Abstract
Diisocyanate (DI) is the most common cause of occupational asthma (OA) in Korea. Mannose-binding lectin (MBL) initiates the lectin complement activation pathway following oxidative stress and plays an important role in the regulation of inflammatory processes. To determine whether there is a genetic association between MBL2 polymorphisms and DI-OA, 99 patients with DI-OA, 99 asymptomatic exposed controls (AECs) and 144 unexposed normal controls were enrolled in this study. Three polymorphisms (−554 G>C, −431A>C and −225 G>C) in the MBL2 promoter were genotyped, and serum MBL levels were determined by enzyme-linked immunosorbent assay. Functional variabilities in the promoter polymorphisms were analyzed by a luciferase reporter assay and electrophoretic mobility shift assay (EMSA). A significantly higher frequency of haplotype (ht) 2 [CAG] was noted in the DI-OA group compared with the AEC group (P=0.044). The patients with DI-OA carrying ht2 [CAG] had significantly lower PC20 methacholine levels (P<0.001) than the non-carriers. The serum MBL levels were significantly higher in the DI-exposed subjects (both the DI-OA patients and AECs) carrying ht1 [GAG] (P=0.028). Luciferase activity was significantly enhanced in ht1 [GAG] compared with ht2 [CAG] in human hepatocarcinoma cells (Hep3B) (P=0.002). The EMSA showed that a −554G probe produced a specific shifted band compared with the −554C probe. These findings suggest that decreased serum MBL levels due to polymorphisms of the MBL2 gene may increase susceptibility to the development of DI-OA in DI-exposed individuals.
Similar content being viewed by others
Introduction
Diisocyanates (DIs) are highly reactive chemicals and well-known triggers of occupational asthma (OA).1 Toluene DI, 4,4-methylenediphenyl DI and hexamethylene DI are DIs that constitute a group of low-molecular weight agents used in various manufacturing industries, such as painting, construction and wood-working.2, 3 In particular, toluene DI is the most common cause of OA in Korea with a prevalence of 2.9–13% among exposed workers.4, 5
DI-induced OA (DI-OA) is characterized by chronic airway inflammation with remodeling and hyperresponsiveness.6 The pathogenic mechanisms of DI-OA have not yet been elucidated; however, several immunological and non-immunological mechanisms have been suggested.2, 7 Oxidative stress, which plays an important role in the pathogenesis of airway inflammation, has been suggested to be a pathogenic mechanism of DI-OA.8 It has been demonstrated that inflammation driven by increased oxidative stress occurs in the airways of asthmatic patients.9 In cases of DI-OA, inhaled DI causes tissue injury, activating both inflammatory and bronchial epithelial cells, which generate reactive oxygen species (ROS) and nitrogen species that cause oxidative stress.10 Increased production of ROS has also been noted in macrophages, antigen-presenting cells, neutrophils and eosinophils within the lungs of patients with asthma, which can further exacerbate asthma by increasing airway hyperresponsiveness and triggering inflammation.11
Studies have suggested that oxidative stress can induce mannose-binding lectin-mediated complement activation.12, 13 Because complement activation is involved in innate defense mechanisms, it could play an important role in the regulation of airway inflammation. The presence of mannose-binding lectin (MBL) in the bronchoalveolar lavage fluid of children with airway infections and not in that of controls suggests its role in pulmonary defense.14 It has been shown that oxidative stress can decrease functional airway MBL in chronic obstructive pulmonary disease patients.15 Similarly, nebulized administration of human plasma-derived MBL at clinically achievable concentrations significantly reduced inflammation and improved efferocytosis in a smoking mouse model, restoring pulmonary macrophage efferocytic ability and reducing airway inflammation, suggesting that it might play an important role in attenuating inflammation induced by oxidative stress.15
MBL is an important serum protein of the innate immune system produced mainly by hepatocytes. It selectively recognizes the carbohydrate patterns of infectious agents or infected cells and then opsonizes antigens and activates the lectin complement pathway system.16 MBL triggers opsonophagocytosis and is involved in the modulation of inflammation by initiating the lectin complement pathway.17 The human MBL 2 (MBL2) gene is located on chromosome 10q11.2-q21 and encodes MBL.18 Six single nucleotide polymorphisms (SNPs) of MBL2 have been associated with altered serum MBL levels in population studies.19, 20 In addition, our previous study has suggested that MBL2 gene polymorphisms can alter serum MBL levels in Korean adult asthmatics.21 However, it is not known whether an alteration in the MBL serum level due to MBL2 genetic variants could have an influence on DI-OA.
