Abstract
For patients with unexplained or undiagnosed conditions, genomic sequencing offers the hope of resolving unanswered questions. With the growth of clinical genomic sequencing, understanding factors that shape patients’ hope for information could have important implications for developing patient education guidelines. Based on the goal-directed theory of hope, we investigated illness uncertainty as a form of motivation and subjective social status as a form of perceived resources to predict the amount and kinds of information that adult patients (N=191) and parents of pediatric patients (N=79) hoped to receive from diagnostic sequencing results. Participants were part of a larger longitudinal study on clinical genomic sequencing, but the current study focuses on their hopes for diagnostic sequencing results. Hopes for information were assessed through close-ended and open-ended responses. Findings from mixed methods analyses indicated that although patients and parents hoped to learn multiple kinds of information from diagnostic sequencing results, their hopes appeared to be influenced by their illness uncertainty and perceptions of their social and economic resources. These findings suggest that patients’ illness uncertainty and perceived resources could be useful avenues for discussing patient hopes and educating patients about strengths and limitations of genomic sequencing.
Similar content being viewed by others
INTRODUCTION
For patients with serious illnesses, hope provides a sense of meaning and stability and enables a positive outlook.1, 2 For unexplained or undiagnosed illnesses, diagnostic genomic sequencing increases the likelihood of detecting a genetic explanation or diagnosis that could help identify treatments and disease risk for family members.3 Yet, uncertainty about the health implications of results will likely persist due to current limitations in scientific and clinical knowledge and sequencing technology.3 Prior studies reveal that at-risk adults, patients, and parents of pediatric patients hope to learn different kinds of information from diagnostic genomic sequencing results (eg, genetic cause, treatment).4, 5, 6 One key question that has not been addressed is why patients hope for different kinds of information. Understanding factors that shape patient hope could inform the development of patient education and counseling approaches that foster hope in ways that acknowledge the strengths and limitations of genomic sequencing.
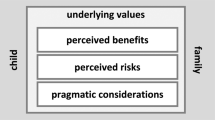
One way to understand factors that shape patient hopes is to apply a theoretical framework that takes into account the personal, interpersonal, and environmental resources that are posited to influence hope.7 The goal-directed theory of hope proposes that hope is shaped by people’s motivation to pursue a desired outcome (ie, a goal) and their perceived means to do so.8, 9 Those with more motivation and perceived means are posited to have more hope than those with less motivation or perceived means. Given the salience of uncertainty and resource demands (eg, the money, time, and social resources for pursuing medical resolution) in patients with unexplained or undiagnosed conditions, the present study investigated illness uncertainty as a form of motivation and subjective social status as a form of perceived means to predict patients’ hopes for information from diagnostic sequencing results.
Illness uncertainty – the inability to explain the cause of an illness, define an illness, or make predictions about future health10, 11 – can undermine health-related decision making and psychological adjustment.12, 13 Such barriers posed by illness uncertainty may increase patient motivation to learn more information from sequencing results. In addition, people’s perceptions of their social and economic resources could shape their views of genomic sequencing and its health implications. People’s views of their social status in terms of education, finances, and occupational prestige (ie, subjective social status14) may influence how they see themselves, others, and their situations.15 Subjective social status has been linked to mental and physical health above and beyond objective indicators of socioeconomic status such as education and income.16 By extrapolation, patients who see themselves as better resourced may feel more hopeful about diagnostic genomic sequencing because they see more possibilities to apply results to health decisions and medical resolution of health concerns than patients who see themselves as less resourced.
Current study
We investigated the effects of illness uncertainty and subjective social status on the number of kinds of information (eg, genetic explanation, diagnosis, treatment) that adult patients and parents of pediatric patients hoped to learn from their (or their child’s) diagnostic whole-exome sequencing (WES). Patients and parents were part of an ongoing longitudinal study that is investigating the feasibility of applying genomic sequencing to clinical care. The current study focuses on participant hopes for information from diagnostic sequencing results. To obtain a nuanced understanding of the nature of participants’ hopes, content analysis was performed on their open-ended responses about their main hope for information from WES. Based on the goal-directed theory of hope,9 we hypothesized that more illness uncertainty and a higher subjective social status would be associated with participants hoping for more kinds of information.
