Abstract
Purpose
To investigate the relationship between socioeconomic status and the extent of visual field loss in POAG and treated OHT patients at their first presentation to Manchester Royal Eye Hospital.
Methods
A cohort of 113 glaucoma patients seen between 1995 and 2005 was reviewed. The clinical parameters intraocular pressure, C : D ratio, family history of glaucoma, visual acuity, extent of visual field loss, and demographic parameters: age, gender, ethnicity, and residential postcode were extracted from hospital records. The socioeconomic status of each patient was estimated from the patient's residential postcode with the ACORN index (group 1: affluent and group 2: socioeconomically deprived).
Results
In comparison to group 1 (n=49), patients in group 2 (n=64) presented with more advanced field loss, lower educational attainment (18 vs 98% with no or unknown qualification), and were less aware of glaucoma in the family (27 vs 17%). Patients with a number of systemic health problems had worse vision, more severe visual field loss, and worse clinical attendance (P<0.05).
Conclusions
The extent of visual field loss in glaucoma patients at first presentation is related to a combination of clinical and socioeconomic factors including the patient's postcode. This finding could be used to target future case-finding resources.
Similar content being viewed by others
Introduction
Visual impairment due to glaucoma is a growing problem worldwide; although the majority of patients with this disease are successfully treated with either eye drops or surgery and retain good vision throughout the remainder of their years, about 15% progress to blindness.1 Despite important developments in both therapy and technology, glaucoma is still the second largest cause of blindness in the United Kingdom, accounting for about 12% of blind registrations and 9.6% partial sight registrations.2, 3 One of the major risk factors for future visual impairment from glaucoma is late presentation with advanced visual field loss.4, 5, 6 Although, in part, the association between prognosis and extent of visual field loss is likely to be the result of length–time bias (slowly progressing disease being detected earlier with an apparent prolonged survival time), it is a widely held view that early detection improves the patient's long-term prognosis.
One likely association for late presentation is low socioeconomic status. Poor utilisation of health-care resources, even in symptomatic conditions such as cancer, is known to be associated with lower socioeconomic status in the community.7 Fraser et al6 have shown a direct relationship between socioeconomic status and late presentation in glaucoma, and delayed response to visual loss has also been reported for other eye conditions such as amblyopia8 and cataract.9 In addition, poor compliance, late presentation, and poor care regimes have been reported in glaucoma patients with lower socioeconomic status.10
Another potential cause for late presentation is poor case finding by optometrists. In the United Kingdom, the vast majority of glaucoma cases are detected and referred by the community optometrist (∼90%),11 with the residual group being referred either directly from the patient's GP or via other hospital departments. Patients referred directly from their GPs are more likely to present with advanced visual loss,4 and an investigation of blind registrations from glaucoma at Manchester Royal Eye Hospital (MREH) has shown that there is a relatively high percentage of direct GP referrals (42 vs <10%),12 indicating poor utilisation of optometric care by patients presenting with advanced glaucoma.
The case–control nature of Fraser et al studies,3, 4, 5 using a combination of the cup-to-disc (C : D) ratio and visual field area classification to generate cases (late presenters) and controls (early presenters), limits the understanding of the risk contributing to presentation at different stages of visual field loss as does their use of a binary-coded visual field measure (advanced/early) rather than indices (eg, mean deviation—MD) derived from the now widely used static automated perimeters.
Moreover, Fraser et al, who used both an area deprivation measure (Jarman index) and three individual measures (occupational group, educational level, and access to car) of socioeconomic status, found only a weak relationship between area deprivation and extent of loss. There is often considerable heterogeneity of socioeconomic status within a ward (unit of measurement for the Jarman index, comprising of approximately 1500 households) that could act to mask the importance of area-based measures of socioeconomic status. Improved area measures (eg, ACORN index12), which classify on a much finer matrix (approximately 15 households), are now available and are likely to give a more accurate estimate of the relationship between late presentation and area-derived socioeconomic status.