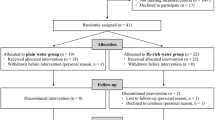
On the basis of these observations, we investigated genetic polymorphisms of the MBL2 gene and serum MBL levels associated with MBL2 variants in patients with DI-OA. A case–control study was performed, in which three groups were evaluated as follows: DI-OA, asymptomatic exposed controls (AECs) and normal controls (NCs). The functional effects of MBL2 polymorphisms were evaluated using a luciferase reporter assay and electrophoretic mobility shift assay (EMSA).
Materials and methods
Study subjects
Ninety-nine patients with DI-OA were enrolled from a pool of volunteers who had been exposed to DI in their workplaces, which included spray painting, furniture polishing, and the musical instrument and car industries. The DI-OA phenotype was determined by positive responses to the DI-bronchial challenge test, which was performed at the Ajou University Medical Center, Suwon, South Korea. Ninety-nine AECs who worked in environments similar to those of the patients with DI-OA and 144 unexposed NCs were recruited from the pool of volunteers. Written informed consent was obtained from all subjects, and the Institutional Review Board of Ajou University Hospital approved the study. Skin-prick tests were performed with 55 common aeroallergens (Bencard Co., Bredford, UK), and atopy was defined as one or more positive reactions to common inhalant allergens. Total IgE concentrations were measured using an ImmunoCAP system (Thermo Scientific, Uppsala, Sweden) according to the manufacturer’s instructions.
DI-bronchial challenge test
The DI-bronchial challenge test was performed according to a protocol previously described.4, 22
Detection of IgE and IgG antibodies specific to DI-human serum albumin conjugate
Serum-specific IgE and IgG levels were determined by enzyme-linked immunosorbent assay as previously described.23 A vapor-type DI-human serum albumin (HSA) conjugate was prepared from 80% of 2, 4-DI isomers based on a recently described DI vapor-phase exposure system.23 Specific DI binding was calculated as the difference in optical density between mock-conjugated and DI-albumin wells. Positive cutoff values were based on the mean±two standard deviations of the absorbance values obtained from tests with unexposed healthy controls.
DNA extraction, SNP identification and genotyping
Total genomic DNA was isolated from peripheral blood samples using a Puregene DNA Purification Kit (Gentra, Minneapolis, MN, USA) according to the manufacturer’s protocol. On the basis of previous findings21 and the SNP sequencing results, we chose three SNPs in the MBL2 promoter (−554 G>C, −431A>C and −225 G>C). Samples were genotyped for the three SNPs by a TaqMan allelic discrimination assay using TaqMan probes (Applied Biosystems, Foster City, CA, USA). The sequences of the primers and probes used for SNP genotyping have been previously reported.21
Measurement of human serum MBL level
The serum MBL level was measured using a human MBL DuoSet ELISA Development Kit (R&D Systems, Minneapolis, MN, USA). Serum samples were stored at −80 °C prior to measurement.
Cell culture and preparation of MBL2 constructs for promoter assays
Hep3B cells (human hepatocarcinoma cells) were maintained in Dulbecco’s modified Eagle’s medium (Gibco, Grand Island, NY, USA) supplemented with 10% heat-inactivated fetal bovine serum (Gibco), 100 U ml−1 penicillin G sodium and 100 μg ml−1 streptomycin sulfate (Gibco), and cultured at 37 °C in humidified 95% air and 5% CO2. A 1239-bp fragment of the human MBL2 gene was prepared by PCR amplification using human genomic DNA as a template (forward primer: 5′-GCTAGGCTGCTGAGGTTTCTT-3′ and reverse primer: 5′-GGGCTGGCAAGACAACTATTAG-3′). The PCR products, haplotype (ht) 1 [G−554A−431G−225] and ht2 [C−554A−431G−225], were used as templates for the cloning construct. Each PCR product was gel-purified with an agarose gel purification kit (GeneAll Biotech, Seoul, Korea) and ligated into a TOPO vector (Invitrogen, Carlsbad, CA, USA). The plasmid was digested with KpnІ and XhoІ (Takara, Shuzo, Japan) and ligated into a pGL3-basic luciferase reporter vector (Promega, Madison, WI, USA) using T4 DNA ligase (Elpis Biotech, Daejeon, Korea). All constructs were confirmed by restriction enzyme analysis and DNA sequencing. Plasmid DNAs were prepared from these constructs using an Endo Free Plasmid Maxi Kit (Qiagen, Hilden, Germany), and concentrations and purity were assessed by UV spectrophotometry and agarose gel electrophoresis.