MATERIALS AND METHODS
Participants
Adult patients (N=191) and the parents of pediatric patients (N=79) were participating in the North Carolina Clinical Genomic Evaluation of Next-generation Exome Sequencing study (NCGENES). Patients are referred to NCGENES by physicians associated with the University of North Carolina (Chapel Hill, NC, USA) and Vidant Medical System (Greenville, NC, USA). Patients are eligible for NCGENES when they have a condition that is suspected to have a genetic cause but has not been definitively explained or diagnosed. Of the eligible patients (or parents of pediatric patients) contacted for study participation as of June 2014 (N=724), 347 enrolled (46.9%). Common reasons for non-enrollment include inability to reach for scheduling (N=119), participant cancellation of clinic visits or no-shows (N=72), or participant refusal to participate owing to lack of interest or time or poor health (N=55).
Procedures
All participants completed telephone surveys and mail-in questionnaires approximately 2 weeks after study enrollment (Time 1) and approximately 2 weeks after receiving diagnostic WES results (Time 2). Adult patients completed additional telephone surveys approximately 3 and 6 months after receiving results. Telephone surveys are audio recorded, and all data are entered in an electronic data storage system (Research Electronic Data Capture, REDCap). Participants provided written consent before participation. All procedures were approved by the Institutional Review Boards of the University of North Carolina, Chapel Hill and Vidant Medical System. The current study is based on Time 1 telephone surveys completed between September 2012 and June 2014.
Measures
Illness uncertainty was assessed during the telephone survey using the 23-item Illness Uncertainty Scale,17 which assesses agreement with statements about cause, ability to define or characterize the illness, and future health implications on a 5-point scale, 1 (strongly disagree) to 5 (strongly agree). Scale scores followed a normal distribution (skewness=−0.07; kurtosis=−0.92), and the scale demonstrated acceptable reliability (α=0.91). Subjective social status was assessed in a mail-in questionnaire using the Subjective SES Scale,14 which is an image of a ladder with 10 rungs, with the lowest rung indicating people in the United States with the worst resources (money, education, jobs) and the highest rung indicating people with the best resources. Participants are instructed to mark one rung on the ladder that corresponds with their sense of social status. Subjective social status score followed a normal distribution (skewness=−0.24; kurtosis=−0.24).
Hopes for information from WES results
Participant hopes for information from their (or their child’s) diagnostic WES results were assessed in the telephone survey through: (1) a close-ended item and (2) an open-ended item about the main thing they hoped to get from results.
The close-ended item was, ‘I’d like to start by reading a list of things people sometimes hope to get out of their [child’s] whole exome sequencing and genetic counseling. As I read the list, I’d like you to tell me whether you are hoping to get each of these things out of your [child’s] whole exome sequencing and the genetic counseling you’ll get with it.’ Participants endorsed (yes/no) to the following: ‘An explanation for your [child’s] health concern?’; ‘Reassurance, or information to reduce your concerns?’; ‘Advice on how to manage your [child’s] health concern?’; and ‘Help making treatment decisions?’. Participants could also name something else they were hoping to get. One-quarter of participants (n=68) named an additional unique item, including information about disease risk for family members and future health, helping others, and helping advance genomic medicine. The endorsed items (including unique items named by participants) were summed to create a score for the number of kinds of information participants hoped to get. Scores followed a fairly normal distribution (skewness=−1.34; kurtosis=2.21). The open-ended item was, ‘In your own words, what is the main thing you hope to get out of your [child’s] whole exome sequencing and genetic counseling?’
