Abstract
Sex chromosome trisomies (SCTs) are frequently diagnosed, both prenatally and postnatally, but the highly variable childhood outcomes can leave parents at a loss on whether, when and how to disclose genetic status. In two complementary studies, we detail current parental practices, with a view to informing parents and their clinicians. Study 1 surveyed detailed qualitative data from focus groups of parents and affected young people with either Trisomy X or XYY (N=34 families). These data suggested that decisions to disclose were principally affected by the child’s level of cognitive, social and emotional functioning. Parents reported that they were more likely to disclose when a child was experiencing difficulties. In Study 2, standardised data on cognitive, social and emotional outcomes in 126 children with an SCT and 63 sibling controls highlighted results that converged with Study 1: logistic regression analyses revealed that children with the lowest levels of functioning were more likely to know about their SCT than those children functioning at a higher level. These effects were also reflected in the likelihood of parents to disclose to unaffected siblings, schools and general practitioners. In contrast, specific trisomy type and the professional category of the clinician providing the original diagnosis did not affect likelihood of disclosure. Our study emphasises the complex weighing up of costs and benefits that parents engage in when deciding whether to disclose a diagnosis.
Similar content being viewed by others
Introduction
Sex chromosome trisomies (SCT) account for around a quarter of all chromosome abnormalities diagnosed following amniocentesis.1 This places them among the most common trisomies resulting in live birth.2 XXX and XYY karyotypes are found in around 1 in 1000 live female and male births, respectively, and XXY (Klinefelter Syndrome) affect around 1.72 in 1000 live births.3, 4 Given that nearly 5% of pregnant women undergo invasive prenatal screening in the UK every year and approximately 1 child in every 160 is born with a rare chromosome disorder,5 medical practitioners need to be able to provide parents with accurate information on possible outcomes, as this may influence significant decisions.2 Yet, both parents receiving and clinicians providing a diagnosis of a SCT reported that the communication process at initial diagnosis was incredibly variable and was, in some cases, traumatic.6
Initial disclosure of diagnosis of an SCT can indeed be a problematic process, because the absence of obvious physical abnormalities means that such chromosome anomalies often remain undiagnosed, and milder or unaffected cases may not contribute to the overall prognostic picture available to practitioners. In turn, a significant portion of those who are diagnosed in childhood or later are identified owing to behavioural or educational difficulties. Consequently, research involving these populations may overrepresent problems. Indeed, some early studies influencing disclosure practices today were carried out in psychiatric and penal institutions and therefore from a highly selected population of individuals who experienced serious problems.7, 8 Unwarranted by the careful caveats posed by researchers who carried out those studies, their reporting in the press led to widespread misunderstandings about individuals with SCTs, particularly presenting males with XYY as aggressive criminals,9 whereas current evidence suggests that outcomes for these individuals are much more positive.10
Several newborn screening studies were carried out in the 1960s to investigate outcomes in children with SCTs in samples unbiased by concerns prior to referral.11, 12, 13, 14 These longitudinal studies followed children who were diagnosed perinatally with an SCT into adulthood.15 Although these studies reported educational and behavioural difficulties, they also suggested a much less gloomy outlook. A recent systematic review of findings from samples less affected by ascertainment bias indicated an IQ of up to 20 points below that of comparison groups and greater risk of neurodevelopmental disorders.10 A greater incidence of social and emotional impairments was also found, particularly in males, for whom these features were associated with autism.16 However, despite average difficulties at the group level, some individuals with a SCT function well, indicating a very varied prognosis.10, 16
With variable cognitive, emotional and behavioural prognoses, however, comes another set of issues and considerations that are problematic for disclosure: whether and when to tell the child and significant others about the diagnosis. In our previous work with these families, parents told us that this question worried them, but we could find no formal guidance or research data on disclosure in SCTs, except for a recent study focussed primarily on Klinefelter Syndrome (http://www.genetic.org/Knowledge/BooksandResources.aspx, 2014). How families approach disclosure in other conditions can be informative. Parents report considering the potential negative impact of telling on emotional wellbeing in cases of chronic illness;17 their own understanding of the condition as a barrier to disclosure;18 and the severity of the condition as a major deciding factor in whether or not to disclose.19 In these cases, disclosure is often necessary because of associated implications of severe cognitive and/or physical impairments and/or inherited risk but there could be useful parallels about how parents approach decisions about disclosure, which may have relevance in SCTs.
