6 and 7.
National eye care programme
-
Reduction in the prevalence of overall blindness by half, that is, from 1.78% in 1987 to 0.9% in 2003 (Figure 8).
-
Reduction in cataract as the cause of blindness from 80 to 51% (Figure 9).
-
Increase in the cataract surgical rate to 4000 per million population per year.
-
Increase in the number of IOL implantations since the year 2000.
-
Improvement in outcomes of cataract surgery with IOL.17
Future agenda, the third 5-year plan
-
Enhancing primary eye care by introducing the following:
-
The concept of community vision centres for refraction and low-vision services.
-
Public health education.
-
-
Improved referral system.
-
Rolling out the concept of DCECP to the remaining few districts.
-
Decentralization of eye care management to the district CEC committee.
-
Inclusion of YAG and argon laser services in the DCECP package.
-
Capacity building of tertiary care institutes and centres of excellence.
-
Introduction of subspeciality development at centres of excellence.
-
Enhancing the number and quality of members of eye care teams at all levels.
Discussion
To assess the true status of eye health in terms of prevalence, causes, and distribution, the national committee with the technical assistance of WHO conducted the first national survey on blindness in 1987–1989.
The beginning of an international collaboration
In 1988, the initial findings of the national survey and the features of a future comprehensive national eye care programme were discussed with the executive Director of SSI, Mr Alan John. He agreed to assist in the following manner.
-
1
Support the training of an ophthalmologist in community eye health at the ICEH, London.
-
2
Support testing the hypothesis of the proposed national CEC programme in a controlled environment to create evidence that the model is workable and replicable.
Dr Mohammad Aman Khan was selected for the course at ICEH, who returned after successfully completing the course.
The concept of a district eye care programme and the operational research to validate it
To test the hypothesis, we borrowed a mobile operating theatre from the Layton–Rahmatullah Benevolent Trust (LRBT) and parked it in front of the eye department at Lady Reading Hospital, Peshawar. The unit was equipped with all necessary surgical instruments, and equipments (courtesy: SSI).
We posted a nurse, an ophthalmic technician, and a young ophthalmologist there. The unit was allowed to function from 0800 to 1400 h, 6 days a week. The project was allowed to function for 2 years and was then externally evaluated by an SSI team.
The evaluation report confirmed that the unit was able to perform >1000 sight-restoration operations per year. It was therefore decided to test the model in a real pilot district.
Bannu district, which is located 160 miles southwest of Peshawar, was selected to be the pilot district. The district had a population of 0.5 million people served by two ophthalmologists posted in the district headquarter hospital. The annual output of the two ophthalmologists was 150 surgeries per year. A gap-analysis study showed that the poor performance of the two surgeons was because of lack of motivation, training, lack of support staff, lack of access to appropriate instruments, and equipments, and as well as lack of a dedicated operation theatre and indoor and outdoor facilities. These gaps were bridged by re-training and remotivation of ophthalmologists, by the provision of four paramedics, a computer, and a computer operator, and by the provision of dedicated indoor, outdoor, and operating room facilities. All essential instruments and equipments were provided by the SSI, UK.
The project was allowed to function for 2 years and was then evaluated by a team of external evaluators.
The evaluation report confirmed a significant increase in the outpatient attendance and surgical output. (See Figures 5 and 6)
The first 10-district programme
With strong evidence at hand, SSI decided that a 10-district project may be prepared for replication of the model. The 10 districts were selected strictly on the basis of their socioeconomic indicators. The districts included all seven FATA districts plus three settled districts (Table 1).
The project lasted for 5 years. However, a midterm review by a group of highly professional external evaluators demonstrated significant success. Apart from a general increase in the uptake of services, the group reported that the uptake by female patients exceeded that of male patients after the first 2 years of initiation of the project. (See Figure 7)
The midterm review report proved to be a turning point in Pakistan's national eye care programme. It affected the programme in two ways. (1) With such strong evidence at hand, the national committee moved confidently towards preparing a national programme on the basis of DCECS. (2) After the report was published, we started getting offers from small donors from all over the world for developing eye care districts.
We were thus set to plan for the first 5-year programme.