Analyses
The number of kinds of information participants hoped to learn
Hierarchical linear regression was performed to investigate illness uncertainty and subjective social status as predictors of the number of kinds of information that participants hoped to learn. To control for potential influences of participants’ background and experiences, prior genetic testing, respondent role (adult patient vs parent), race/ethnicity (non-Hispanic white vs other ethnicity/race combinations), and patient functional status (standardized scores for adults18, 19 and pediatric patients20) were entered as covariates in the first block. Because of the potential overlap between objective socioeconomic status and race/ethnicity, educational attainment (less than college degree vs college degree or higher) and total household income (continuous) were entered separately in the second block. Illness uncertainty and subjective social status were entered in the third block to assess their effects above and beyond control variables, including education and income. Power calculations for a sample size that takes into account missing data on covariates (N~240), a small-to-moderate effect size, and statistical significance at P=0.0521 indicated sufficient statistical power (>0.95).
The main thing participants hoped to learn
Content analysis was conducted on participants’ open-ended responses. The first two authors (CMK and EGM) separately noted response patterns of the first 105 participants and came to an agreement about major themes to include in a codebook as distinct codes (eg, cause, future implications; Table 3). Participants who mentioned several items in their responses were assigned multiple codes. Next, the second (EGM) and third (CL) authors applied the codebook to separately conduct content analysis for the first 125 participant responses. Across two separate coding sessions, the inter-rater agreements (kappas) for coded responses ranged from 0.73 to 0.80 for the first coding session and from 0.69 to 0.72 for the second session before discussion of coding disagreements. Disagreements were settled by CMK. Given high inter-rater agreement, responses of remaining participants (N=144) were coded by EGM or CL. Questions about coding were resolved among CMK, EGM, and CL. For participants who completed the subjective social status item (N=260), coded responses were stratified by low status (scores 1–3), moderate status (scores 4–7), and high status (scores 8–10). Status cutoffs were chosen to obtain a clearer differentiation of high status and low status and used as a three-category status variable to investigate emergent themes in responses.
RESULTS
The number of kinds of information participants hoped to learn
Demographic and study variable information are presented in Table 1. On average, participants endorsed hoping to learn 3.87 (SD=1.02) kinds of information. Findings for illness uncertainty and subjective social status were in line with predictions (Table 2). As participants’ illness uncertainty increased, they hoped for more kinds of information from WES (β=0.29, P<0.001). A marginal effect emerged for subjective social status such that as participants’ subjective social status increased they hoped for marginally more kinds of information (β=0.14, P=0.077). Illness uncertainty and subjective social status accounted for an additional 7.0% of the variance above and beyond control variables, including education and income (Adj. R2=0.12; F change P<0.001).
The main thing participants hoped to get
Content analysis of participants’ open-ended responses (N=269) generated 10 distinct codes for information. As shown in Table 3, participants most commonly mentioned the following kinds of information as a ‘main hope’: Cause of the illness (‘cause’; 44.2%); directions for illness management (‘treatment’; 36.4%); identity or name for the illness (‘diagnosis’; 26.8%); and disease risk for family members (‘family implications’; 23.0%). Other items such as implications for future health (‘future implications’), illness prevention (‘prevention’), or implications for having children (‘family planning’) were mentioned by relatively few participants (≤12%). Smaller percentages of participants hoped that their results would benefit others (‘help others’) and advance research (‘advance science’). Over half (54.1%) of the participants mentioned more than one kind of information in their response.
Emergent themes in the kinds of information that participants mentioned as a main hope and the language used to describe main hopes were observed across social statuses. The majority (57.1%) of low-status participants (N=28) mentioned hoping to get information about the cause of the illness. Moderate-status participants (N=180) were fairly broad in their main hopes, with over one-third hoping to get information about the genetic cause (39.4%) or treatment for the illness (39.4%) and over one-quarter (29.4%) hoping to get a diagnosis. Nearly half of the high-status participants (N=51) hoped to get information about the cause of the illness (49.0%) or information about disease risk in family members (41.2%).
