Abstract
Purpose
To evaluate the incidence and clinical features of patients with ocular toxoplasmosis in a Colombian cohort.
Methods
We collected prospectively the clinical features of patients with ocular toxoplasmosis seen at the ‘Universidad del Quindio’ health centre between September 2005 and September 2007 (24 months).
Results
Seventy patients were included in the analysis (95 affected eyes). The median age at the first episode was 21 years (range: 1–54 years). Thirty-two patients had active lesions (45.7%), one of them had active lesions in both eyes. The acquisition of infection was determined in 14 patients as congenital (20%), in seven as an acquired postnatal infection (10%), and in 49 as undetermined (70%). Bilateral involvement was found in 25 cases (35.7%). Unilateral legal blindness (<20/200) was found in 14 of 37 inactive cases (37.8%). The most frequent complication was strabismus (n: 12; 13.4%).
Conclusions
There is a high incidence of cases of ocular toxoplasmosis in Quindio region (three new episodes by 100 000 inhabitants by year). Clinical features of ocular toxoplasmosis in Colombia are similar to those reported in other regions but there are no comparative data about the size and number of lesions.
Similar content being viewed by others
Introduction
Ocular toxoplasmosis is the most common cause of posterior uveitis and in some countries is one of the most important causes of visual impairment.1 Although congenital infection was considered to be the most important origin of the infection, this has been recently re-evaluated, and in Colombia it was estimated that 5.5% of the population have retinochoroidal scars after a non-congenital infection and 20% of these persons have reduced visual capacity.2 With 41 million inhabitants and 47% of them infected,3 this would mean around 1 million Colombians with retinochoroidal scars and at least 200 000 with unilateral legal blindness due to this infection. In comparison, congenital infection is estimated to affect 4500 newborns each year, and 30% of them will have retinochoroidal lesions.4 A study in Colombia found that toxoplasmosis was the second commonest cause of congenital blindness.5
There are no previous reports that describe the clinical features of ocular toxoplasmosis in Colombia, and it is suspected that strains in South America are more virulent than in other parts of the world.6, 7 Therefore, we collected the clinical characteristics of patients seen at our clinic to determine if there exist variations in clinical characteristics with reference to those reported in other countries.
Patients and methods
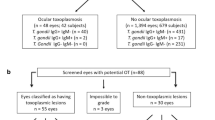
The study included 70 consecutive patients examined at the toxoplasmosis clinic of the Universidad Quindio (Colombia). We collected prospective clinical and laboratory medical records of all patients seen during September 2005 and September 2007 (24 months) simultaneously with a collection of serum for a serogenotyping project aimed to determine the clonal types of Toxoplasma that infect Colombian patients with ocular toxoplasmosis. The present report refers only to the clinical characteristics and incidence observed during the time of sample collection. All of 12 ophthalmologists who work at the Quindio region (534 522 inhabitants) were requested to refer their patients with active or inactive lesions.
The clinical diagnosis of ocular toxoplasmosis was based on criteria described previously.8 Active ocular toxoplasmosis was defined by the presence of an active creamy-white focal retinal lesion eventually resulting in hyperpigmented retinochoroidal scars in either eye. Primary ocular toxoplasmosis was defined as an active creamy-white focal retinal lesion without associated pigmented retinochoroidal scars in either eye. Recurrent ocular toxoplasmosis was defined as an active retinochoroidal lesion in the presence of old pigmented retinochoroidal scars in either eye. Central lesions were defined as lesions located within the large vascular arcades. A complete ocular examination was performed at each visit, including best-corrected Snellen visual acuity, slit-lamp biomicroscopy, tonometry, and indirect ophthalmoscopy. All patients included in the study had fundus drawings and/or colour fundus photography. Angiographic studies were performed only in selected cases. Patients were seen at 1-week intervals until the resolution of each active episode and then were called for follow-up visits every 6 months or whenever they had new symptoms. All patients or their legal tutors for minors signed an informed consent.
Serological criteria for the acute phase of systemic infection with Toxoplasma gondii included the presence of specific IgM antibodies. All patients with primary lesions were examined for the presence of IgM and for comparison purposes this assay was also requested in some patients with recurrent lesions or in the quiescent phase. The chronic phase of systemic infection was defined as positive IgG antibodies (any positive titre) without IgM antibodies. T. gondii serology was performed routinely in all cases by an ELISA IgG and IgM commercial assays (Human, Germany). Congenital infection was defined by the presence of a PCR assay positive on amniotic fluid during pregnancy or as ocular symptoms at birth accompanied or not by neurological symptoms (micro or macrocephaly or cerebral calcifications) with a persistent IgG anti-Toxoplasma at 12 months of life. We defined an acquired infection in adult (>18 years of age) with a specific IgM-positive test. Patients less than 18 years of age and with IgM were considered to be of uncertain origin because we have previously found some patients with confirmed congenital toxoplasmosis with persistent specific IgM-positive test up to 10 years of age.