The purpose of this study is to establish the relationship between the extent of visual field loss (MD) in POAG and OHT patients at first presentation to MREH and a number of clinical and socioeconomic parameters using the ACORN index.
Materials and methods
Patient selection and methods
We randomly selected 960 patients from the visual field database of the patients who attended the glaucoma clinic for the first time between 1995 and 2005. We excluded 638 patients (66%) on the basis of the exclusion criteria (tertiary referrals, ocular comorbidity, secondary glaucoma, age less than 40 years, prior hospital appointment (MREH or elsewhere), and the patient not being diagnosed with glaucoma). From the remaining cohort, we selected 113 glaucoma patients by excluding the patients who had attended the clinic before 1995 and to maintain approximately equal number of patients in the six visual field groups to satisfy the stratified sampling requirements (Figure 1).
The presenting visual field data (Humphrey 24-2 threshold; Zeiss-Humphrey Instruments, Dublin, CA, USA) of each patient were classified into one of six groups on the basis of MD (better than −5 dB, between −5 and −9.99 dB, between −10 and −14.99 dB, between −15 and −19.99 dB, between −20 and −24.99 dB, and worse than −25 dB). Stratified sampling ensured that there was an even distribution of cases within each group.
In addition, the following information was extracted from hospital records: presenting visual acuity (VA) at the first appointment, diagnosis at the initial visit, family history, intraocular pressure (IOP) both at initial referral and during follow-up, vertical C : D ratio, and referral details including clinical information available from the referral letter and ethnicity from the NHS electronic database.
The demographic details of the patients including race, residential postcode, and non-compliance with follow-up appointments were also collected from the patients' case notes and from the hospital database. The study was approved by the North Manchester Local Research Ethics Committee (04/Q1406/105).
Estimation of socioeconomic status
The socioeconomic status of the patients was estimated from the patients' residential postcode using the ACORN index.13 The ACORN index uses data sources, including 2004 census and local authority data, to detail social characteristics of the population, with a resolution for each postcode of approximately 15 residences. The ACORN index classifies individuals into five different socioeconomic groups, namely wealthy achievers, urban prosperity, comfortably off, moderate means, and hard-pressed. Several subclassifications are also available of which we included the educational level.
Analysis
Data were aggregated using MS Excel (2003) and analysed using the statistical package SPSS (SPSS ver. 13.0 for Windows; SPSS Inc., Chicago, IL, USA). Descriptive statistics were calculated for demographic, medical, and clinical characteristics. Group comparisons were made using ANOVA for continuous variable and Spearman rank correlation for categorical or nominal variables. P<0.05 was considered significant.
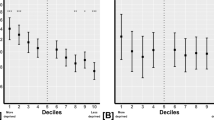
When analysing the results, the ACORN indexes were classified into two groups (group 1: wealthy achievers, urban prosperity, and comfortably off; group 2: moderate means and hard-pressed). Visual field at first presentation was classified into mild (>−5 dB), moderate (−5 to >−15 db), and severe (<−15 dB) for understanding the impact of the social status at different levels of visual field loss.
The association between the visual field loss and the risk factors was estimated using a multiple regression analysis. First, a univariate analysis was performed to determine the significant difference among the risk factors and visual field loss. The risk factor that showed significance of at least P<0.25 was considered to be included in the model. The inclusion of the variable in the model was determined by forward and backward selection and finally the variables with significance of at least P<0.1 were used in the multiple regression model.
Results
The sociodemographic and clinical characteristics of the study population are shown in Tables 1a and 1b. In 94% of the patients, the referral was initiated by an optometrist and the rest by GPs. Of these, 80% of the optometrists referred patients on the suspicion of glaucoma, whereas others were referred because of cataract (12%), complaints such as pain, lacrimation or redness (6%), or the suspicion of ocular pathology (2%). In two cases, no reason for referral was given.