A small subset of participants mentioned hoping to learn both the cause of the illness and receive a diagnosis: 5 (17.9%) low-status participants, 11 (6.1%) moderate-status participants, and 1 high-status participant. Although content analysis of this small subset of participant responses precludes strong conclusions, we observed a tendency of moderate-status participants to qualify their hopes with words such as ‘maybe’ or ‘possible’ relative to low-status participants. For example, one low-status adult patient said, ‘I hope to get an answer to what has been affecting my vision and what exactly I have’. A moderate-status parent tempered her hope by saying, ‘To know what happened that caused him to have this disorder that he has. If possible, to know what exactly his diagnosis is’.
Follow-up hierarchical logistic regression analyses were conducted to investigate the effects of illness uncertainty and subjective social status (status category variable) on whether or not participants mentioned the four most common types of information as a main hope: cause, treatment, diagnosis, and family implications. These analyses controlled for participant role, prior genetic testing, race/ethnicity, patient functional status, educational attainment, and household income.
Cause
Participants’ illness uncertainty was not significantly associated with the odds of mainly hoping to learn the cause (P=0.927). However, low-status participants were more likely to mention cause than moderate-status participants (OR=3.34; 95% CI=1.30, 8.60; P=0.012).
Treatment
As participants’ illness uncertainty increased, their odds of mainly hoping to learn about treatment increased by 4.90 (95% CI=2.63, 9.12; P<0.001). There were no significant differences in the odds of mentioning treatment across status categories (Ps>0.200).
Diagnosis
As participants’ illness uncertainty increased, their odds of mainly hoping to receive a diagnosis increased by 6.51 (95% CI=3.12, 13.59; P<0.001). Low-status participants were marginally more likely to mention diagnosis than high-status participants (OR=4.49; 95% CI=0.98, 20.56; P=0.053). Moderate-status participants were marginally more likely to mention diagnosis than high-status participants (OR=3.13; 95% CI=0.98, 10.04; P=0.055).
Family implications
As participants’ illness uncertainty increased, their odds of mainly hoping to learn about disease risk in family members decreased by over one-half (OR=0.44; 95% CI=0.24, 0.81; P=0.008). There were no significant differences in the odds of mentioning family implications as a main hope across status categories (Ps>0.100).
DISCUSSION
Patients and parents of pediatric patients in the current study were hoping to learn multiple kinds of information from WES results. In line with the psychosocial and practical challenges of living with an unexplained or undiagnosed condition, participants’ descriptions of their main hopes were largely aimed at receiving an explanation for the illness, information about treating it, a diagnosis (ie, a name or label for the condition), and information about disease risk in family members. These findings are similar to those found for oncology patients5 and parents of pediatric patients with rare conditions6 but are unlike findings for adults at risk for coronary artery disease whose hopes to help others or advance medical science figured more prominently.4 Such similarities and differences from prior research suggest that how people prioritize hopes for genomic sequencing may vary by health context. In line with the goal-directed theory of hope,8, 9 participants’ uncertainty about their (or their child’s) illness and, to a lesser extent, their subjective social status appeared to influence how much and what kinds of information they hoped to learn from WES.
Patients and parents who felt uncertain about the cause, nature, and/or future implications of their (or their child’s) illness hoped for more kinds of information than those who felt less uncertain. Thus, illness uncertainty may be a key motivator to have diagnostic sequencing by shaping how patients view the range of benefits from sequencing information. Findings also suggested that illness uncertainty influences what kinds of information patients hope to learn. When patients are unsure of the identity of their illness or are unsure of how to treat it, they may focus their hopes for WES on themselves. By contrast, when patients have a better understanding of their illness, they may hope to learn if their family members are at risk to help their family members prepare for the possibility of future illness.
Subjective social status was marginally linked to the amount of information patients and parents hoped to learn from WES; however, findings revealed differences in the kinds of information that they were mainly hoping to learn. Participants from all subjective social status groups hoped to learn the cause of their illness, but the breadth of additional hopes mentioned varied across status groups. Low-status participants were overwhelmingly hoping to learn the cause of their illness, whereas the hopes of moderate-status participants appeared more varied. The hopes of high-status participants more narrowly focused on hoping to learn the cause of their illness and information about disease risk in family members. Thus patients’ perceptions of their social and economic resources may shape their priorities for information from sequencing results.