Transient transfection for luciferase activity assessment
Transfection of Hep3B cells was performed. Detailed transfection protocols have been described in our previous study.24 Hep3B cells were transfected using a microporator (model MP-100; Digital Biotechnology, Seoul, Korea) and an MPK-1096 solution kit (Digital Biotechnology) according to the manufacturer’s instructions. Briefly, 12-well plates were filled with 1000 μl of Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum. Plates were incubated in a humidified incubator at 37 °C and 5% CO2. Hep3B cells (2 × 105 cells per well), reporter plasmid DNA containing MBL2 (1 μg) and Renilla plasmid DNA (5 ng) were suspended in 10 μl Solution R (MPK-1096). The incorporation tube was filled with 3 ml Solution E (MPK-1096). The cell and DNA mixtures were inserted into a microporator pipette station. The Hep3B cells were shocked using the following settings: 850 V, 60-ms pulse width and one pulse. The samples were transferred to preincubated 12-well plates and incubated for 24 h. The cells were lysed with 100 μl per well of passive lysis buffer (Promega). A 10-μl aliquot from each well was assayed for luciferase activity using a Dual-Luciferase Reporter Assay Kit (Promega) and a Clarity Luminescence microplate reader (BioTek, Winooski, VT, USA). pGL3-control (Promega) and promoterless pGL3-basic vectors were used as positive and negative controls, respectively. Transfection efficiency was determined by measuring Renilla activity using a Dual-Luciferase Reporter Assay Kit (Promega) after co-transfection of both the reporter construct and the Renilla control vector into the cell line.
Nuclear extract preparation and EMSA
Nuclear extracts were prepared from Hep3B cells, and protein concentrations were determined using the Bradford assay as previously described.25 Samples were stored at −80 °C until use. The double-stranded oligonucleotide sequences for MBL2 −554G and −554C were 5′-GCAAGCCTGTGTAAAACACCA-3′ and 5′-GCAAGCCTGTCTAAAACACCA-3′, respectively. Competitor oligonucleotide nuclear factor-κB (NF-κB) (5′-AGTTGAGGGGACTTTCCCAGG-3′) and activating protein-1 (AP-1) (5′-TTCCGGCTGAGTCATCAAGCG-3′) were used as probes for the EMSA. Oligonucleotides and their complementary strands were designed and purchased (Bioneer, Daejeon, Korea). Preparation of double-stranded oligonucleotides, radiolabeled DNA probes and reaction mixtures was performed as previously described. For the competition experiments, unlabeled blunt-ended competitor oligonucleotides were added to the binding reaction mixtures before addition of the radiolabeled oligonucleotide probe. The gels were dried, and radioactivity was detected using a FLA-7000 scanner and Multi Gauge software ver. 3.0 (Fuji Photo Film Co., Ltd., Tokyo, Japan).
Statistical analysis
Statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) version 12.0 software (SPSS Inc., Chicago, IL, USA). Genotype frequency was examined for the subject groups using a χ2 test, and differences in genotype and haplotype frequencies were examined using a logistic regression analysis with co-dominant, dominant and recessive models after accounting for age and sex as co-variables. Differences in clinical characteristics among the groups were examined using the independent t-test for continuous variables and the χ2 test for categorical variables. Statistical significance was established at P<0.05.
Results
Clinical characteristics of the study subjects
The clinical characteristics of the study population are summarized in Table 1. The mean age of the patients with DI-OA was 42.46 years (±9.71) and that of the unexposed NCs was 33.19 years (±13.54) (P<0.001). The prevalence of males was significantly higher in the DI-OA group than in the NC group (65.66% male DI-OA patients and 40.28% male NCs) (P<0.001). In addition, the atopy rate was also significantly higher for the patients with DI-OA (41.67% for the DI-OA patients and 14.1% for the NC group) (P<0.001). The serum total IgE level of the patients with DI-OA was 274.49 IU ml−1 (±420.51), and that of the NCs was 87.95 IU ml−1 (±112.42) (P=0.001). The patients with DI-OA had a higher prevalence of serum-specific IgE and IgG to DI-HSA conjugates than those in the control groups (21.88% serum-specific IgE to DI-HSA and 28.13% serum-specific IgG to DI-HSA) (P=0.013 and P=0.009, respectively). No significant differences were observed in the serum MBL levels between the patients with DI-OA and those in the control groups (Table 1). However, the DI-exposed workers (both the DI-OA and AEC subjects) tended to have higher serum MBL levels than those in the NC group (610.05±455.08 vs 425.36±186.55 μg l−1; data not shown).