The current study: factors influencing parental disclosure
We hypothesised that at least three factors might influence parental decisions about disclosure of the diagnosis. First, the type of SCT and associated clinical issues might influence disclosure. For example, fertility is not thought to be affected for two of the trisomies, XXX and XYY, although there are suggestions of a link with premature ovarian failure in some with XXX.20, 21, 22 We hypothesised that there may be less pressure to inform a child with one of these karyotypes compared with Klinefelter Syndrome, XXY, where there are clinical implications that generally result in referral to an endocrinologist. Second, research suggests that information given to parents at the point of diagnosis varies considerably,6 and we therefore assessed whether this had an impact on parents’ decisions. Third, the variable phenotypes with individuals with SCTs means that parents may take into account their child’s level of language and social functioning. The relationship between the affected child’s level of functioning and the likelihood that they have been told is not yet known. On the one hand, children with language, social or emotional impairments may be more likely to know about their SCT, because it could provide a relevant explanation for difficulties. Alternatively, children without any such impairments may be disclosed to as they are more likely to understand about the condition. The degree to which children experience these difficulties may additionally provide the impetus for parents disclosing a diagnosis to their child’s school or siblings.
To investigate reasons for disclosure, we conducted a series of focus groups with parents of children with an SCT (N=34, Study 1). We combined these qualitative data with a quantitative investigation of the factors that parents consider when making a decision to disclose, using a large data set about children with an SCT (N=126) and unaffected siblings (N=63)16 (Study 2).
Methods
Study 1—Qualitative exploration of parental reports about disclosure
Design
The study underwent ethical review by the Central University Research Ethics Committees of the primary host institution. We held two Study days, one for parents who had a daughter with XXX and one for parents who had a son with XYY. Study days were organised in collaboration with Unique, the Rare Chromosome Disorder Support Group; a parental support group for individuals with rare chromosome disorders. Parents spoke about their experiences with diagnosis and how this impacted decisions to disclose to their child, siblings, schools and other family members.
Sample
A total of 34 families provided informed consent and participated in the focus groups, offering information on 12 girls with XXX and 22 boys with XYY. Participating parents spanned income brackets. Each focus group included some parents who had told their son or daughter about having an SCT as well as others who had not. This allowed us to gain information from those who had already chosen to disclose about their own experiences and also to hear from parents who were currently deciding about disclosure. Those who did not wish to participate in a focus group were invited to join a general discussion group with other parents. All quotes provided use pseudonyms.
Procedure
Team members experienced in facilitating focus groups led the exercise, adhering to published guidelines.23 Focus group facilitators were particularly geared to maintaining neutrality, to allow for the full range of views from the preference for early disclosure to the decision not to disclose until adolescence. A focus group schedule was created to facilitate discussion on the following themes: reasons for and against disclosure; the disclosure process; disclosure to siblings, other family members, schools and other health-care professionals. Consent was obtained to audio record each session, and recordings were transcribed verbatim after each Study day. Notes taken by facilitators complemented the recordings of each session. Data were coded by the first author following the principles of thematic analysis,24, 25 using a constant comparison method.
Results
Reasons for and against disclosure
For children who were most severely affected by their SCT in terms of impaired functioning, parents felt their child should know about their SCT. Parents whose children were not exhibiting signs of educational or social difficulties reported being less likely to disclose about the SCT. One parent with a 9-year-old daughter with XXX highlights the problem of unpredictable outcomes for these children in her dilemma:
“With Caroline I just think ‘I hope she’s going to be okay’. It’s that 50/50—will she/won’t she? At the moment, she’s doing fantastic. If we didn’t know about her XXX, I wouldn’t be thinking twice about ‘is she different’—I’d be thinking ‘no, she’s exactly like her brother was’. So if anyone ever said to me ‘your child has got XXX now’, I’d probably be like ‘no, you’re telling me the wrong information, she’s fine’.”
