Abstract
Megalencephaly-capillary malformation (MCAP) syndrome is an overgrowth syndrome that is diagnosed by clinical criteria. Recently, somatic and germline variants in genes that are involved in the PI3K-AKT pathway (AKT3, PIK3R2 and PIK3CA) have been described to be associated with MCAP and/or other related megalencephaly syndromes. We performed trio-exome sequencing in a 6-year-old boy and his healthy parents. Clinical features were macrocephaly, cutis marmorata, angiomata, asymmetric overgrowth, developmental delay, discrete midline facial nevus flammeus, toe syndactyly and postaxial polydactyly—thus, clearly an MCAP phenotype. Exome sequencing revealed a pathogenic de novo germline variant in the PTPN11 gene (c.1529A>G; p.(Gln510Arg)), which has so far been associated with Noonan, as well as LEOPARD syndrome. Whole-exome sequencing (>100 × coverage) did not reveal any alteration in the known megalencephaly genes. However, ultra-deep sequencing results from saliva (>1000 × coverage) revealed a 22% mosaic variant in PIK3CA (c.2740G>A; p.(Gly914Arg)). To our knowledge, this report is the first description of a PTPN11 germline variant in an MCAP patient. Data from experimental studies show a complex interaction of SHP2 (gene product of PTPN11) and the PI3K-AKT pathway. We hypothesize that certain PTPN11 germline variants might drive toward additional second-hit alterations.
Similar content being viewed by others
INTRODUCTION
The megalencephaly-capillary malformation (MCAP) syndrome (OMIM #602501) is a clinically recognizable syndrome, consisting of megalencephaly and other typical features (see Table 1). It has first been described as macrocephaly-cutis marmorata (M-CM) teleangiectatica syndrome in 19971, 2 and been renamed in 2007 to M-CM syndrome.3 In order to reflect the very large brain size—rather than simply a large head—Mirzaa et al4 proposed to re-rename the syndrome as MCAP syndrome, which is the current nomenclature until today.
Not surprisingly, there exist various diagnostic criteria for MCAP syndrome, differing in minor criteria depending on the respective authors.5 To date, >140 cases have been reported in the literature.6 Extensive work has been done to reveal the molecular causes and mechanisms of this, as well as the associated megalencephaly-polymicrogyria-polydactyly-hydrocephalus (MPPH) syndrome.
Rivière et al7 were the first to report on de novo germline and postzygotic variants in MCAP and MPPH syndromes in three key factors of the PI3K-AKT pathway: AKT3, PIK3R2 and PIK3CA. In MCAP syndrome, only PIK3CA variants have been found (22 postzygotic and 2 germline variants).6
In this report, we describe the first patient with MCAP syndrome in whom exome sequencing revealed a germline PTPN11 variant, whereas ultra-deep sequencing from saliva showed a 22% mosaic for a PIK3CA variant.
We discuss possible biological mechanisms that might be responsible for this intriguing observation.
Clinical report
The index patient is a 6-year-old boy from consanguineous Turkish parents (cousins of second degree). Pregnancy was uneventful, but his mother has had two early miscarriages previously. Birth weight was 4230 g (98th centile), body length was 56 cm (98th centile) and head circumference was 36.5 cm (95th centile). APGAR scores were 10/10/10, and arterial umbilical pH was 7.34. Directly after birth, bilateral postaxial polydactyly and syndactyly II/III of the feet were detected.
Motor development, as well as speech development, were delayed. He learned to walk at 22 months.
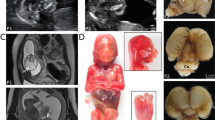
Examination at the age of 6 years and 3 months: Friendly and cooperative boy. Striking features were cutis marmorata, macrocephaly (head circumference 56.5 cm,+2.9 SD>98th centile), frontal bossing, hemangiomata (nasal root, tongue and lower lip), discrete facial nevus flammeus and hemihypertrophy of the left body part. Postaxial hexadactyly had been operated; syndactyly II/III had only been operated on the right side. According to the clinical criteria,5 the diagnosis MCAP syndrome could be established (see Table 1; some clinical features are shown in Figure 1).
METHODS AND RESULTS
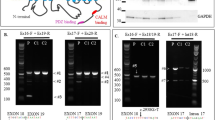
After array-CGH analysis and candidate gene sequencing of the megalencephaly genes AKT3, PIK3R2 and PIK3CA of leukocyte DNA by conventional methods (Sanger sequencing) had returned normal results, we performed trio-exome sequencing of the boy and his parents. The diagnostic pipeline was as previously reported.8
Exome sequencing of leukocyte DNA revealed a de novo heterozygous variant in the PTPN11 gene (c.1529A>G; p.(Gln510Arg); according to LRG_614, NG_007459.1, NM_002834.3 and ENST00000351677). Both parents did not carry this variant. Paternity was confirmed. This finding was confirmed by Sanger sequencing from buccal swab DNA, therefore suggesting a germline PTPN11 variant. As that variant has been described to be associated with Noonan9 and LEOPARD10 syndrome and thus did not seem to explain the patient’s complete phenotype, special attention was payed to the megalencephaly genes PIK3CA, PIK3R2 and AKT. In DNA from blood, no variant could be detected (coverage: >150-fold). Deep sequencing results of 551 tumor-associated genes from saliva (CeGaT somatic tumor panel TUM01, version 2; http://cegat.de/Tumor-panel-%28somatic%29_l=1_202.html, including PIK3CA, PIK3R2 and AKT; coverage: >1000-fold) revealed a known disease-causing variant in PIK3CA (c.2740G>A; p.(Gly914Arg); according to LRG_310, NG_012113.2, NM_006218.2 and ENST00000263967) in 172 out of 1572 reads, thus indicating that 22% of the cells carry the variant in a heterozygous state (somatic mosaic).