MBL2 genotype and haplotype frequencies
We selected three MBL2 SNPs (−554 G>C, −431A>C and −225G>C) for this study. Linkage disequilibrium analyses were performed among the three SNPs. Four common haplotypes, ht1 [GAG], ht2 [CAG], ht3 [CAC] and ht4 [CCG], were constructed utilizing the EM algorithm. Tables 2 and 3 show the genotype and haplotype frequencies, respectively, of each MBL2 SNP in the study subjects. A significantly higher frequency of the AA genotype at −431 A>C was noted in the DI-OA group compared with the AEC group (P=0.016, both in the co-dominant and recessive analysis models), but no significant differences among the study groups were noted in the genotype frequencies of the −554 G>C and −225 G>C polymorphisms. A higher frequency of ht2 [CAG] was noted in the DI-OA group in the recessive analysis model compared with the AEC group (P=0.044 in the recessive analysis model), but no significant differences in ht1 [GAG], ht3 [CAC] or ht4 [CCG] were noted among the study groups.
Serum MBL levels according to MBL2 genotype and haplotype in DI-exposed workers
Significant differences in serum MBL levels were observed according to the MBL2 polymorphisms in the DI-exposed workers (both the DI-OA and AEC subjects). Subjects carrying ht1 [GAG] showed significantly higher serum MBL levels than those with other haplotypes (743.85±404.11 vs 553.33±465.55 μg l−1, P=0.028; Figure 1).
PC20 methacholine levels according to MBL2 haplotype 2 [CAG] in patients with DI- OA
PC20 methacholine levels were assessed according to MBL2 polymorphism in the patients with DI-OA. The patients with DI-OA carrying ht2 [CAG] showed significantly lower PC20 methacholine levels than those of the patients with other genotypes and haplotypes (1.32±1.92 vs 6.07±8.14 pg ml−1, P<0.001; Figure 2). Other clinical parameters, including atopy, baseline FEV1% and other immunological findings, were not significantly different according to MBL2 genotype or haplotype frequency (data not shown).
Effects of MBL2 polymorphisms on transcriptional activity between haplotype 1 [GAG] and haplotype 2 [CAG]
We performed a luciferase reporter assay using the haplotype constructs ht1 [GAG] and ht2 [CAG] to determine the transcriptional effects of the MBL2 −554 G>C polymorphisms. A construct composed of the MBL2 sequence and a luciferase reporter gene was transfected into Hep3B cells. Reporter activities were compared between ht1 [GAG] and ht2 [CAG] in MBL2. Luciferase activity was significantly enhanced in the ht1 [GAG] construct compared with ht2 [CAG] in the Hep3B cells (P=0.002, Figure 3).
Effect of the MBL2 –554 G>C polymorphism on transcriptional activity. (a) Schematic representation of the reporter gene construct containing the MBL2 promoter region with –554 G>C polymorphisms. (b) Transfection of MBL2 –554 G>C polymorphisms (ht1 [GAG] and ht2 [CAG]) into Hep3B cells. The data represent the mean values of three independent experiments±s.d. (total, n=9).
Electrophoretic mobility shift assay (EMSA)
To determine whether the −554 G>C polymorphism altered transcription factor binding affinity, we performed an EMSA with nuclear extracts from Hep3B cells using double-stranded oligonucleotide probes that corresponded to −554 G>C. The −554G probe produced a specific band that differed from that of the −554C probe (Figure 4).
Electrophoretic mobility shift assay of MBL2 –554 G>C polymorphisms using nuclear extracts obtained from human hepatocarcinoma cells (Hep3B). (a) Oligonucleotide sequences were used as a probe and competitor (–554G and –554C, respectively). The boldface characters indicate –554 G>C. (b) Differential binding of nuclear proteins to –554 G>C alleles. Transcription factor binding to the –554G probe was assessed by a competitive binding assay. Competitors were present at 50- and 100-fold molar excess compared with the probe. NF-κB: nuclear factor-κB; AP-1: activator protein-1.
