Abstract
Purpose
To investigate the possible roles of retinal photoreceptors in macular oedema and retinal angiogenesis with particular reference to the mode of action of laser therapy.
Methods
(i) Studies in rats made hypoxic for 2 h by administering an oxygen/nitrogen mixture of reduced oxygen content, and growth factors determined by RT-PCR, western blotting, and immunohistochemistry. Assessment of blood–retinal barrier integrity using fluorescent and electron-dense tracers. (ii) Studies in pigs with one retina made hypoxic by selective embolisation of the retinal capillary circulation with fluorescent microspheres. (iii) Assessment of laser therapy in selected cases of retinal neovascularisation indicating a role for photoreceptors.
Results
In the hypoxic retina, angiogenic and vascular permeability factors such as vascular endothelial growth factor (VEGF), nitric oxide synthases (NOSs), and insulin-like growth factor-1 are upregulated in retinal astrocytes and Müller cells but are also present in large amount in the photoreceptors. Hypoxia-inducible factor-1 (HIF-1) is upregulated in retinal glial cells but not in the photoreceptors, suggesting that growth factors in the photoreceptors may not have been generated there. The tracer dye, rhodium isothiocyanate, leaking from an abnormally permeable inner blood–retinal barrier in the hypoxic retina accumulates in the photoreceptors.
Conclusions
The results indicate that laser treatment of macular oedema or retinal neovascularisation may obtain its effect not only by improving oxygen availability in the inner retina, but also by reducing the load of angiogenic/permeability factors that accumulate in the photoreceptors in hypoxic/ischaemic conditions.
Similar content being viewed by others
Introduction
It is well recognised that retinal hypoxia has a major role in the genesis of intraocular neovascularisation, such as occurs in proliferative diabetic retinopathy and after ischaemic retinal vein occlusion.1, 2, 3, 4 There is also evidence that hypoxia has a role in some forms of retinal oedema, including diabetic macular oedema, which is the commonest cause of visual loss in individuals suffering from type II diabetes.5 It is well recognised that vascular endothelial growth factor (VEGF) is upregulated in the retina in response to hypoxia, and the fact that anti-VEGF therapy has also been shown to have a beneficial effect in reducing retinal thickness in a number of conditions in which macular oedema is a feature6, 7, 8 is evidence that hypoxia has a significant role in the aetiology of hypoxia-induced macular oedema in addition to its undoubted role in angiogenesis.
The aetiological roles of retinal hypoxia in angiogenesis and in the breakdown of the inner blood–retinal barrier that leads to macular oedema operate through the upregulation of hypoxia-inducible factor-1 (HIF-1), which in turn leads to an upregulation of VEGF and NOSs, the latter leading to an increase in retinal nitric oxide (NO) levels.9, 10, 11, 12
Both VEGF and NO are angiogenic13 and cause vasodilatation and increased vascular permeability leading to extracellular oedema. Indeed, VEGF has also been known as a vascular permeability factor.14 We have investigated the effects of hypoxia on the rat retina and of inner retinal hypoxia on the pig retina, and now relate some of our cellular and molecular findings to clinical conditions in which hypoxia is thought to have a role and which suggest additional reasons, to those currently accepted, for the efficacy of laser treatment in the management of intraocular new vessel formation and of some forms of macular oedema.