Legal blindness was defined as the best-corrected visual acuity of the affected eye equal to or less than 20/200. Visual outcome was determined by the final optimal visual acuity (not the worst visual acuity at any visit). Patients without ophthalmologic evaluation and those without IgG anti-Toxoplasma antibodies were excluded.
Differences in proportions among groups were compared by means of the χ2 test and Fisher's exact test.
Results
Eighty-one patients were examined during the period of 24 months (2005–2007), and 70 patients were included for the analysis (95 affected eyes). Eleven patients were excluded, seven because they did not have the Toxoplasma serological test and four because data were incomplete. Sixty-six patients were from the region of Quindio (centre west of Colombia, 534 552 inhabitants) and only four were from outside this region. We then contacted by phone all the ophthalmologists to confirm that they referred all their patients. According to their answers, the percentage of referring was between 80 and 100% during the period of the study. The distribution by gender was 37 women (53%) and 33 men (47%). Bilateral involvement was found in 25 of 70 cases (35.7%). Unilateral legal blindness (VA <20/200) was found in 14 of 37 inactive cases (37.8%). The median age at the first episode was 21 years (range: 1–54 years). The acquisition of infection was determined in 14 patients as congenital (20%), in seven as an acquired postnatal infection (10%), and in 49 as undetermined (70%). Two patients were also HIV-infected, one with an inactive chorioretinal scar and the other with an active chorioretinal macular lesion.
Thirty-two patients (45%) had active lesions; one of them had active lesions in both the eyes (3%). All active patients were from Quindio; therefore, the incidence was of three new episodes per year for each 100 000 inhabitants. Primary lesions were found in 13 of the 32 patients (40.6%); the median age of this group was 32 years (range: 13–60). In 19 of 32 patients (59.3%), there were concomitant inflammatory lesions and retinochoroidal scars (recurrent toxoplasmosis). The median age of this group with active lesions was 25 years (range: 7–44).
The IgM-specific assay was positive in 3 of 13 patients with primary lesions (23%) and in 2 of 16 (12%) with pigmented scars (recurrent lesion). The IgM was also positive in 3 of 11 (27%) children with congenital infection. Bilateral ocular involvement was more common in the congenitally infected group than in the postnatally acquired infected group (12 of 14, 85.7% vs 1 of 7, 14.2%; Fisher exact test: P=0.003).
The most common symptoms in 32 patients during the active phase were blurred vision in 32 (100%), floaters in 24 (75%), ocular pain in 16 (50%), and photophobia in 12 (37.5%). In 33 eyes with active lesions, there were vitritis in 26 (78.7%), anterior uveitis in 14 (42.4%), vasculitis in 8 (24%) (Figure 1), and papillitis in 7 (21.2%) (Figure 2). The percentage of women with anterior uveitis (12/21; 57%) was greater than that in men (2/11; 18%). This difference was statistically significant (Fisher's exact test one tail: P=0.03).
In 89 eyes (six eyes were lost to follow-up and they were seen only during the period of vitritis), the median number of lesions was two (range: 1–11). No difference in the number of lesions was found between congenital or acquired infections (mean: 1.8±1.6 vs 1.8±1.5). The median lesion size (area of active retinitis not the retinochoroidal scar) was 1 disc diameter (range: 0.5–7). Size of lesion was greater than 3 disc diameters in 2 of 12 patients with congenital infection (16%) vs one of seven patients (14%) with acquired infection. Localization of lesions was in the macula in 65 (73%) and in the peripheral retina in 24 (26%) of 89 eyes. In 14 patients (15.7%), there were central and peripheral lesions simultaneously. The most frequent complications were strabismus (n: 12; 13.4%); posterior synechiae (n: 9; 10.1%); ocular hypertension (n: 4; 4.4%); cataracts (n: 4; 4.4%); and cystoid macular oedema (n: 4; 4.4%).
Discussion
We found a high incidence of ocular toxoplasmosis (three new episodes per 100 000 inhabitants) as compared to that reported in England of 0.08 per 100 000 inhabitants.9 There was no difference in gender distribution of the disease, and the age of presentation was similar to that reported in other series10, 11 but the 37% of definitive unilateral blindness is higher than the 24% reported in the Netherlands.10 Primary lesions were less frequent than recurrent lesions in a similar manner to previous case series.10, 11 The frequency of 17% of a positive IgM assay was lower than that reported previously of 47% for patients during the acute phase of ocular toxoplasmosis in the same region in Colombia by the high-sensitive assay ISAGA and of 37% in Iran.12, 13 This could be partly explained by the different commercial assays used. Our series includes a high number of congenital cases and we confirm that in these cases bilateral involvement was more frequent as reported by other authors.10 Interestingly, anterior uveitis was more frequent in women than in men; there are no previous reports of this association.