Discussion
DI-OA is a complex disease influenced by multiple genetic and environmental factors. Oxidative stress has been described as a trigger that aids in the development of DI-OA.8 Moreover, it can aggravate airway inflammation by inducing pro-inflammatory mediators, stimulating bronchospasms, enhancing bronchial hyperresponsiveness and increasing mucus production.26, 27 However, the specific mechanism has not yet been determined. ROS generated during oxidative stress can lead to compromised cellular functioning and increased inflammation by damaging nucleic acids, lipids, proteins and mitochondria.28 ROS may act as signaling modifiers of transcription factors, such as NF-κB and AP-1, in epithelial cells, which can activate genes encoding many pro-inflammatory cytokines and adhesion molecules, thus inducing the inflammatory response.29, 30 Oxidative-stress-induced MBL-complement activation plays an important role in modulating the inflammatory response; however, the role of MBL in asthma remains obscure.12, 13 Protective as well as deleterious roles of MBL have been shown in different studies of asthmatic patients.31, 32, 33 MBL is a key regulator of inflammation and provides a first line of defense through complement activation.34 Accumulation of MBL in bronchoalveolar lavage fluid during pulmonary inflammation has been reported, whereas no MBL was detected in the non-disease group.14 In addition, MBL levels in bronchoalveolar lavage fluid were significantly higher in patients with acute pulmonary inflammation compared with those with chronic inflammation, suggesting that MBL can play a defensive role against airway inflammation.14 Low serum MBL levels due to MBL2 genetic variants may fail to counteract the inflammation induced by oxidative stress, resulting in DI-OA. Therefore, we hypothesized that MBL2 gene polymorphisms affect serum MBL levels and increase susceptibility to DI-OA.
Several association studies of the MBL2 gene have been conducted in various ethnic groups and in both children and adult patients with asthma. Aittoniemi et al.32 have demonstrated that the carriage of a promoter region variant, −221 G>C, which causes low MBL expression, is a significant risk factor for asthma in Finnish populations. Similarly, MBL insufficiency has been reported to contribute to the development and maintenance of airway hyperresponsiveness during chronic fungal asthma.31 Oxidative stress has been shown to decrease functional airway MBL in chronic obstructive pulmonary disease by increasing susceptibility to degradation.15 To our knowledge, this is the first study to investigate a possible association between DI-OA and promoter polymorphisms of MBL2. In this study, we noted a significant difference in the frequency of ht2 [CAG] between the DI-OA and AEC groups. We also found severe airway hyperresponsiveness in the DI-OA patients carrying ht2 [CAG], indicating that they were more susceptible to the development of this symptom. Airway hyperresponsiveness in patients with DI-OA is one of the most important clinical features and has been used for diagnostic assessment.35, 36, 37 We noted a significantly higher prevalence of serum-specific IgE to DI-HSA in the DI-OA subjects compared with the AEC subjects. In our previous study, we have shown that the level of serum-specific IgE to DI-HSA is significantly higher in DI-OA patients compared with unexposed healthy controls.38 Serum IgE levels are usually elevated in asthmatic patients, adversely affecting asthma pathogenesis.39
In vitro experiments have shown that DI can induce oxidative stress in the lungs and affect the function of lung tissue.40, 41 Hodge et al.42 have demonstrated that MBL facilitates the reduction in lung inflammation induced by cigarette smoking in a mouse model. Our results also support these previous findings. The functional study of MBL2 promoter polymorphisms in the Hep3B cell line showed differential transcriptional regulation by dual-luciferase activity. The decreased promoter activity observed for MBL2 ht2 [CAG] compared with ht1 [GAG] suggests that MBL2 expression is downregulated in liver cells in the presence of MBL2 ht2 [CAG]. Thus, in subjects with ht2 [CAG], the protective role of MBL against oxidative stress induced by DI is reduced, which may lead to DI-OA.