It is accepted on the basis of clinical experience and the results of randomised trials that laser panretinal photocoagulation is an effective treatment for proliferative diabetic retinopathy15, 16, 17 and that laser treatment is of benefit in controlling the neovascularisation that characterises the retinopathy of prematurity18, 19 and ischaemic branch retinal vein occlusion.20, 21
In spite of the fact that laser panretinal photocoagulation for diabetic retinopathy has been used since it was first suggested by Meyer-Schwickerath almost 50 years ago,22 and that grid laser treatment in the management of macular oedema has been used for some 40 years,23 some aspects of the mode of action of laser in these and similar conditions remain incompletely explained. Thus, although it has been established both experimentally24, 25, 26, 27 and clinically28, 29, 30, 31 that laser treatment results in an increase in oxygen availability in the inner retina, explanations for this finding have varied between an increased inward diffusion of oxygen from the choroid through laser-disrupted tight junctions in the retinal pigment epithelium (RPE),32 and a reduced oxygen demand in the outer retina (and a consequent increased availability of oxygen in the inner retina) resulting from laser destruction of highly energy-demanding photoreceptors26, 33 or from destruction of other retinal neural elements,34 or from a combination of these factors, including diffusion of oxygen from the anterior chamber in eyes undergoing concomitant vitrectomy and laser treatment.35
Originally it was suggested that laser panretinal photocoagulation obtained its effect from destruction of ischaemic retina, but in diabetes and after ischaemic retinal vein occlusion, retinal capillary closure leading to retinal ischaemia and hypoxia affects the inner retina while laser is preferentially absorbed, and produces its effects in the RPE and outer retina.
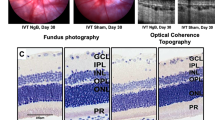
Even gentle laser restricted to the RPE and photoreceptors (Figure 1a) can be effective in controlling neovascularisation.36 Gentle laser can cause regression of optic disc new vessels in as short as 3 days (Figure 1b), which is too short a period for trans-neuronal degeneration to affect the inner retina.
In an illustrative case it appears that gentle laser can cause regression of new vessels even when applied to an area of the retina in which the inner retina is functionally ‘dead’. The case in question was a man who suffered an upper hemiretinal vein occlusion that led to optic nerve head neovascularisation. This was treated before his referral to one of the authors by heavy xenon photocoagulation applied immediately above the optic disc, which had the effect of closing most of the vascular blood supply to the upper retina with an absolute loss of the lower half of the visual field, however, without beneficially affecting the new vessels that were present (Figure 2a).
An illustrative case. (a) Fundus photographs and fluorescein angiograms showing new vessels on the optic disc (OD) after treatment of an upper hemiretinal vein occlusion with heavy xenon photocoagulation above the OD that closed most of the upper retinal blood supply with total loss of the inferior visual field. (b) Resolution of new vessels after the application of gentle laser to the non-functional upper retina.
Gentle scatter laser applied to the upper non-functional retina resulted in a rapid disappearance of the optic disc new vessels (Figure 2b).
In this case, although the inner retina was functionally ‘dead’, the outer retina would have remained functional. It is probable that the inner retina still received some perfusion that was inadequate to maintain the functionality of the retinal ganglion cells but was sufficient to maintain the integrity of the retinal glial cells, which have lower energy demands than neuronal cells. Retinal Müller cells are relatively resistant to hypoxia and are a major source of VEGF and other angiogenic factors in hypoxic retina.37, 38 VEGF elaborated in hypoxic Müller cells was the probable cause of the optic disc neovascularisation in this case.
Gentle laser applied to the apparently non-functional upper retina would have been unlikely to have affected the Müller cells directly, and the only tissues directly affected by the laser would have been the RPE and photoreceptors. As the retinal ganglion cells in the upper affected area of retina were nonfunctional, it is unlikely that the disappearance of optic disc new vessels in this case was effected by an increased availability of oxygen in the inner retina.
The mode of action of grid laser photocoagulation as a therapeutic strategy for diabetic and other forms of macular oedema in which hypoxia has a role remains even less explained.
From our studies on the effects of retinal hypoxia in experimental animals,12, 39, 40, 41, 42 we believe that we have found an additional explanation for the beneficial effects of both laser panretinal photocoagulation for neovascularisation and grid laser treatment for macular oedema.