Parents who had a child who was experiencing difficulties often cited this as a key reason for disclosure. One parent with a 16-year-old daughter with XXX explains:
“I thought she should know really soon after she started school. They want to know why they can’t keep up with the others. They have got learning difficulties, or Natalie has and I just felt that she should know why she couldn’t keep up.”
The majority of parents argued that the presence of problems was a strong reason for disclosure. The point at which these became noticeable varied greatly, and this had an impact on the age at which parents chose to disclose to their children. For one parent with a 15-year-old daughter with XXX, this did not emerge until secondary school:
“There was a critical point in her understanding when she was about aged 13 or 14 and she was beginning to notice a real difference in her educational achievement and started to ask questions.”
In summary, then, many parents’ beliefs supported our hypothesis that their child’s level of functioning would have a role in parents’ willingness to disclose. Some parents had made a decision not to disclose the diagnosis to their child. There were three reasons that emerged for non-disclosure. First, some parents were concerned about stigmatisation of their child. Second, it was thought that a diagnosis may give an excuse for bad behaviour or for not trying at school. And third, some felt there was no point in raising the issue if the child had no problems: it might just cause needless anxiety. In addition to these articulated reasons for non-disclosure, there were several cases where parents felt they should disclose the diagnosis to their child but did not know how to go about this. In some cases, they felt their own poor understanding of genetics meant they would not be able to give a coherent explanation to their child.
Disclosure to siblings and other family members
When discussing disclosure to siblings, parents also relied on the level of functioning of their affected child when deciding whether or not to disclose. One parent explains why she told her son about his sister having XXX:
“We told our son when Aria was one. He started to ask why she was different, she seemed more immature than others her age, and he seemed relieved to know that there was a reason. He puts up with more from her now, before he would get frustrated but now he seems to make allowances.”
Disclosure to schools
In terms of disclosure to schools, a similar pattern emerged that those whose child had no apparent difficulties were less likely to have told the school, and those whose children required help or support due to lower levels of functioning were more inclined to disclose to the school. One parent explains that she only disclosed to the school when her son was diagnosed with learning difficulties:
“William was diagnosed with XYY because he had behavioural and development issues and once we found out I told the school straight away. I wanted them to know because he needed the help.”
When to tell: the timing of disclosure
There was no clear consensus from the participants on when the most appropriate age was to disclose about a SCT. Knowing at what age to disclose was thought to be difficult for parents as they had to balance the following arguments when deciding on the best time to disclose; when children are younger their understanding may be more limited, but they may be more accepting. However, older children may be better able to understand the complexities of the condition but may be upset to discover that information had been kept from them until now. Parents who participated in our focus groups were evenly split between these two opposing viewpoints. One parent with an 8-year-old son with XYY explained why she felt that, although she had not told her son yet, she believed early disclosure for the best:
“I don’t think it’s going to do anyone any good, shying away from it till the later years. I’ll tell him as soon as he questions the fact of ‘why’. I think it will do more damage to leave it till later years to tell somebody that they’re different from everybody else. My friend likened it to adoption; you hear so many cases where children aren’t told until they’re like mid/late teens and then they find that more catastrophic because they feel they’ve been misled. That made sense to me.”
Some parents argued that disclosure at a young age allowed for the gradual development of their child’s understanding, with the child absorbing more as they grew older, integrating it into their own personal story. For example, one parent of a 9 year-old son who has been told about having XYY, explains how she told her son:
“Throughout his childhood, I read about differences in people and not focusing on any one thing, and really focusing on things like some people have genes for blond hair, some people have genes for brown hair. So I introduced the idea of genetic difference pretty early on you know as a topic of conversation. Also I think the way that you tell them I think really makes a difference. When I told Daniel I sat down and told him ‘you know you have an extra chromosome’ and we can talk more about it and deal with our differences. Your differences might make you have problems with your behaviour but it also makes you lovely and tall. I think that’s the other thing as well because I think you have to draw on their strengths all the time.”