In addition, the EMSA results revealed that −554G-specific DNA binding was more prominent compared with −554C and that this binding may be important in the transcriptional regulation of the MBL2 gene. This finding was further confirmed by a competition assay using a −554G probe. The candidate transcription factor AP-1, which was suggested by the transcription factor database, also competed specifically with the −554G band. This finding indicates that the −554G allele may bind with the transcription factor AP-1 for transcriptional regulation of the MBL2 promoter, whereas the −554C allele binds weakly, producing less significant transcriptional regulation. Transcription factor AP-1 is well known as a redox-sensitive transcription factor, and it can be activated by oxidative stress in inflammatory diseases.43, 44, 45 In our previous study, we have shown that serum MBL levels in asthmatics are significantly higher compared with healthy non-asthmatics; however, there are no significant differences in genotype and haplotype frequencies between these groups.21 MBL levels have been reported to be elevated in individuals with inflammatory disease compared with healthy controls, suggesting that increased MBL levels in asthmatics might be an acute response to inflammation.46 However, in the present study, there were no marked differences in serum MBL levels between the DI-OA patients and NCs, which might have been due to the high prevalence of ht2 [CAG] in the DI-OA group, causing the low expression of MBL2.
In the present study, endogenous expression of MBL2 was limited only to the Hep3B cells. A previous functional study performed using various tissues has concluded that MBL2 transcription is limited to liver tissue. In addition, extra-hepatic transcription of MBL2 can be detected in the small intestine and cord blood at low mRNA levels, and MBL2 mRNA is not detected in human mononuclear cells. This study has several limitations. There was a small number of study subjects in each group. Although ROS have been widely considered as important mediators of DI-OA, data are lacking for the determination of the role of ROS in DI-OA. The presence of MBL in the bronchoalveolar lavage fluid of asthmatic patients has been previously reported; however, there is a lack of data regarding DI-OA subjects.14 Another limitation of this study is the weak association between ht2 [CAG] distribution and serum MBL levels. Although we identified a significantly higher ht2 [CAG] frequency in the patients with DI-OA, no differences in serum MBL levels were observed in the patients with ht2 [CAG] distribution. Therefore, further studies are required to elucidate the functional role of MBL2 in the pathogenesis of DI-OA.
In conclusion, reduced serum MBL levels caused by genetic variants of MBL2 could lead to enhanced susceptibility to DI-OA. Low serum MBL levels may fail to neutralize the detrimental effects of oxidative stress due to DI exposure, which may contribute to the development of DI-OA.
References
Vandenplas O . Occupational asthma: etiologies and risk factors. Allergy Asthma Immunol Res 2011; 3: 157–167.
Wisnewski AV, Redlich CA . Recent developments in diisocyanate asthma. Curr Opin Allergy Clin Immunol 2001; 1: 169–175.
Fisseler-Eckhoff A, Bartsch H, Zinsky R, Schirren J . Environmental isocyanate-induced asthma: morphologic and pathogenetic aspects of an increasing occupational disease. Int J Environ Res Public Health 2011; 8: 3672–3687.
Park HS, Nahm DH . Isocyanate-induced occupational asthma: challenge and immunologic studies. J Korean Med Sci 1996; 11: 314–318.
Palikhe NS, Kim JH, Park HS . Biomarkers predicting isocyanate-induced asthma. Allergy Asthma Immunol Res 2011; 3: 21–26.
Mapp CE, Boschetto P, Zocca E, Milani GF, Pivirotto F, Tegazzin V et al. Pathogenesis of late asthmatic reactions induced by exposure to isocyanates. Bull Eur Physiopathol Respir 1987; 23: 583–586.
Park HS, Cho SH, Hong CS, Kim YY . Isocyanate-induced occupational asthma in far-east Asia: pathogenesis to prognosis. Clin Exp Allergy 2002; 32: 198–204.
Shin YS, Kim MA, Pham LD, Park HS . Cells and mediators in diisocyanate-induced occupational asthma. Curr Opin Allergy Clin Immunol 2013; 13: 125–131.
Dworski R, Roberts LJ 2nd, Murray JJ, Morrow JD, Hartert TV, Sheller JR . Assessment of oxidant stress in allergic asthma by measurement of the major urinary metabolite of F2-isoprostane, 15-F2t-IsoP (8-iso-PGF2alpha). Clin Exp Allergy 2001; 31: 387–390.
Yucesoy B, Johnson VJ, Lummus ZL, Kissling GE, Fluharty K, Gautrin D et al. Genetic variants in antioxidant genes are associated with diisocyanate-induced asthma. Toxicol Sci 2012; 129: 166–173.
Dozor AJ . The role of oxidative stress in the pathogenesis and treatment of asthma. Ann N Y Acad Sci 2010; 1203: 133–137.
Collard CD, Vakeva A, Morrissey MA, Agah A, Rollins SA, Reenstra WR et al. Complement activation after oxidative stress: role of the lectin complement pathway. Am J Pathol 2000; 156: 1549–1556.