Methods
Firstly, the experimental animals used (adult rats of 200 g body weight) were made hypoxic by breathing a 7% oxygen/93% nitrogen mixture for 2 h and were followed up subsequently for periods up to 2 weeks. In summary, 108 rats made hypoxic for 2 h were followed up in normoxic conditions for 3 h, 24 h, or 3 , 7, or 14 days before killing. Twenty-five non-hypoxic rats were used as controls. Another 25 rats received an intraperitoneal injection of melatonin in normal saline (10 mg/kg body weight) immediately before and immediately after hypoxic exposure, and again 1 h later, and were followed up for 3 h, 24 h, 3 days, or 7 days. At these time intervals, the effect of hypoxia on retinal growth factors, inflammatory cytokines, and other factors was investigated in all animals by RT-PCR, western blotting, and immunohistochemistry, and also by light and electron microscopy. Retinal VEGF levels were also investigated, as previously described,12 using a Chemikine VEGF EIA kit (Chemicon International Inc., Temeccula, CA, USA), and NO levels by determining the retinal nitrite levels by the Griess reaction.
Secondly inner retinal ischaemia was induced in pigs by embolisation of retinal capillaries with fluorescent microspheres of 10 or 15-μm diameter (Fluospheres, Molecular Probes, Eugene, OR, USA). The microspheres were delivered to the origin of the external ophthalmic artery that supplies blood to the eye in this species.
A custom-built cannula of 2.5 mm external diameter was introduced into one common carotid artery and advanced past the origin of the internal carotid artery into the external carotid and maxillary arteries, the latter of which gives origin to the external ophthalmic artery in this species.
In this way the microspheres were delivered to the eye and not to the central nervous system. The microspheres were of a size sufficient to block retinal but not choroidal capillaries (Foulds WS et al, unpublished). Closure of inner retinal capillaries, thus restricting ischaemia to the inner retina, reproduces some of the features of retinal capillary closure, which is a characteristic of advanced diabetic eye disease.
We certify that in relation to the animal research undertaken, all applicable institutional and governmental regulations regarding the ethical use of animals were followed during this research.
Results
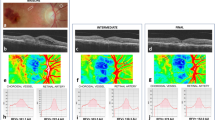
We have reported that in the hypoxic adult rat retina there is an upregulation of HIF-1α,12 VEGF,12 NOSs,12 insulin-like growth factors,39 angiopoetin-2,39 glial fibrillary acidic protein (GFAP),40 and aquaporin-4,40 and a downregulation of pigment epithelial-derived factor.39 In the rat model, VEGF and inducible nitric oxide synthase (iNOS), which are absent from the photoreceptor layer in the retina of control eyes, are markedly present in the photoreceptor layer in the post-hypoxic rat retina, and it appears that factors such as iNOS actually concentrate in the photoreceptors (and possibly in their outer segments, although there is some diffusion into the surrounding interphotoreceptor matrix). The photoreceptor cell bodies do not show evidence of iNOS (Figures 3a–d).
Immunohistochemistry to show VEGF in control (a) and post-hypoxic (b) adult rat retinas. VEGF is not present in the photoreceptor layer of control eyes (blue arrow) (a), but is upregulated in astrocytes and Müller cells in the hypoxic eye (small white arrows) and is markedly concentrated in the photoreceptor layer (red arrow). Immunohistochemistry to show inducible nitric oxide synthase (iNOS) in control retina (c) and hypoxic retina (d). Inducible nitric oxide synthase is not present in the photoreceptors of control eyes, but is markedly present in the photoreceptors in the hypoxic retina (red arrow), where it appears to be concentrated in the photoreceptor outer segments (e—inset at higher magnification). Fluorescein angiogram (f) of a pig retina embolised with fluorescent microspheres showing diffuse leakage of fluorescein from the embolised capillaries. Immunohistochemistry to show the distribution of VEGF in hypoxic embolised pig retina (g). In the embolised eye VEGF is present in the astrocytes and Müller cells (white arrows) and in the photoreceptors (red arrow).
In the embolised pig retina there was increased retinal vascular permeability with diffuse fluorescein leakage at 3 weeks after embolisation (Figure 3e) and a significant increase in retinal thickness. VEGF, which is not present in the photoreceptors of control eyes, was markedly present in the photoreceptors of the embolised retina (Figure 3f).