The clinical diagnoses made at MREH were POAG (48%), NTG (24%), OHT (11%), and pseudoexfoliation glaucoma (7%). About 10% of the eyes were noted to have no glaucomatous changes at the first visit but 5% were diagnosed to have glaucoma at subsequent visits. The IOP was noted to be greater in the pseudoexfoliation group, and the C : D ratio was higher in NTG patients (Tables 1a and 1b). Patients with lower IOPs were generally noted to be referred as non-glaucomatous cases (ρ=−0.35, P=0.0005). As expected, hospital-based assessment of C : D ratios showed good correlation with IOP (ρ=0.23, P=0.02) and vision (ρ=−0.28, P=0.001). About 74% of the patients had some systemic problem for which they were taking medication. About a third of the patients had some other health or personal problems (eg, sick family member).
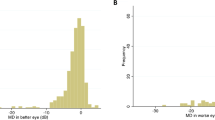
The socioeconomic status estimated by ACORN index showed good correlation (ρ=0.706, P<0.01) with the standard index of multiple deprivation (Table 1a). ACORN index classified 56% of the patients to have come from the areas of poorer socioeconomic status (group 2), a higher figure than that for the United Kingdom (Table 1a). A comparison of MD values at the first presentation between group 1 (n=49) and group 2 (n=64) for the worst-affected eye (WAE) and the least-affected eye (LAE) is shown in Figure 2a and b, respectively. Most of the patients (79%) who presented with mild loss, in the WAE, were noted to be in the affluent group (group 1). The majority of the patients (60%) with moderate loss and 63% of those presenting with severe visual field loss are noted to be from the areas of poorer socioeconomic status that is, group 2 (Figure 2a). The visual field in the fellow eye was better on average by 8.11±7.31 dB, and 56 of 113 (50%) patients had at least 6 dB difference in MD between their eyes. Again, the majority of the patients who presented with mild visual field loss in the LAE were from the more affluent group 1 (see Figure 2b).
Visual field results indicate that patients in group 1 were more likely to present with mild visual field loss (rather than moderate or severe loss) in the WAE (OR=5.89, 95% CI=1.54–22.4) and in the LAE (OR=2.68, 95% CI=1.23–5.81) than the patients in group 2. On the other hand, patients in group 2 are less likely to present with early than severe visual field loss in LAE (OR=1.178, 95% CI=1.02–1.36) compared to group 1 though it was not statistically evident in WAE (OR=1.74, 95% CI=0.81–3.63).
In group 1, 27% of the patients were known to have family history of glaucoma compared to only 17% in group 2. The education attainment (derived from the ACORN database) is much higher in group 1 than in group 2 (18 vs 98% having no or unknown qualifications) (see Figure 3). Of the patients with known ethnicity, non-White patients were older (ρ=−0.21, P=0.04) and had more systemic health problems (ρ=0.21, P=0.04). The sample size (11 non-Whites) was insufficient to make any valid judgement on the relationship between ethnicity and presenting visual field loss.
Patients who are older had poorer vision (ρ=−0.39, P=0.0005), greater visual field loss (ρ=−0.302, P=0.001), and were on treatment for more systemic health problems (ρ=−0.251, P=0.007). The frequency of non-attendance (DNA/year) after the first appointment showed a correlation with the number of systemic health problems (ρ=0.260, P=0.029) but not necessarily with increase in age (ρ=0.086, P=0.367).
A two-stage multiple regression analysis was undertaken to explore the risk factors for late presentation. Eight variables were found from a univariate analysis to correlate (P<0.25) with the amount of visual field loss in the WAE: age, IOP, ACORN grouping, VA, non-glaucoma referral, education, systemic problem, and family history (Table 2a). We did not include C : D ratio in the equation as it showed good correlation with visual field (ρ=−0.52, P=0.001), IOP (ρ=0.23, P=0.02), and vision (ρ=−0.28, P=0.001). Multiple collinearity with significant correlations (ρ>0.3, P<0.05) were also evident between some variables: education and ACORN index (ρ=−0.84, P=0.0005), IOP and non-glaucoma referral (ρ=−0.35, P=0.0005), and also between age and vision (ρ=−0.39, P=0.0005). The aim of the analysis was to ensure that the final regression did not contain variables with multiple collinearity. Initially, a multiple regression model was fitted with all eight variables, with visual field loss in the WAE as the outcome. Least significant values were removed from the model one at a time until only variables with significance of P<0.1 were included. To validate the model, the variables removed were reinserted again one by one (forward selection) to ensure that none of the omitted variables became significant in the presence of other variables.