Collard CD, Montalto MC, Reenstra WR, Buras JA, Stahl GL . Endothelial oxidative stress activates the lectin complement pathway: role of cytokeratin 1. Am J Pathol 2001; 159: 1045–1054.
Fidler KJ, Hilliard TN, Bush A, Johnson M, Geddes DM, Turner MW et al. Mannose-binding lectin is present in the infected airway: a possible pulmonary defence mechanism. Thorax 2009; 64: 150–155.
Tran HB, Ahern J, Hodge G, Holt P, Dean MM, Reynolds PN et al. Oxidative stress decreases functional airway mannose binding lectin in COPD. PLoS ONE 2014; 9: e98571.
Rantala A, Lajunen T, Juvonen R, Bloigu A, Silvennoinen-Kassinen S, Peitso A et al. Mannose-binding lectin concentrations, MBL2 polymorphisms, and susceptibility to respiratory tract infections in young men. J Infect Dis 2008; 198: 1247–1253.
Krug N, Tschernig T, Erpenbeck VJ, Hohlfeld JM, Kohl J . Complement factors C3a and C5a are increased in bronchoalveolar lavage fluid after segmental allergen provocation in subjects with asthma. Am J Respir Crit Care Med 2001; 164: 1841–1843.
Guo N, Mogues T, Weremowicz S, Morton CC, Sastry KN . The human ortholog of rhesus mannose-binding protein-A gene is an expressed pseudogene that localizes to chromosome 10. Mamm Genome 1998; 9: 246–249.
Garred P, Larsen F, Seyfarth J, Fujita R, Madsen HO . Mannose-binding lectin and its genetic variants. Genes Immun 2006; 7: 85–94.
Heitzeneder S, Seidel M, Forster-Waldl E, Heitger A . Mannan-binding lectin deficiency - Good news, bad news, doesn't matter? Clin Immunol 2013; 143: 22–38.
Bae SJ, Kim SH, Losol P, Yang EM, Park HS . Mannose-binding lectin 2 gene polymorphisms affect serum mannose-binding lectin levels in adult asthmatics. Ann Allergy Asthma Immunol 2013; 111: 71–73.
Kim SH, Cho BY, Park CS, Shin ES, Cho EY, Yang EM et al. Alpha-T-catenin (CTNNA3) gene was identified as a risk variant for toluene diisocyanate-induced asthma by genome-wide association analysis. Clin Exp Allergy 2009; 39: 203–212.
Ye YM, Kim CW, Kim HR, Kim HM, Suh CH, Nahm DH et al. Biophysical determinants of toluene diisocyanate antigenicity associated with exposure and asthma. J Allergy Clin Immunol 2006; 118: 885–891.
Palikhe NS, Kim SH, Cho BY, Ye YM, Choi GS, Park HS . Genetic variability in CRTH2 polymorphism increases eotaxin-2 levels in patients with aspirin exacerbated respiratory disease. Allergy 2010; 65: 338–346.
Kim SH, Son JK, Yang EM, Kim JE, Park HS . A functional promoter polymorphism of the human IL18 gene is associated with aspirin-induced urticaria. Br J Dermatol 2011; 165: 976–984.
Grievink L, Smit HA, Ocke MC, Veer VP, Kromhout D . Dietary intake of antioxidant (pro)-vitamins, respiratory symptoms and pulmonary function: the MORGEN study. Thorax 1998; 53: 166–171.
Terada LS . Specificity in reactive oxidant signaling: think globally, act locally. J Cell Biol 2006; 174: 615–623.
Zuo L, Otenbaker NP, Rose BA, Salisbury KS . Molecular mechanisms of reactive oxygen species-related pulmonary inflammation and asthma. Mol Immunol 2013; 56: 57–63.
Adcock IM, Brown CR, Kwon O, Barnes PJ . Oxidative stress induces NF kappa B DNA binding and inducible NOS mRNA in the human epithelial cell line A549. Biochem Soc Trans 1994; 22: 186S.
Sen CK, Packer L . Antioxidant and redox regulation of gene transcription. FASEB J 1996; 10: 709–720.
Hogaboam CM, Takahashi K, Ezekowitz RA, Kunkel SL, Schuh JM . Mannose-binding lectin deficiency alters the development of fungal asthma: effects on airway response, inflammation, and cytokine profile. J Leukoc Biol 2004; 75: 805–814.