The integrity of the blood–retinal barriers in the hypoxic rat retina was investigated using of the fluorescent dye tracer rhodium isothiocyanate (RhIC) and the electron-dense horseradish peroxidase (HRP) product. The results and methodology are fully described elsewhere.40 In summary, three post-hypoxic rats, three control rats, and three hypoxic rats also injected with melatonin intraperitoneally (as described above), were given RhIC (5 μl 1% RhiC/g body weight) by intraperitoneal injection at 24 h after hypoxic exposure. Six hypoxic rats and six control animals were given an intravenous injection of HRP (0.5 μl/g body weight) at 24 h after hypoxic exposure.
Animals given RhIC were killed 6 h after tracer administration and were studied by double immunofluorescence (RhIC and GFAP). Animals given HRP were killed 3 or 24 h after and were studied by electron microscopy.
It was found that although there was no leakage of either tracer in any of the control eyes, in the post-hypoxic rat retina both tracers leaked copiously from a breakdown in the inner blood–retinal barrier.
Electron microscopy showed that the RPE tight junctions remained intact and there was no leakage of HRP across the posterior blood ocular barrier.40
In the post-hypoxic rat retina, the tracer RhIC not only leaked copiously from the damaged inner blood–retinal barrier, but also appeared to accumulate in Müller cells and in the photoreceptors (Figure 4). As the RhIC was derived from the blood circulating in the capillaries in the inner retina through an inner BRB of increased permeability and not generated within the retina, the fact that this tracer accumulated in the photoreceptors suggested a predilection for the absorption and accumulation of this dye tracer in the photoreceptors.
Control and hypoxic rat retina showing leakage of the red tracer dye RhIC from the hypoxia-damaged inner blood–retinal barrier. The leaking dye has accumulated in the Müller cells (*) and markedly in the photoreceptors (yellow arrow). None of the control eyes showed dye leakage (INL, inner nuclear layer; ONL, outer nuclear layer).
As an upregulation of VEGF in the hypoxic rat retina or embolised pig retina is a consequence of upregulated HIF-1, the distribution of HIF-1 in the embolised retina would be expected to be similar to that of VEGF. However, immunohistochemistry of the embolised pig retina showed that although HIF-1 is upregulated in the astrocytes and Müller cells of the embolised pig retina, it is not detectable in the photoreceptor layer in either control or embolised eyes (Figure 5). This suggests that VEGF in the photoreceptors may not have been elaborated there but had accumulated from elsewhere in the retina.
Immunohistochemistry of HIF-1 in control and embolised pig retina. HIF-1 is upregulated in the astrocytes and Müller cells of the embolised retina (inset at higher magnification), but is not detectable in the control eye. HIF-1 is not present in the photoreceptors of either the control or embolised eyes (arrowed).
Discussion
The findings suggest that the photoreceptors may act as a repository for molecules elaborated in the inner and mid-retina that have diffused outward across the retina, and that the resulting high concentration of growth factors in the photoreceptors in hypoxic conditions may form a reservoir from which their angiogenic and vascular permeability effects might proceed.
Analysis of published data on how much laser treatment is required to control neovascularisation in conditions such as proliferative diabetic retinopathy15, 36 indicates that it is the area lasered that is important rather than the intensity, a larger area of gentle laser being more effective than a smaller area of intense laser. As even gentle laser destroys photoreceptors, this is additional evidence that photoreceptor destruction is the key to its effectiveness in the treatment of neovascular retinopathies and of macular oedema.
As already indicated, it has been shown that that laser photocoagulation results in an increase in oxygen availability in the inner retina and in the pre-retinal vitreous.