The formation of a consortium
A consortium consisting of federal government, provincial governments, and three major INGDOs, namely, the SSI of UK, the CBM of Germany, and the FHF of Australia, provided the necessary financial and technical resources. WHO and ICEH, London, continued to guide and support the national committee.
Few smaller donors such as Himalaya Eye Care, Light and dark foundation, Light for the world, and Rotary International also offered valuable support.
The 5-year programme: salient features, targets and achievements
-
To make PBL a national health priority.
-
To integrate PEC into PHC.
-
To determine and standardize the human resource and infrastructure needs.
-
To estimate the cataract surgical output.
-
To prepare a blueprint for national eye care services.
The first 5-year programme lasted from 1994 to 1999. Most of the targets in terms of training and re-training at all levels, physical infrastructure improvements and technology supply were adequately met.
The concept of a comprehensive programme was shared with global leaders in a major international meeting in Tokyo, Japan, in 1998.
The second 5-year programme: salient features, targets, and achievements
-
To adopt a WHO global initiative V2020 at the national level.
-
To extend DCECP to other districts on the basis of their infrastructure, human resource, and technology needs.
-
To establish seven centres of excellence with facilities for the following:
-
1
Human resource development (HRD).
-
2
Subspeciality services.
-
3
Production of low-cost eye drops.
-
4
Eye banks.
-
1
-
To conduct trachoma rapid assessment to implement SAFE control strategies.
-
To evaluate the impact of the national eye care programme by conducting a second nation-wide blindness survey.
The second 5-year plan followed and lasted till 2004.
Other important events
Three additional significant developments took place during these years that had a major impact on eye care in the country.
The establishment of the layton–rahmatullah benevolent trust
The trust was established in 1984 by Mr Graham Layton, a British Pakistani, and his friend Mr Rahmatullah with a humble sum of 1.0 million Pakistani rupees. The trust now runs a large national network of very high-quality free eye hospitals consisting of 2 tertiary hospitals, 17 secondary hospitals, and 41 primary eye care outlets. The trust has so far treated more than 17.0 million outpatients and performed more than 1.8 million sight-restoration operations. They are also involved in HRD and clinical research.
Al Shifa trust hospitals
In 1984, on the occasion of the Afro-Asian Congress of Ophthalmology at Lahore, the President of Pakistan ordered the establishment of an eye hospital in Pakistan with international standards, for which he donated military land in Rawalpindi.
Al Shifa now runs four autonomous centres of excellence, one in each province, all engaged in service, HRD, and research and development.
The pakistan institute of community ophthalmology, peshawar
In 1987, on the occasion of Haj, the author discussed with Dr Aman khan the possibility of enroling in a postgraduate study in community eye health. He was at that time serving as an ophthalmologist in Saudi Arabia. Dr Aman agreed to the suggestion. In 1988, during the annual conference of OCP, the matter was discussed with one of the invited guests, Mr Alan John, the executive Director of SSI, UK. He readily agreed to our request and Dr Aman went to ICEH and returned to Pakistan after graduation.
A small one-room cell of community eye health was created within the Department of Ophthalmology, Lady Reading hospital, Peshawar, from where Dr Aman initiated his work. When the workload increased and ICEH trained a few more experts in community eye health, courtesy SSI, UK, the cell began to grow and was soon given the status of Department of Community Eye Health.
In 1997, WHO, IAPB, ICEH, and the INGDOs decided to create a community eye health institute in the WHO EMR. After considering one or two alternate sites, the group, in a meeting of the Program Advisory committee (PAG) in New Delhi, decided to build the institute at Peshawar, Pakistan, where some infrastructure already existed. An MOU was signed17 between the Government of NWFP and two INDGOs, namely, the SSI and the CBM, to support the creation of such an institute.
PICO was inaugurated in 1999 in a major function presided over by the President of the country and dignitaries from WHO, relevant ministries, and INGDOs.
PICO with financial assistance from SSI, CBM, FHF, and technical assistance from ICEH started running a Master course in community eye health, and also designed a 1-year course for ophthalmic technicians and a 4-year degree course in vision sciences. It also became the national headquarters for prevention of blindness activities in Pakistan and Afghanistan.