Findings also raise the question of how to encourage realistic hopes and downplay unrealistic hopes for genomic sequencing. Some patients and families may hope for more information than genomic sequencing can feasibly provide at this time. Unrealistic hopes may needlessly predispose patients and families to greater distress when hopes for sequencing results are inevitably unmet. Poor health literacy and numeracy,22 unfamiliarity with genetics terminology and patterns of inheritance,23 and inevitable shifts in interpretation and return of results with advances in genomic medicine24, 25 complicate the communication of strengths and limitations of genomic sequencing. Taking into account patients’ level of illness uncertainty and perceived resources could inform the development of guidelines for provider communication by helping providers ascertain patients’ frame of reference for their hopes. It could also inform the development of educational resources that help patients clarify their priorities and make informed decisions.
Limitations and future directions
The current study extends prior research on people’s hopes for genomic sequencing4, 5, 6 by investigating predictors of hope in adult patients and parents of pediatric patients in a real-world, clinical setting. The hopes of patients and parents reflected personally relevant information that could potentially influence their psychological well-being, beliefs about the condition, and subsequent health decisions. Nonetheless, study limitations remain that could serve as future research directions.
One limitation is that patients’ and parents’ hopes were based on one time point. Whereas some have suggested that being hopeful is a relatively stable individual difference,8, 9 others have suggested that patients’ hopes can change as a function of adaptation to an illness.2 Although patients’ and parents’ hopes for information from WES and genetic counseling were assessed through close-ended and open-ended questions, our methods for measuring and coding hope may not have fully captured the entire scope of the emotional26 and cognitive9 aspects of hope. Findings from the exploratory content analysis of the dual hopes for cause and diagnosis should be interpreted for the purpose of hypothesis generation in future research. It is also unclear whether patients and parents distinguished their hopes for WES from genetic counseling. For instance, participants may have hoped that WES results could elucidate a cause, but they may have hoped that genetic counseling would provide reassurance. Finally, participants’ hopes for WES may be driven by other forms of motivation or perceived means. For example, participants could also be motivated by personal beliefs about their illness or family history. Participants’ perceptions of their means to use information from WES could also be influenced by access to health-care providers or insurance coverage.
For patients grappling with an unexplained or difficult-to-diagnose condition, hope is an important resource for psychological well-being and resilience. The growth of clinical sequencing will necessitate finding ways to foster patients’ hope while also educating them about the limitations of diagnostic sequencing. Understanding why patients hope for certain information could help providers tailor their communication and inform the development of educational resources that enable informed decisions surrounding genomic sequencing and its applications to health care.
References
Nekolaichuk CL, Jevne RF, Maguire TO : Structuring the meaning of hope in health and illness. Soc Sci Med 1999; 48: 591–605.
Soundy A, Smith B, Dawes H, Pall H, Gimbrere K, Ramsay J : Patients’ expression of hope and illness narratives in three neurological conditions: a meta-ethnography. Health Psychol Rev 2013; 7: 177–201.
Facio FM, Lee K, O’Daniel JM : A genetic counselor’s guide to using next-generation sequencing in clinical practice. J Genet Couns 2014; 23: 455–462.
Facio FM, Brooks S, Loewenstein J, Green S, Biesecker LG, Biesecker BB : Motivators for participation in a whole-genome sequencing study: implications for translational genomics research. Eur J Hum Genet 2011; 19: 1213–1217.
Miller FA, Hayeems RZ, Bytautas JP et al: Testing personalized medicine: patient and physician expectations of next-generation genomic sequencing in late-stage cancer. Eur J Hum Genet 2014; 22: 391–395.