Diffusion of oxygen into the retina from the inner blood vascular system or from the choroid is governed by the relevant concentration gradients of oxygen across the retina, although the heterogeneity of oxygen distribution across the inner retina makes application of simple models of diffusion difficult.43 Oxygen levels in the inner retina are higher near arterioles,25 and in the absence of a choroid, there would be an oxygen concentration gradient favouring oxygen diffusion towards the outer retina across the whole retina. Similarly, it has been shown that in eyes without an inner retinal circulation oxygen diffuses inwards from the choroid across the whole retina in amounts sufficient to meet the metabolic requirements of the normal inner retina.44
In eyes with a dual blood supply but in which the inner retinal circulation is deficient, the supply of oxygen to the inner retina from the choroid is not sufficient to overcome the inner retinal hypoxia.45
In relation to oxygen distribution in the retina, experiments have shown that in eyes with a dual blood supply the inner and outer retina behave as two separate domains.46 In such eyes there are two oxygen concentration gradients, one decreasing from the inner to mid-retina and the other decreasing from the outer to mid-retina, each reaching a similarly reduced concentration at around this level, and in normal circumstances, no further inward or outward diffusion of oxygen from this locus.
The actual availability of oxygen at any particular locus in the retina is determined not only by the diffusion pattern of oxygen but also by the uptake of oxygen by cells using oxygen for their metabolic requirements.
Thus, the concentration of oxygen is high in the outer retina, close to the choriocapillaris, but falls dramatically at the level of the photoreceptor inner segments that have the highest energy requirements in the retina.47 This reduction of available oxygen at the level of the photoreceptor inner segments is most marked during darkness, when the rod metabolism is at its highest.47, 48, 49
In conditions in which inner retinal hypoxia has a role in pathophysiology, such as in diabetes, there is a reduced availability of oxygen in the inner retina but a normal availability in the outer retina. The resulting altered concentration gradient would favour increased diffusion of oxygen from the outer to inner retina, but as has been shown experimentally, in normoxic conditions, this would be insufficient to overcome the hypoxia affecting the inner retina.45
The increased availability of oxygen in the inner retina that follows laser treatment has given rise to a number of separate possible explanations. Thus it has been suggested26, 33 that laser panretinal photocoagulation may obtain its effect from the reduced oxygen demand resulting from photoreceptor destruction with a consequent improvement in retinal oxygenation. Destruction of photoreceptors with their high oxygen demand would increase the concentration of oxygen in the retina at the level of the photoreceptor inner segments and alter the concentration gradient of oxygen towards an increased diffusion of oxygen to the previously hypoxic inner retina.
An alternative explanation that has been suggested is that, as laser treatment disrupts RPE tight junctions, this might allow an increased inward diffusion of oxygen to the retina through laser scars.32 However, there is evidence that junctional complexes including tight junctions form between cells within such laser scars,50 and also that the barrier function of the RPE is rapidly restored after photocoagulation burns.51, 52
An early suggestion was that grid laser might increase outward water movement from the retina to the choroid through a damaged and scarred RPE,53 but experimental determination of the rate of water movement across the photocoagulated retina to the choroid in rabbits indicated that laser treatment reduced the rate of outward water movement to the choroid rather than increasing it.54 The fact that the outward movement of small molecules from the retina to the choroid was reduced following scatter photocoagulation might suggest that inward diffusion of oxygen might be similarly reduced by laser.
In addition, as laser can be effective in causing regression of new vessels even when applied to retina in which the oxygen demand has already been diminished by loss of functional retinal ganglion cells, as in the case already cited, this suggests that another or an additional explanation may be operative.
If, as it appears, angiogenic and vascular permeability factors concentrate in the photoreceptors in the hypoxic retina, laser treatment may obtain its beneficial effect in both intraocular neovascularisation and in the reduction of macular oedema that follows grid laser treatment, not only from an increased availability of oxygen in the inner retina (most probably as a result of reduced consumption of oxygen by the reduced number of photoreceptor inner segments) but also by a reduction in the load of angiogenic and permeability factors accumulating in the photoreceptors that would also follow laser-induced photoreceptor destruction.
Laser treatment is of necessity destructive, and a more rational approach to the treatment of intraocular neovascularisation or macular oedema would be the development of medical means of reducing the angiogenic and vascular permeability load in the photoreceptors. In this regard, it is of interest that melatonin administration in the post-hypoxic rat reduced VEGF in the retina to levels comparable to those in normal control animals and completely prevented hypoxia-induced inner retinal blood–retinal barrier breakdown,40 a finding that may point a way towards a less-destructive approach to the problems of neovascularisation and macular oedema.