Other parents felt that waiting until later in the teenage years was more appropriate. One parent with a 15-year-old daughter explained why they felt it best to wait until later to tell their daughter about her XXX:
“I think it’s best to tell in the teenage years once they’ve got more genetics knowledge. It’s meaningless for the child before then. Around then, our daughter asked if there was something wrong with her. For others I would say to tell when she’s in her teens. Before then the distinction between peers isn’t too great but when they get to teenage age it becomes more apparent.”
It was apparent that in terms of disclosure to affected children, siblings and schools, parents considered their child’s level of cognitive functioning when making a decision about disclosure. Although many parents also agreed that age is a consideration, there was an underlying reliance on functioning level apparent in these choices. Parents who waited often claimed that their children were not experiencing particular difficulties at a younger age and this affected their decision making.
Study 2—Quantitative analysis of factors affecting disclosure
Common themes emerged from our qualitative exercise and are consistent with other recent work on disclosure in sex chromosomal aneuploidies,26 but group discussions can ultimately mask honest opinions. In order to limit this pitfall, experts in qualitative methods led Study 1. However, we remained critical of qualitative findings used in isolation, and this motivated us to validate them against quantitative analyses. Therefore, we made use of a large existing data set, for which findings on specific language and social cognitive outcomes have been published16, 27 but had not focussed on disclosure or the broader phenotype. We addressed the following novel issues:
-
1)
Does trisomy type have an influence on disclosure? Given fertility implications for individuals with XXY, we predicted that they would be more likely to know than others.
-
2)
Does receiving a diagnosis from a geneticist or receiving advice about disclosure at the point of diagnosis influence parents’ willingness to disclose to their child? Previous work has found that parents who see a genetic counsellor have lower termination rates post diagnosis;28, 29 we predicted that discussion with a genetics professional might also influence the willingness of parents to disclose to their child.
-
3)
Does sharing information with the affected child subsequently influence parents’ willingness to disclose to other family members, the child’s school or other professionals? If a parent has shared with their child, we predicted that they may be more open to further disclosure to others on a need-to-know basis.
-
4)
Does the affected child’s level of functioning impact on parents’ willingness to disclose? Our qualitative data from parental focus groups suggested that this would be the case.
Method
Study design
The study underwent ethical review by the National Research Ethics Service, Oxfordshire Research Ethics Committee B. Having provided informed consent, parents reported on the information received at the time of diagnosis and their subsequent decisions on disclosure to their children, family members, schools and other professionals. We also collected data on the children’s language, social and emotional functioning, behavioural difficulties and environmental and educational information using a broad range of standardised questionnaires and interviews. As the affected children may or may not have been informed about their condition, all data are from parental reports.
Sample
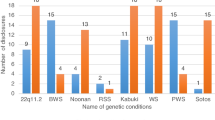
Families were identified through records of prenatal diagnoses at six regional genetics centres in England, with additional XXX and XYY cases recruited from Unique. Data were available from parents of 54 girls with XXX, 19 boys with XXY and 53 boys with XYY aged between 4 and 16 years. The lower representation of boys with XXY depends on the fact that Unique does not support families with XXY. In addition, parents provided information on disclosure to 39 male and 24 female siblings, as well as schools and general practitioners (GPs). The SCT sample was divided into two groups; Group I includes all prenatal referrals from the regional genetics centres plus additional families who joined Unique before their child’s first birthday, where there is minimal likelihood of the child’s difficulties determining diagnosis. Group II consisted of all prenatal and postnatal XXX and XYY cases who joined Unique after their child’s first birthday. This classification aims to report on children who are not identified because of difficulties.16, 27 Demographics, including maternal education, are provided in Table 1.
Background information and assessments
Four main assessments fed into this study and were administered according to standardised test instructions:
-
1)
Vineland Adaptive Behaviour Scales II30 is a structured interview administered to parents to assess a child’s daily functioning across three domains: communication (receptive, expressive and written), daily living skills (personal, domestic and community), and socialisation (interpersonal relationships, play and leisure time and coping skills). This assessment has been standardised on a US population aged from birth to 90 years.