College of Physicians and Surgeons of Pakistan
In the sixth decade of the last century, General WA Burki, an ophthalmologist with a vision, was working as Minister of Health, Government of Pakistan. In 1963, he created four major health institutions through an act of law. They were:
-
1
The College of Physicians and Surgeons, Pakistan (CPSP).
-
2
The Pakistan Medical and Dental Council.
-
3
The Jinnah Postgraduate Medical Center.
-
4
The Pakistan Medical Research Council.
CPSP was established on the lines of the Royal colleges of UK. It was initially training relatively a small number of fellows till 1980, when suddenly the western countries closed doors on trainees from developing countries. CPSP therefore had to get energized.
At present, apart from its headquarters at Karachi, it operates from 13 national regional centres and 3 overseas regional centres. It has 139 national and 96 overseas-accredited institutes. It has currently 2069 supervisors and 13 290 students. It offers fellowship in 57 specialities and Masters and Diplomas in 18 specialities. To date, 18 296 fellows and Diploma holders (10 970 fellows and 7324 Masters and Diploma holders) have passed out from this institute. Currently, over 90% of the specialist health-care delivery of the country is through the alumni of CPSP.
Pakistan Medical and Dental Council
The council is supposed to monitor the quality of medical education and maintain high standards of medical practice. It started with 78 doctors and two medical colleges. It is currently dealing with 64 medical colleges, 28 dental colleges, and 25 postgraduate medical institutes. It is also monitoring the work and conduct of 111 600 general doctors, 21 500 specialist doctors, 84 000 dentists, and 517 dental specialists.
Table 1 indicates the current ophthalmic health force.
The impact
In 2001, after working for 25 years, the national committee felt a strong need for a well-planned second national survey. Figures 10 and 11 The matter was discussed with the donors who agreed to support the survey. A joint survey protocol was developed and signed between PICO SSI, CBM, and FHF. The ethical committee of the Pakistan Medical Research Council approved this project. The survey began in 2001 and finished in 2004.
National impact
The national prevalence of blindness declined from 1.78 to 0.9%.
Impact on the policy
The national programme until 2004 was solely dependent on funds from INGDOs, with minimal input from the Government. The results from the second survey were presented to the Federal Minister of Health. For the first time in the history of the country, the Federal Minister of Health announced 2.87 billion Pakistan rupees (46 million USD) for the third prevention of blindness plan.
Vitamin A deficiency was recognized as an important cause of corneal blindness in children.18 Therefore, the vitamin A national distribution programme was dovetailed to the national immunization programme.
Trachoma
In the late 1990s, Pakistan was recognized as one of the countries having endemic blinding trachoma. It was therefore included in the list of 47 priority countries needing intervention. It thus became a member of the global elimination of trachoma programme (GET 2020). A lot of effort has gone into the control of this chronic and disabling eye aliment. The country has already fixed 2015 as the date for declaring the country free from blinding trachoma.
Impact on eastern mediterranean region
The national programmes of almost all the countries in the EMR region are based on the concept of DCECS.
It is expected that in the not too distant future all these countries will have equitable eye care services for their people.
To facilitate this process many young ophthalmologists from a number of countries in EMR have been trained in the Masters course of PICO.
Global impact
-
a)
A number of ophthalmologists in Africa, China, Indonesia, and Sri Lanka have gone through the Masters course of PICO, and are now the advocates of district eye care services in their respective countries.
-
b)
The Pakistan Programme has given V2020 a strong evidence-based replicable model for implementation in other developing countries.
References
Health Systems Profile - Pakistan. Regional Health Systems Observatory - EMRO: http://who.org.int. (downloaded 5 June 2010).
Fazila-Yacoobali V . The Long Partition and The Making of Modern South Asia. Zamindar: Columbia, 1893.
National Health Policy 2010: towards a healthy Pakistan: Ministry of Health Government of Pakistan.
Aziz S . Economic Survey 1990–1991. Government of Pakistan, Finance Division, Economic Adviser's Wing: Islamabad, 1991.
Archives of Ophthalmological Society of Pakistan at its Golden Jubilee: at the occasion of the Second Congress of APAO in Pakistan, 24–28 February. 2007.