References
Patz A . Clinical and experimental studies on retinal neovascularisation. XXXIX Edward Jackson Memorial Lecture. Am J Ophthalmol 1983; 94: 715–743.
Pe'er J, Shweiki D, Itin A, Hemo I, Gnessin H, Keshet E . Hypoxia–induced expression of vascular endothelial growth factor by retinal cells is a common factor in neovascularizing ocular diseases. Lab Invest 1995; 72: 638–645.
Joussen AM, Fauser S, Krohne TU, Lemmen KD, Lang GE, Kirchof B . Diabetic retinopathy: pathophysiology and therapy of hypoxia-induced inflammation. Ophthalmologe 2003; 100: 363–370.
Pournaras CJ, Tsacopoulos M, Strommer K, Gilodi N, Leuenberger PM . Experimental retinal branch retinal vein occlusion in miniature pigs induces local tissue hypoxia and vasoproliferative microangiopathy. Ophthalmology 1990; 97: 1321–1328.
Early Treatment of Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. ETDRS Report No. 1 Arch Ophthalmol 1985; 103: 1677–1682.
Schaal KB, Hoh AE, Scheuerle A, Schutt F, Dithmar S . Bevacizumab for the treatment of macular edema secondary to retinal vein occlusion. Ophthalmologe 2007; 104: 285–2897.
Scott IU, Edwards AR, Beck RW, Bressler NM, Chan CK, Elman MJ et al. Diabetic Retinopathy Clinical Research Network, A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmology 2007; 114: 1860–1867.
Campochiaro PA, Hafiz G, Shah SM, Nguyen QD, Ying H, Do DV et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther 2008; 16: 791–799.
Semenza GL . Expression of hypoxia-inducible factor 1: mechanisms and consequences. Biochem Pharmacol 2000; 59: 47–53.
Josko J, Mazurek M . Transcription factors having impact on vascular endothelial growth factor (VEGF) gene expression in angiogenesis. Med Sci Monit 2004; 10: RA89–RA98.
Wilkinson-Berka JL . Vasoactive factors and diabetic retinopathy: vascular endothelial growth factor, cyclooxygenase-2 and nitric oxide. Curr Pharm Des 2004; 10: 3331–3348.
Kaur C, Sivakumar V, Foulds WS . Early response of neurons and glial cells to hypoxia in the retina. Invest Ophthalmol Vis Sci 2006; 47: 1126–1141.
Dobrogowska DH, Lossinsky AS, Tarnawski M, Vorbrodt AW . Increased blood-brain barrier permeability and endothelial abnormalities induced by vascular endothelial growth factor. J Neurocytol 1988; 27: 163–173.
Croll SD, Ransohoff RM, Cai N, Zhang Q, Martin FJ, Wei T et al. VEGF-mediated inflammation precedes angiogenesis in adult brain. Exp Neurol 2004; 187: 388–402.
Diabetic Retinopathy Study Group. Photocoagulation treatment of proliferative diabetic retinopathy: relationship of adverse treatment effects to retinopathy severity. Diabetic Retinopathy Study Report No. 5 Dev Ophthalmol 1981; 2: 248–261.
Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings. DRS Report Number 8 Ophthalmology 1981; 88: 583–600.
Early Treatment Diabetic Retinopathy Study Group. ETDRS Report number 9 Early photocoagulation for diabetic retinopathy. Ophthalmology 1991; 98: 766–785.
Opsina LH, Lyons CJ, Matsuba C, Jan J, McCormick AQ . Argon laser for retinopathy of prematurity: long-term outcome. Eye 2005; 18: 1213–1218.
Kieselbach GF, Rambarter A, Baldissera I, Kralinger MT . Laser photocoagulation for retinopathy of prematurity: structural and functional outcome. Acta Ophthalmol Scand 2006; 84: 21–26.
Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for the prevention of neovascularisation and vitreous hemorrhage in branch vein occlusion. Arch Ophthalmol 1986; 104: 34–41.
Hayreh SS, Rubinstein L, Podhajsky P . Argon scatter photocoagulation in the treatment of branch retinal vein occlusion. A prospective clinical trial. Ophthalmologica 1993; 206: 1–14.
Meyer-Schwickerath G . Light coagulation, (Translated by Drance). Mosby: St Louis, 1960, p 114.
Dobree JH . Simple diabetic retinopathy. Evolution of lesions and therapeutic considerations. Br J Ophthalmol 1970; 54: 1–10.
Pournaras CJ, Tsacopoulos M, Strommer K, Gilodi N, Leuenberger PM . Scatter photocoagulation restores tissue hypoxia in experimental vasoproliferative microangiopathy in miniature pigs. Ophthalmology 1990; 97: 1329–1333.
Molner I, Poitry S, Tsacopoulos M, Gilodi N, Leuenberger PM . Effect of laser photocoagulation on oxygenation of the retina in miniature pigs. Invest Opththalmol Vis Sci 1985; 26: 1410–1414.
Stefánsson E, Hatchell DL, Fisher BL, Sutherland FS, Machemer R . Panretinal photocoagulation and retinal oxygenation in normal and diabetic cats. Am J Ophthalmol 1986; 101: 657–664, (PR Dest).
Budzynski E, Smith JH, Bryar P, Birol G, Linsenmeier RA . Effects of photocoagulation on intraretinal PO2 in the cat. Invest Ophthalmol Vis Sci 2008; 49: 380–389.
Stefánsson E, Machemer R, de Juan Jr E, McCuen 2nd BW, Peterson J . Retinal oxygenation and laser treatment in patients with diabetic retinopathy. Am J Ophthalmol 1992; 113: 36–38, (clin).
Funatsu H, Wilson CA, Berkowitz BA, Sonkin PL . A comparative study of the effects of argon and diode laser photocoagulation on retinal oxygenation. Graefes Arch Clin Exp Ophthalmol 1997; 235: 168–175.
Stefánsson E . The therapeutic effects of retinal laser treatment and vitrectomy. A theory based on oxygen and vascular physiology. Acta Ophthalmol Scand 2001; 79: 435–440.
Gottfredsdóttir MS, Stefánsson E, Jónasson F, Gíslason I . Retinal vasoconstriction after laser treatment for diabetic macular edema. Am J Ophthalmol 1993; 115: 64–67.
Stefánsson E . Oxygen and diabetic eye disease. Graefes Arch Clin Ophthalmol 1990; 228: 120–123.
Landers 3rd MB, Stefansson E, Wolbarsht ML . Panretinal photocoagulation and retinal oxygenation. Retina 1982; 2: 167–175.
Grunwald JE, Riva CE, Brucker AJ, Sinclair SH, Petrig BL . Effect of panretinal photocoagulation on retinal blood flow in proliferative diabetic retinopathy. Ophthalmology 1986; 93: 590–595.
Stefánsson E, Landers 3rd MB, Wolbarsht ML . Increased retinal oxygen supply following pan-retinal photocoagulation and vitrectomy. Trans Am Ophthalmol Soc 1981; 79: 307–334.
Luttrull JK, Musch DC, Spink CA . Subthreshold diode micropulse panretinal photocoagulation for diabetic retinopathy. Eye 2008; 22: 607–612.
Behzadian MA, Wang XL, Al-Shabrawey M, Caldwell RB . Effects of hypoxia on glial cell expression of angiogenesis-regulating factors VEGF and TGFbeta. Glia 1998; 24: 216–225.
Eichler W, Yafai Y, Wiedemann P, Reichenbach A . Angiogenesis-related factors derived from retinal glial (Müller) cells in hypoxia. Neuroreport 2004; 15: 1633–1637.