Aittoniemi J, Soranummi H, Rovio AT, Hurme M, Pessi T, Nieminen M et al. Mannose-binding lectin 2 (MBL2) gene polymorphism in asthma and atopy among adults. Clin Exp Immunol 2005; 142: 120–124.
Kaur S, Gupta VK, Shah A, Thiel S, Sarma PU, Madan T . Elevated levels of mannan-binding lectin (MBL) and eosinophilia in patients of bronchial asthma with allergic rhinitis and allergic bronchopulmonary aspergillosis associate with a novel intronic polymorphism in MBL. Clin Exp Immunol 2006; 143: 414–419.
Ip WK, Takahashi K, Ezekowitz RA, Stuart LM . Mannose-binding lectin and innate immunity. Immunol Rev 2009; 230: 9–21.
Redlich CA, Karol MH . Diisocyanate asthma: clinical aspects and immunopathogenesis. Int Immunopharmacol 2002; 2: 213–224.
Brannan JD, Lougheed MD . Airway hyperresponsiveness in asthma: mechanisms, clinical significance, and treatment. Front Physiol 2012; 3: 460.
Holgate ST . Mechanisms of asthma and implications for its prevention and treatment: a personal journey. Allergy Asthma Immunol Res 2013; 5: 343–347.
Park HS, Lee SK, Lee YM, Kim SS, Nahm DH . Longitudinal study of specific antibodies to toluene diisocyanate (TDI)-human serum albumin (HSA) conjugate in patients with TDI-induced asthma. Korean J Intern Med 2002; 17: 249–251.
Oettgen HC, Geha RS . IgE regulation and roles in asthma pathogenesis. J Allergy Clin Immunol 2001; 107: 429–440.
Mishra PK, Khan S, Bhargava A, Panwar H, Banerjee S, Jain SK et al. Regulation of isocyanate-induced apoptosis, oxidative stress, and inflammation in cultured human neutrophils: isocyanate-induced neutrophils apoptosis. Cell Biol Toxicol 2010; 26: 279–291.
Mishra PK, Panwar H, Bhargava A, Gorantla VR, Jain SK, Banerjee S et al. Isocyanates induces DNA damage, apoptosis, oxidative stress, and inflammation in cultured human lymphocytes. J Biochem Mol Toxicol 2008; 22: 429–440.
Hodge S, Matthews G, Dean MM, Ahern J, Djukic M, Hodge G et al. Therapeutic role for mannose-binding lectin in cigarette smoke-induced lung inflammation? Evidence from a murine model. Am J Respir Cell Mol Biol 2010; 42: 235–242.
Hsu TC, Young MR, Cmarik J, Colburn NH . Activator protein 1 (AP-1)- and nuclear factor kappaB (NF-kappaB)-dependent transcriptional events in carcinogenesis. Free Radic Biol Med 2000; 28: 1338–1348.
Karin M, Takahashi T, Kapahi P, Delhase M, Chen Y, Makris C et al. Oxidative stress and gene expression: the AP-1 and NF-kappaB connections. Biofactors 2001; 15: 87–89.
Surh YJ, Kundu JK, Na HK, Lee JS . Redox-sensitive transcription factors as prime targets for chemoprevention with anti-inflammatory and antioxidative phytochemicals. J Nutr 2005; 135: 2993S–3001S.
Schafranski MD, Stier A, Nisihara R, Messias-Reason IJ . Significantly increased levels of mannose-binding lectin (MBL) in rheumatic heart disease: a beneficial role for MBL deficiency. Clin Exp Immunol 2004; 138: 521–525.
Acknowledgements
This research was supported by a grant from the Korea Health Technology R&D project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (HI14C0065).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kim, SH., Bae, SJ., Palikhe, S. et al. Effects of MBL2 polymorphisms in patients with diisocyanate-induced occupational asthma. Exp Mol Med 47, e157 (2015). https://doi.org/10.1038/emm.2015.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/emm.2015.10
This article is cited by
-
Association of MBL2 gene polymorphisms and MBL levels with dilated cardiomyopathy in a Chinese Han population
BMC Medical Genomics (2024)
-
Identification of potential urine proteins and microRNA biomarkers for the diagnosis of pulmonary tuberculosis patients
Emerging Microbes & Infections (2018)
-
Association of the miR-196a2, miR-146a, and miR-499 Polymorphisms with Asthma Phenotypes in a Korean Population
Molecular Diagnosis & Therapy (2017)