Lim ASM, Singh P, Selvarajah DS . Transactions of the Asia Pacific Academy of Opthalmology. XI Vol., PG Publishing Pte Ltd: Singapore 1998.
The Hugh Taylor Report WHO. 1980.
EU Proposal. North West Frontier Province/Federally Administered Tribal Areas: Comprehensive Eye Care Programme: 1999–2004.
National Program for Prevention of Blindness. 1st Five Year Plan: 1994–1998. Ministry of Health, Special Education and Social Welfare: Islamabad.
National Program for Prevention of Blindness. 2nd Five Year Plan: 1999–2003. Ministry of Health, Special Education and Social Welfare: Islamabad.
Memon S . Pakistan National Blindness Survey. J Pak Med Assoc 1992; 196–198.
PICO & Sight Savers International. Mid-term Review of the Bannu Comprehensive Eye Care Project North West Frontier Province Pakistan, November 1997.
Courtright P, Van Berkel W, Banzi J, Khan UN, Jan N . Final Evaluation PICO. 10 District Comprehensive Eye Care Program. NWFP and FATA: Pakistan, 2004.
Jadoon MZ, Dineen B, Bourne RR, Shah SP, Khan MA, Johnson GJ et al. Pakistan: prevalence of blindness in Pakistan adults: the Pakistan National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci 2006; 47 (11): 4749–4755.
Dineen B, Bourne R, Jadoon Z, Shah SP . Causes of blindness and visual impairment Pakistan. The Pakistan National Blindness and Low Vision Survey, January 2007 10.1136/bjo.2006.108035.
Bourne R, Dineen B, Jadoon Z, Lee PS, Khan A, Johnson GJ et al. Visual outcomes of cataract surgery in Pakistan: results from Pakistan national blindness and visual impairment survey. Br J Ophthalmol 2007; 91 (4): 420–426.
Jadoon Z, Shah SP, Bourne R, Dineen B, Khan MA, Gilbert CE et al. Cataract prevalence, cataract surgical coverage and barriers to uptake of cataract surgical services in Pakistan: the Pakistan national blindness and visual impairment survey. Br J Ophthalmol 2007; 91: 1269–1273.
Khan MA, Khan MD . Classification of 154 clinical cases of vitamin A deficiency in children (0–15 years) in a tertiary hospital in North West Frontier Province Pakistan. J Pak Med Assoc 2005; 55 (2): 77–78.
Acknowledgements
I gratefully acknowledge the support of the following: Federal and Provincial Ministries and Directorates of Health, District Health authorities, WHO country, regional, and international offices, and Internal Center for Eye Health London; INGDOs: Sight Savers International, CBMI, Fred Hollows Foundation, Eye Care Foundation, Light and Dark Foundation, Light for the World, International Eye Foundation USA, Wild Geese Netherlands, Rotary International, Al-Basar Foundation, AusAID, and European Union; International institutes: Jutendo University Japan, and University of Pretoria, South Africa; National NGOs: Layton–Rahmatullah Benevolent Trust, Al Shifa Trust, and Khyber Eye Foundation; National institutes: College of Physicians & Surgeons Pakistan, Hayatabad Medical Complex Peshawar, Pakistan Institute of Community Ophthalmology, College of Ophthalmology and Allied Vision Sciences, Sindh Institute of Community Ophthalmology, Balochistan, Comprehensive Eye Care Cell, and Al-Ibrahim Eye Hospital; and members of national and provincial committees. The following individuals made significant contributions: Dr Para Rajasegaram, Professor Saleh Memon, Dr Aman Khan, Dr Harron Awan, Dr Rubina Guillani, Dr Mohammad Babar Qureshie, Dr Zahid Jadoon, Professor Ziauddin Sheikh, Professor Nasim Panezai, Professor Shad Mohammad, and Professor Asad Aslam Khan. I offer special thanks to Mr Basharat Waris of CHEF International for typing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Khan, M. The Duke Elder Lecture: The challenge of equitable eye care in Pakistan. Eye 25, 415–424 (2011). https://doi.org/10.1038/eye.2010.186
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.186