-
2)
Children’s Communication Checklist-231 is a checklist completed by parents who rate the frequency of particular communication behaviours. There are 10 scales: four scales that assess communicative behaviours impaired in specific language impairment (SLI) and a further six that cover areas often associated with autistic disorder. This assessment has been standardised on a UK population of children aged 4–16 years.
-
3)
Strengths and Difficulties Questionnaire32 is a brief behavioural screening questionnaire that assesses children across five scales: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and pro-social behaviour. The assessment uses UK norms for children aged 4–15 years.
-
4)
Conners’ Parent Rating Scale23 is checklist completed by parents to assess childhood behavioural problems, particularly concerned with symptoms of Attention Deficit Hyperactivity Disorder and related disorders. Norms are based on an American and Canadian sample of children aged 6–18 years.
Additional information included the type of school the child attended, whether the child had been identified as having special educational needs and whether any relevant diagnosis had been made by a medical professional or psychologist. Non-standardised additional questions surrounding diagnosis are included in Supplementary Appendix A for inspection.
Results
Data were analysed using SPSS version 20 (IBM Corp., Armonk, NY, USA). Several logistic regression analyses were used to test predictors of disclosure to the affected child, siblings and schools for the 126 families involved (Table 2). Assumption of normality was tested using the Kolmogorov–Smirnov test. Vineland Socialisation and Conners’ DSM total scores violated the assumption of normality; KS(126)=0.106, P<0.05; KS(126)=0.098, P<0.05; respectively. Data transformation had no effect on outcomes, so results from analysis of untransformed data are reported. Variables with missing data are indexed by variable N.
Disclosure data
Descriptive data about family members and professionals to whom parents had disclosed is presented in Table 1. Slightly fewer of the affected children had been told than had not, over twice as many siblings had been told as had not, three-quarters of schools knew and nearly all GPs knew. When the child was aware of their diagnosis, the chances of their siblings also being aware was significantly increased, χ2 (1, N=97)=19.09, P<0.001, with the odds ratio indicating that siblings were 10.25 times more likely to know if the affected child already knew. The same was also true for the school being aware if the child was, χ2 (1, N=114)=10.85, P<0.01, with an odds ratio of 5.29, but not for GPs, for whom no significant relationship existed, χ2 (1, N=112)=0.19, P=0.57, probably owing to limited variance (the vast majority of GPs knew).
SCT type
We found no significant effect of trisomy type on disclosure.
Diagnostic factors
Receiving a diagnosis postnatally as opposed to prenatally did not significantly predict disclosure, although age of the child when parents were interviewed did. The average age at which disclosure took place did not differ across groups, F(2, 47)=2.122, P=0.131. If they were told, more than half of children were told before the age of 10 across groups, except for boys with XXY (see Table 1). We examined whether the advice and support parents received at diagnosis had an influence on their willingness to subsequently disclose. Only 17% of families reported that they had received advice. Of the 21 families who did receive advice, only 5 indicated that the advice was helpful and that they were actively told to disclose to their child. Of the remaining 16 families, 3 indicated that the advice they received was to tell for medical reasons (all 3 children had a diagnosis of Klinefelter Syndrome, XXY) and a further 5 families were discouraged from disclosure and advised not to tell their child. There was no significant relationship between advice received and parents’ decisions to disclose to their child, χ2 (1, N=117)=0.97, P=0.32. We also examined whether there was a significant difference in disclosure rates for those who were given the initial diagnosis by a geneticist as opposed to another health-care professional. Eighty-four families provided information on who delivered the initial diagnosis, but the identity of the professional providing the diagnosis did not affect the likelihood of disclosing, χ2 (1, N=84)=0.54, P=0.46. Only a quarter of the families reported receiving a diagnosis from a clinical geneticist, with the majority being informed by an obstetrician (44%) and the remaining families by an alternate health-care professional.