Sapp JC, Dong D, Stark C et al: Parental attitudes, values, and beliefs toward the return of results from exome sequencing in children. Clin Genet 2014; 85: 120–126.
Schrank B, Bird V, Rudnick A, Slade M : Determinants, self-management strategies and interventions for hope in people with mental disorders: systematic search and narrative review. Soc Sci Med 2012; 74: 554–564.
Snyder CR : Current trends: conceptualizing, measuring, and nurturing hope. J Couns Dev 1995; 73: 355–360.
Snyder CR, Harris C, Anderson JR et al: The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 1991; 60: 570–585.
Han PKJ, Klein WMP, Arora NK : Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making 2011; 31: 828–838.
Mishel MH : Reconceptualization of the uncertainty in illness theory. J Nur Scholarship 1990; 22: 256–262.
Hamilton JG, Hutson SP, Moser RP et al: Sources of uncertainty and their association with medical decision making: exploring mechanisms in Fanconi anemia. Ann Behav Med 2013; 46: 204–216.
Johnson Wright J, Afari N, Zautra A : The illness uncertainty concept: a review. Curr Pain Headache Rep 2009; 13: 133–138.
Adler NE, Epel ES, Catellazzo G, Icovics JR : Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women. Health Psychol 2000; 19: 586–592.
McLeod JD, Lively KJ : Social structure and personality; In: Delamater J (ed): Handbook of Social Psychology. New York, USA: Kluwer Academic/Plenum, 2003, ch 4, pp 77–102.
Singh-Manoux A, Marmot MG, Adler NE : Does subjective social status predict health and change in health status better than objective status? Psychosom Med 2005; 67: 855–861.
Mishel MH : The measurement of uncertainty in illness. Nurs Res 1981; 30: 258–263.
Wingard JR, Curbow B, Baker F, Piantadosi S : Health, functional status, and employment of adult survivors of bone marrow transplantation. Ann Intern Med 1991; 114: 113–118.
Karnofsky DA, Abelman WH, Craver LF, Burchenal JH : The use of the nitrogen mustards in the palliative treatment of carcinoma. Cancer 1948; 1: 634–656.
Lewis CC, Pantell RH, Kieckhefer GM : Assessment of Children's Health Status: Field Test of New Approaches. Medical Care, Vol. 27, No. 3, Supplement: Advances in Health Status Assessment: Conference Proceedings 1989, pp S54–S65.
Cohen J, Cohen P, West SG, Aiken LS : Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Mahwah, NJ, USA: Lawrence Erlbaum, 2003, pp 181.
Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW : Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics 2011; 14: 279–289.
Condit CM : Public understandings of genetics and health. Clin Genet 2010; 77: 1–9.
Berg JS, Khoury MJ, Evans JP : Deploying whole genome sequencing in clinical practice and public health: meeting the challenge one bin at a time. Genet Med 2011; 13: 499–504.
Green RC, Berg JS, Grody WW et al: (2013). ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Gen Med 2014; 15: 565–574.
Averill JR, Sundararajan L : Hope as rhetoric: cultural narratives of wishing and coping; in Eliott J (ed): Interdisciplinary Perspectives on Hope. Hauppauge, NY, USA: Nova Science, 2004, pp 127–159.
Acknowledgements
Research reported in this publication was supported by the National Human Genome Research Institute of the National Institutes of Health under award number U01HG006487. Principal Investigators: James P Evans, Jonathan S Berg, Karen E Weck, Kirk C Wilhelmsen, and Gail E Henderson. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Dr Gail E Henderson for feedback on previous drafts and Dr Debra Skinner for guidance on content analysis and feedback on previous drafts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Khan, C., Moore, E., Leos, C. et al. Patient hopes for diagnostic genomic sequencing: roles of uncertainty and social status. Eur J Hum Genet 24, 803–808 (2016). https://doi.org/10.1038/ejhg.2015.204
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2015.204
This article is cited by
-
Known unknowns: building an ethics of uncertainty into genomic medicine
BMC Medical Genomics (2016)