The final model was fitted with four variables: age, ACORN grouping, vision, and IOP. Data from 104 patients were used to predict this model, which showed good reliability (R2=0.258, adjusted R2=0.23 and SE=7.42). The coefficient of the regression equation is shown in Table 2b. Loss of vision in the worst eye showed highest correlation with visual field loss. The multiple regression model constructed using the unstandardised coefficient values is

where V is the amount of visual field loss (MD value) in the worse eye, a is the presenting VA in decimal unit, b is ACORN grouping, c is IOP in mmHg, and d is age of the patient in years.
Discussion
The results of this study show a strong association between socioeconomic factors, derived from an area-based measure of deprivation, and presenting visual field loss (MD) due to glaucoma. The reason for other studies not showing such an association, despite finding a strong relationship with individual factors (occupation, tenancy, and access to a car), is most likely due to the higher fidelity of the ACORN vs Jarman index (15 vs 1500 households). The finding emphasises the importance of socioeconomic factors in glaucoma and how modern area-based indices can be used to accurately target patients at greater risk of late presentation.
This study also confirmed that high IOP and large C : D ratios are associated with more advanced visual field loss and that IOP measurements by community optometrist are well correlated to those obtained at MREH. However, the C : D ratio assessment by optometrists did not correlate well with the measurements recorded at MREH. In fact, only 55% of the NTG patients were suspected to have glaucoma by the optometrist, whereas 91% of the patients, with IOP >21 mmHg, were referred on suspicion of glaucoma. Additional training of community optometrists has been shown to improve the positive predictive value of the glaucomatous referrals.14, 15 However, we believe that case-finding performance by community optometrists is likely to vary with equipment usage and, in an environment where additional diagnostic services such as fundus photography and optic nerve head imaging are being offered for a fee, with the socioeconomic status of the patient.
The increased number of systemic health problems is often suggested to be a proxy for poor socioeconomic status and might indicate poor utilisation of health services.
Our results show a correlation between vision, visual field loss, and the number of systemic problems and old age. This finding might suggest that old age and the presence of other systemic health problems are barriers to accessing of health-care resources or it could also mean that glaucoma is associated with many systemic diseases that might aggravate the associated vascular complications or degenerative changes. The presence of other systemic problems results in poor compliance or poor attendance, as indicated by significant correlation between frequency of non-attendance in the clinic (DNA/year) and number of systemic problems.
The awareness and knowledge of glaucoma (or any other eye disease) improve with the level of education and socioeconomic status,16, 17 and this could be the reason for the finding of more systemic illness in group 1 (Table 1b). The level of compliance is also likely to be better in highly educated people.10 A recent study by Owen et al18 showed that most of the patients in the hard-pressed group (ACORN index) received less treatment than those in the wealthy achiever group, indicating a possible trend towards poor compliance. In this study, patients with poor socioeconomic status had lower educational attainment, were not aware of glaucoma in the family, and presented to the clinic with a greater level of visual loss.
The retrospective nature of this study, and averaging 15 household data by ACORN classification, limits the detailed understanding of the barriers to early presentation that exist within the United Kingdom. Further prospective work is needed to fully elucidate the importance of other factors such as the perceived costs of optometric care, mobility, and cognition.
In summary, these results provide some insight into the clinical and social risks of late presentation. Poor socioeconomic status, education level, associated systemic condition, and old age show a strong association with visual impairment in addition to the known clinical factors. Patients presenting with advanced visual field loss due to glaucoma can be identified from area-based measures of socioeconomic status; ACORN index. These relationships can be used to target populations at risk of late presentation and of becoming blind due to glaucoma.