Child’s age, language, social and emotional functioning
Age predicted disclosure: older children were significantly more likely to know about having an SCT than younger children. Measures of language, social and behavioural impairments were highly inter-correlated. Therefore principal component analysis was conducted. Principal component analysis obtained one component with an eigenvalue of 3.86 greater than Kaiser’s criterion of 1 and this accounted for 77.2% of the variance within the sample. This component reflected all the standardised measures of language, social and behavioural functioning with similar weight and was utilised in all logistic regressions predicting the likelihood of disclosure (Table 3 and Supplementary Tables S1 and S2 for further details).
This principal component significantly accounted for disclosure to the child. Children who were performing most poorly on these measures of functioning were the most likely to be told about their SCT. Furthermore, those children whose affected siblings were the lowest functioning were also most likely to have been told about their brother or sister having a SCT. The principal component also significantly predicted whether a school was likely to have been told: schools were significantly more likely to know about the SCT for children who were doing more poorly.
Discussion
The widely varied outcomes in children with SCTs can make it hard for parents to know if, when and how to disclose to their children and others.10, 16
Although many parents had informed us that they were unsure how to make a decision about whether or not to disclose, it is clear that the families who participated in both aspects of our current study guided their decisions through consistent factors. Older children were more likely to know, but this is not surprising, given that likelihood of disclosure might simply increase with passage of time. Of note, age at which diagnosis was disclosed did not differ across diagnostic groups. This is of interest, because one may instead have predicted earlier disclosure for boys with XXY, who present with overt physical differences compared with the other groups. In fact our numerical trends pointed to later disclosure in XXY. Consistent with a recent study on disclosure in a sample composed in the main by boys with XXY, a substantial proportion of children across groups tended to be told before 11 years of age.26 Most importantly, parents considered their child’s level of functioning in order to help them reach a decision about disclosure. Parental reports from our qualitative data are undoubtedly supported by our quantitative data in suggesting that children with the lowest levels of functioning in the domains of language, social skills and emotional behaviour were significantly more likely to know about their SCT. Disclosure to the affected child was correctly predicted by his/her level of functioning in >65% of cases, in >71% of families for disclosure to siblings and in >81% of families in terms of disclosure to schools. Given the lack of clear consensus from focus groups on whether and when to disclose, it is interesting that our quantitative data instead suggest a clear role for the difficulties encountered by children as a predictor of disclosure. The fact that greater impairments were associated with higher likelihood of disclosure also highlights the urgent need for disclosure tools that are ability appropriate (http://www.genetic.org/Knowledge/BooksandResources.aspx, 2014; http://figshare.com/articles/Booklets_for_parents_and_children_XYY_and_Trisomy_X/1203560, 2014).
The quantitative data suggest that the type of medical professional providing the initial diagnosis has no subsequent effect on parents’ willingness to disclose to their child about having an SCT, and parental experiences provided in our focus groups support this, even in cases where the parents described the experience of diagnosis as traumatic. Despite evidence that receiving the diagnosis from a genetics specialist has a positive influence on lowering termination rates,28, 29 genetics professionals do not seem to influence parents in favour of disclosure. We found no evidence that receiving the initial diagnosis from a non-genetic specialist predisposed parents to non-disclosure.
Our current data set is unusual in representing both prenatally and postnatally diagnosed individuals, allowing us a view of factors affecting disclosure in a sample not influenced by the ascertainment bias associated with late diagnosis. There are reported differences between those children who received a diagnosis prenatally as opposed to postnatally, with the postnatally diagnosed children demonstrating a greater impairment in areas, including educational difficulties, rates of speech and language therapy, autistic features and motor skills.16, 27 Given this increased severity of impaired functioning in children who were diagnosed postnatally, it is therefore surprising that we did not see a difference in disclosure between these two groups. Children receiving a diagnosis postnatally received genetic testing owing to learning or behavioural difficulties, but it is clear that the variability in outcomes results in parents considering their own children’s level of functioning as a primary consideration in deciding whether or not to disclose, rather than the prenatal or postnatal diagnosis. The similarity in disclosure choices for prenatal and postnatally diagnosed children is echoed in a recent study.26 Medical professionals providing diagnoses to parents therefore need to be aware of the diversity in outcomes in order to correctly inform parents who would like to disclose diagnosis.6
Limitations
We have already highlighted caution in considering qualitative data alone, especially in the context of group discussions, and found our mixed methodological approach a strength. For pragmatic recruitment reasons, we did not investigate in as much depth the views of parents of children with XXY, in particular those receiving a postnatal diagnosis, to whom this approach should be extended. However, current common themes are also reflected in a study primarily focussed on boys with XXY:26 across the three SCTs, parents endorsed disclosing, especially if their child was more severely affected, although they also flagged concerns about how to make the conversation age and ability appropriate. Specific needs for parents of individuals with XXY need to be investigated further in a sample that represents this group better and that ideally compares it with other SCTs characterised by overt physical symptoms, such as 45,X aneuploidy, and unlike XXX or XYY.