Many characteristics of the lesions are similar to those previously reported10, 11, 13 with a predominance of macular localization. Papillitis has been described as an atypical presentation in ocular toxoplasmosis; we found this in 7% of cases, which is near to the 5% reported in Turkey.11 There were six patients with chorioretinitis without frank vitritis (18%), which could be explained by a low inflammatory reaction in these cases. There are no available data in the literature to determine whether our patients have a different number or size of lesions relative to other geographical regions; however, we did not observe differences between acquired and the congenital presentation. Our impression is that it is possible to find severe clinical cases in the acquired form, yet bilateral involvement was more common in congenital form.
In conclusion, we found a high prevalence of ocular toxoplasmosis in the Quindio region, with an important effect on visual health. We need to complete a follow-up of our patients to determine if differences in treatment can explain the higher percentage of unilateral visual blindness. Some differences between South American and European clinical case series have been found in the rate of congenital transmission, in the probability of symptoms in congenital infection, and in the difference in frequency of serological markers in ocular toxoplasmosis.6, 7, 12 Therefore, it would be important to make a multicentre clinical study to confirm the existence of a more severe clinical picture in South America.
References
Holland GN . Ocular toxoplasmosis: a global reassessment. Part I: epidemiology and course of disease. Am J Ophthalmol 2003; 136: 973–988.
de-la-Torre A, Gonzalez G, Diaz-Ramirez J, Gomez-Marin JE . Screening by ophthalmoscopy for Toxoplasma retinochoroiditis in Colombia. Am J Ophthalmol 2007; 143: 354–356.
Gómez JE, Castaño JC, Montoya MT . Toxoplasmosis congénita en Colombia: Un problema subestimado de salud pública. Colombia Médica 1995; 26: 66–70.
Gomez-Marin JE, delaTorre A . Positive benefit of postnatal treatment in congenital toxoplasmosis. Arch Dis Child 2007; 92: 88–89.
Zuluaga C, Sierra MV, Asprilla E . Causas de ceguera infantil en Cali. Colombia Medica 2005; 36: 25–238.
SYROCOT. Effectiveness of prenatal treatment for congenital toxoplasmosis: a metanalysis of individual patient's data. Lancet 2007; 369: 115–122.
Gomez Marin JE . New world and old world Toxoplasma: do they have a clinical relevance? Infectio 2007; S1: 26–28.
Holland GN, O’Connor GR, Belfort Jr R, Remington JS . Toxoplasmosis. In: Pepose JS, Holland GN, Wilhelmus KR (eds). Ocular Infection and Immunity. Mosby: St Louis, MO, 1996, pp 1183–1223.
Gilbert RE, Dunn DT, Lightman S, Murray PI, Pavesio CE, Gormley PD et al. Incidence of symptomatic toxoplasma eye disease: aetiology and public health implications. Epidemiol Infect 1999; 123: 283–289.
Bosch-Driessen L, Berendscho T, Ongkosuwito JV, Rothova A . Ocular toxoplasmosis: clinical features and prognosis of 154 patients. Ophthalmology 2002; 109: 869–878.
Atmaca LS, Simsek T, Batioglu F . Clinical features and prognosis in ocular toxoplasmosis. Jpn J Ophthalmol 2004; 48: 386–391.
Soheilian M, Sadoughi MM, Ghajarnia M, Dehghan MH, Yazdani S, Behboudi H et al. Prospective randomized trial of trimethoprim/sulfamethoxazole versus pyrimethamine and sulfadiazine in the treatment of ocular toxoplasmosis. Ophthalmology 2005; 112: 1876–1882.
Gomez-Marin JE, Montoya-De-Londono MT, Castano-Osorio JC, Heine FA, Duque AM, Chemla C et al. Frequency of specific anti-Toxoplasma gondii IgM, IgA and IgE in Colombian patients with acute and chronic ocular toxoplasmosis. Mem Inst Oswaldo Cruz 2000; 95: 89–94.
Acknowledgements
We thank the patients and the ophthalmologists of Quindio who referred the patients.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de-la-Torre, A., López-Castillo, C. & Gómez-Marín, J. Incidence and clinical characteristics in a Colombian cohort of ocular toxoplasmosis. Eye 23, 1090–1093 (2009). https://doi.org/10.1038/eye.2008.219
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.219
Keywords
This article is cited by
-
Outcomes of trimethoprim/ sulfamethoxazole treatment for ocular toxoplasmosis in Congolese patients
BMC Ophthalmology (2023)
-
Chorio-retinal toxoplasmosis: treatment outcomes, lesion evolution and long-term follow-up in a single tertiary center
International Ophthalmology (2020)
-
An overview of seventy years of research (1944 – 2014) on toxoplasmosis in Colombia, South America
Parasites & Vectors (2014)
-
Th1 and Th2 immune response to P30 and ROP18 peptides in human toxoplasmosis
Medical Microbiology and Immunology (2014)
-
Clinical pattern of ocular toxoplasmosis treated in a referral centre in Serbia
Eye (2012)