References
Chen PP . Blindness in patients with treated open-angle glaucoma. Ophthalmology 2003; 110 (4): 726–733.
Evans JR . Causes of Blindness and Partial sight in England and Wales 1990–1991. Studies on Medical and Population Subjects Reports No. 57. HMSO: London, 1995.
Bunce C, Evans J, Fraser S, Wormald R . BD8 certification of visually impaired people. Br J Ophthalmol 1998; 82 (1): 72–76.
Fraser S, Bunce C, Wormald R . Risk factors for late presentation in chronic glaucoma. Invest Ophthalmol Vis Sci 1999; 40 (10): 2251–2257.
Fraser S, Bunce C, Wormald R . Retrospective analysis of risk factors for late presentation of chronic glaucoma. Br J Ophthalmol 1999; 83 (1): 24–28.
Fraser S, Bunce C, Wormald R, Brunner E . Deprivation and late presentation of glaucoma: case–control study. BMJ 2001; 322 (7287): 639–643.
Loehrer Sr PJ, Greger HA, Weinberger M, Musick B, Miller M, Nichols C et al. Knowledge and beliefs about cancer in a socioeconomically disadvantaged population. Cancer 1991; 68 (7): 1665–1671.
Smith LK, Thompson JR, Woodruff G, Hiscox F . Social deprivation and age at presentation in amblyopia. J Public Health Med 1994; 16 (3): 348–351.
Tielsch JM, Sommer A, Katz J, Quigley H, Ezrine S . Socioeconomic status and visual impairment among urban Americans. Baltimore Eye Survey Research Group. Arch Ophthalmol 1991; 109 (5): 637–641.
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW . Compliance barriers in glaucoma: a systematic classification. J Glaucoma 2003; 12 (5): 393–398.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR . An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol 1994; 1 (1): 31–39.
Henson DB, Thampy R . Preventing blindness from glaucoma. BMJ 2005; 331 (7509): 120–121.
CACI. ACORN User Guidehttp://www.caci.co.uk/pdfs/Acorn%20Guide.pdf. [accessed January 2007]. 2006.
Theodossiades J, Murdoch I, Cousens S . Glaucoma case finding: a cluster-randomised intervention trial. Eye 2004; 18 (5): 483–490.
Patel UD, Murdoch IE, Theodossiades J . Glaucoma detection in the community: does ongoing training of optometrists have a lasting effect? Eye 2006; 20 (5): 591–594.
Livingston PM, Lee SE, De Paola C, Carson CA, Guest CS, Taylor HR . Knowledge of glaucoma, and its relationship to self-care practices, in a population sample. Aust N Z J Ophthalmol 1995; 23 (1): 37–41.
Dandona R, Dandona L . Socioeconomic status and blindness. Br J Ophthalmol 2001; 85 (12): 1484–1488.
Owen CG, Carey IM, De Wilde S, Whincup PH, Wormald R, Cook DG . The epidemiology of medical treatment for glaucoma and ocular hypertension in the United Kingdom: 1994–2003. Br J Ophthalmol 2006; 90 (7): 861–868.
Acknowledgements
This research was supported by a grant from the BUPA Foundation. We thank Dr Richard Worlmald, Dr Paul Spry, and an anonymous reviewer for their valuable suggestions to the previous version of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sukumar, S., Spencer, F., Fenerty, C. et al. The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye 23, 1038–1044 (2009). https://doi.org/10.1038/eye.2008.245
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.245
Keywords
This article is cited by
-
Deprivation and the location of primary care optometry services in England
Eye (2024)
-
Determinants of late presentation of glaucoma in Hong Kong
Eye (2023)
-
Measures of multiple deprivation and visual field loss in glaucoma clinics in England: lessons from big data
Eye (2023)
-
Advanced glaucoma at diagnosis: current perspectives
Eye (2020)
-
Impact of socioeconomic status on vision-related quality of life in primary open-angle glaucoma
Eye (2017)