Conclusions and clinical implications
In conclusion, our findings are clinically relevant because they evidence how the wide variability in children’s functioning in both prenatally and postnatally diagnosed individuals with an SCT drives parental decisions on disclosure. Overall, our study suggests that parents see both advantages and disadvantages of disclosure of diagnosis to their child, but the main factors determining their decision are whether or not the child is experiencing educational, emotional or behavioural difficulties, rather than the type of trisomy, the identity of the professional providing a diagnosis or guidance provided. These findings are clinically important, because they highlight the urgent need for tools helping parents deciding on whether, when and how to disclose to their child in a manner that is compatible with their child’s level of social, linguistic and cognitive functioning. International efforts are beginning to fill this gap (http://www.genetic.org/Knowledge/BooksandResources.aspx, 2014; http://figshare.com/articles/Booklets_for_parents_and_children_XYY_and_Trisomy_X/1203560, 2014), and we await eagerly data on the effectiveness of these new disclosure tools.
References
Crandall BF, Lebherz TB, Rubinstein L et al: Chromosome findings in 2500 second trimester amniocenteses. Am J Med Genet 1980; 5: 345–356.
Linden MG, Bender BG, Robinson A : Intrauterine diagnosis of sex chromosome aneuploidy. Obstet Gynecol 1996; 87: 468–475.
Jacobs PA, Melville M, Ratcliffe S, Keay AJ, Syme J : A cytogenetic survey of 11 680 newborn infants. Ann Hum Genet 1974; 37: 359–376.
Morris JK, Alberman E, Scott C, Jacobs P : Is the prevalence of Klinefelter syndrome increasing? Eur J Hum Genet 2008; 16: 163–170.
Thompson M, Thompson J, McInnis R, Willard H : Genetics in Medicine. Philadelphia, PA, USA: WB Saunders, 1991.
Abramsky L, Hall S, Levitan J, Marteau TM : What parents are told after prenatal diagnosis of a sex chromosome abnormality: interview and questionnaire study. BMJ 2001; 322: 463–466.
Jacobs P, Brunton M, Melville MM : Aggressive behaviour, mental sub-normality and the XYY male. Nature 1965; 208: 1351–1352.
Maclean N, Mitchell JM : A survey of sex-chromosome abnormalities among 4514 mental defectives. Lancet 1962; 1: 293–296.
Theilgaard A : Aggression and the XYY personality. Int J Law Psychiatry 1983; 6: 413–421.
Leggett V, Jacobs P, Nation K, Scerif G, Bishop DVM : Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Dev Med Child Neurol 2010; 52: 119–129.
Netley C : Summary overview of behavioural development in individuals with neonatally identified X and Y aneuploidy. Birth Defects Orig Artic Ser 1986; 22: 293–306.
Pennington BF, Bender B, Puck M, Salbenblatt J, Robinson A : Learning disabilities in children with sex chromosome anomalies. Child Dev 1982; 53: 1182–1192.
Ratcliffe S : Long-term outcome in children of sex chromosome abnormalities. Arch Dis Child 1999; 80: 192–195.
Theilgaard A : A psychological study of the personalities of XYY and XXY men. Acta Psychiatr Scand 1984; 69: 1–133.