Zhang Y, Sivakumar V, Ling E-A, Foulds WS, Kaur C . Insulin-like growth factors, angiopoetin-2, and pigment epithelium derived growth factor in hypoxic retina. J Neuroscience Res 2008; 86: 702–711.
Kaur C, Sivakumar V, Yong Z, Foulds WS, Ling EA . Blood-retinal barrier disruption and ultrastructural changes in the hypoxic retina of adult rats: the beneficial effect of melatonin administration. J Pathol 2008; 212: 429–439.
Kaur C, Foulds WS, Ling EA . Hypoxia-ischemia and retinal ganglion cell damage. Clin Ophthalmol 2008; 2: 879–889.
Kaur C, Foulds WS, Ling EA . Blood-retinal barrier in hypoxic ischaemic conditions: basic concepts, clinical features and management. Prog Ret Eye Res 2008; 27: 622–647.
Linsenmeier RA, Braun RD . Oxygen distribution and consumption in the cat retina in normoxia and hypoxemia. J Gen Physiol 1992; 99: 177–197.
Cringle SJ, Yu DY, Alder V, Su EN . Light and choroidal PO2 modulation of intraretinal oxygen levels in an avascular retina. Invest Ophthalmol Vis Sci 1999; 40: 2307–2313.
Yu DY, Cringle SJ, Yu PK, Su EN . Intraretinal oxygen distribution and consumption during retinal artery occlusion and graded hyperoxic ventilation in the rat. Invest Ophthalmol Vis Sci 2007; 48: 2290–229647.
Wangsa-Wirawan ND, Linsenmeier RA . Retinal oxygen: fundamental and clinical aspects. Arch Ophthalmol 2003; 121: 547–557.
Braun RD, Linsenmeier RA, Goldstick TK . Oxygen consumption in the inner and outer retina of the cat. Invest Ophthalmol Vis Sci 1995; 36: 542–554.
Cringle SJ, Yu DY, Yu PK, Su EN . Intraretinal oxygen consumption in the rat in vivo. Invest Ophthalmol Vis Sci 2002; 43: 1922–1927.
Birol G, Wang S, Budzynski E, Wangsa-Wirawan ND, Linsenmeier RA . Oxygen distribution and consumption in the macaque retina. Am J Physiol Heart Circ Physiol 2007; 293: H1696–H1704.
Johnson NF, McNaught EI, Foulds WS . Effect of photocoagulation on the barrier function of the pigment epithelium. II A study by electron microscopy. Trans Ophthal Soc UK 1977; 97: 640–651.
McNaught EI, Foulds WS, Johnson NF . The permeability of the posterior blood ocular barrier after xenon photocoagulation: a study using fluorescein labelled dextrans. Br J Ophthalmol 1981; 65: 473–477.
Inoue M, Tsukahara Y, Shirabe H, Yamamoto M . Disruption of the blood-aqueous barrier following retinal laser photocoagulation and cryopexy in pigmented rabbits. Ophthalmic Res 2001; 33: 37–41.
Foulds WS . The clinical significance of trans-scleral fluid transfer. Trans Ophthal Soc UK 1976; 96: 290–308.
Foulds WS, Moseley H, Eadie A, McNaught E . Vitreal, retinal and pigment epithelial contributions to the posterior blood ocular barrier. Trans Ophthal Soc UK 1980; 100: 341–342.
Acknowledgements
We are grateful to Dr Viswanathan Sivakumar for his help with the rat immunohistochemistry and to Ms Song In Chin for her help with the pig surgery.
Research funding was provided by the Singapore Biomedical Research Council Research Grant 05/1/35/19/422 and the National University of Singapore Research Grant R181-000-065-112.
Based on a presentation made at the 20th Anniversary Congress of the Royal College of Ophthalmologists, Liverpool, May 2008, Professor WS Foulds as first President of the College.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Foulds, W., Kaur, C., Luu, C. et al. A role for photoreceptors in retinal oedema and angiogenesis: an additional explanation for laser treatment?. Eye 24, 918–926 (2010). https://doi.org/10.1038/eye.2009.173
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.173