Bender BG, Berch DB: Sex Chromosome Abnormalities and Human Behavior. Boulder, CO, USA: Westview Press and the American Assosciation for the Advancement of Science, 1990, pp 1–19.
Bishop DVM, Jacobs PA, Lachlan K et al: Autism, language and communication in children with sex chromosome trisomies. Arch Dis Child 2011; 96: 954–959.
Metcalfe A, Coad J, Plumridge GM, Gill P, Farndon P : Family communication between children and their parents about inherited genetic conditions: a meta-synthesis of the research. Eur J Hum Genet 2008; 16: 1193–1200.
Gallo AM, Angst DB, Knalfl KA : Disclosure of genetic information within families. Am J Nurs 2009; 109: 65–69.
Gallo AM, Angst D, Knafl Ka, Hadley E, Smith C : Parents sharing information with their children about genetic conditions. J Pediatr Health Care 2005; 19: 267–275.
Villanueva A, Rebar R : Triple-X syndrome and premature ovarian failure. Obstet Gynecol 1983; 62: 70–73.
Holland CM : 47, XXX in an adolescent with premature ovarian failure and autoimmune disease. J Pediatr Adolesc Gynecol 2001; 14: 77–80.
Sugawara N, Maeda M, Manome T, Nagai R, Araki Y : Patients with 47, XXX karyotype who experienced premature ovarian failure (POF): two case reports. Reprod Med Biol 2013; 9–11.
Conners CK: Conners‘ Rating Scales-Revised. North Tonawanda, NY, USA: Multi-Health Systems, 2001, pp 83–98.
Boyatzis RE : Transforming Qualitative Information: Thematic Analysis and Code Development. London, UK: Sage, 1998.
Braun V, Clarke V : Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101.
Dennis A, Howell S, Cordeiro L, Tartaglia N : ‘How should I tell my child?’ Disclosing the diagnosis of sex chromosome aneuploidies. J Genet Couns 2015; 24: 88–103.
Bishop DVM, Scerif G : Klinefelter syndrome as a window on the aetiology of language and communication impairments in children: the neuroligin-neurexin hypothesis. Acta Paediatr 2011; 100: 903–907.
Robinson A, Bender BG, Linden MG : Decisions following the intrauterine diagnosis of sex chromosome aneuploidy. Am J Med Genet 1989; 34: 552–554.
Holmes-Siedle M, Ryynanen M, Lindenbaum RH : Parental decisions reagrding termination of pregnancy following prenatal detection of sex chromosome abnormality. Prenat Diagn 1987; 7: 239–244.
Sparrow SS, Cicchetti DV, Balla DA : Vineland Adaptive Behaviour Scales: Second Edition, Survey Interview Form/Caregiver Rating Form. Livonia, MN, USA: Pearson Assessments, 2005.
Bishop DVM : Children’s Communication Checklist, Version 2. London, UK: Pearson, 2003.
Goodman R : Strengths and Difficulties Questionnaire 1997. Available at http://www.sdqinfo.com/a0.html.
USAID Center for Development Information and Evaluation: ‘Conducting Focus Group Interviews.’ Performance Monitoring and Evaluation Tips 1996, Available at https://www.ndi.org/files/USAID%20Guide_Conducting%20Focus%20Groups.pdf.
Acknowledgements
Special thanks to the staff at Unique for their support in organising the Study Days, to Dr Karen Melham for assistance with focus groups and to all the families who gave up their time to participate in the study, without whom this would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Gratton, N., Myring, J., Middlemiss, P. et al. Children with sex chromosome trisomies: parental disclosure of genetic status. Eur J Hum Genet 24, 638–644 (2016). https://doi.org/10.1038/ejhg.2015.168
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2015.168
This article is cited by
-
Understanding the phenotypic spectrum and family experiences of XYY syndrome: Important considerations for genetic counseling
Journal of Community Genetics (2023)
-
Healthcare and support experiences of adolescents and young adults diagnosed with 47,XXY, 47,XXX, and 48,XXYY
Journal of Community Genetics (2023)
-
Communicating the diagnosis of Klinefelter syndrome to children and adolescents: when, how, and who?
Journal of Community Genetics (2022)