The patient phenotype and the detected variants have been submitted to the Leiden Open Variation Database (LOVD 3.0; http://databases.lovd.nl/shared/individuals/00016593).
DISCUSSION
Variants in the RAS-MAPK pathway are known as the cause of several entities of the neuro-cardio-facio-cutaneous syndrome spectrum, which share many clinical features but, depending on the location of the variant in the pathway, display distinguishable phenotypes. The most common phenotype is Noonan syndrome (the prevalence is estimated to be 1:1000–1:2500), but there are other distinct phenotypes such as LEOPARD (lentigines, electrocardiographic abnormalities, ocular hypertelorism, pulmonary stenosis, abnormal genitalia, retardation, deafness) syndrome, cardio-facio-cutaneous syndrome, Costello syndrome, neurofibromatosis type 1 and Legius syndrome. As the variants all lead to functionally altered proteins in the RAS-MAPK pathway, this group is also referred to as ‘rasopathies’.11, 12
Recently, variants in the PI3K-AKT pathway have been described to be associated with megalencephaly and overgrowth syndromes, such as MCAP and MPPH,5, 6, 7 but also CLOVES (congenital lipomatous asymmetric overgrowth, epidermal naevi, skeletal and spinal anomalies) syndrome,13, 14 as well as hemimegalencephaly15 and isolated macrodactyly.16
Although both the RAS-MAPK pathway and the PI3K-AKT pathway are very complex and still only partly understood, interactions between these two signaling pathways are well known: most importantly but not exclusively, activated GTP-bound RAS not only induces the MAP-kinase cascade through association with RAF, but can also bind to PI3K to increase the generation of PIP3 out of PIP2, thereby activating several downstream effectors such as mTOR, BAX or FOXO—each directing to distinct cellular results leading to inhibition of apoptosis, initiation of translation, cell proliferation and loss of cell differentiation (see Figure 2).
Simplified synopsis on the PI3K-AKT and RAS-MAPK signaling pathways and their interactions. The signaling cascades start at a receptor tyrosine kinase (e.g., a growth hormone receptor). Shown on the left is the PI3K-AKT pathway, on the right the RAS-MAPK pathway. (Some) interactions of the pathways are highlighted by thick arrows: activated RAS is known to interact with PI3K, activating its downstream signaling. Furthermore, SHP2 (the protein encoded by PTPN11) also interacts with the PI3K pathway. The effects are shown in the red boxes: inhibition of apoptosis, start of translation, induction of cell proliferation and inhibition of cell differentiation. All of these are possible underlying mechanisms not only of MCAP, but also of tumorigenesis. GF, growth factor; RTK, receptor tyrosine kinase; PI3K, phosphatidyl-inositol-3-kinase; PIP2, phosphatidyl-inositol-bisphosphate; PIP3, phosphatidyl-inositol-trisphosphate; AKT, PKB (protein kinase b); BAX, Bcl-2-like protein 4; Rheb, Ras homolog enriched in brain; mTOR, mammalian target of rapamycin; S6K, S6 kinase; FOXO, forkhead box protein O; GRP2, growth factor receptor-bound protein 2; GAB2, GRB2-associated protein 2; SHC, Src 2 homology domain containing; SHP2, gene product of PTPN11; SOS, son of sevenless; RAS, rat sarcoma protein; RAF, RAS-associated factor; MEK, mitogene-activated protein kinase kinase, ERK, extracellular signal-regulated kinase; AP-1, activating protein 1. The full colour version of this figure is available at European Journal of Human Genetics online.
Apart from implications in neurodevelopmental disorders, both pathways are extensively described in tumorigenesis17 and many of the above mentioned syndromes are associated with a higher risk for the development of benign and/or malignant tumors.
For example, in MCAP syndrome, many benign vascular tumors (described as hemangiomas, angiomata and angiomyolipomas),5 but also two meningeomas,1, 18 as well as a few malignant tumors have been reported (two children with Wilms tumor19, 20 and leukemia in an 18-year-old1).
In Noonan patients, juvenile myelocytic leukemia (JMML) occurs more often than in the general population.11 As biologically suspected, disruption of the RAS-MAPK pathway lowers the transformation rate to tumor cells in vitro.21 Interestingly, also intervention on the PI3K-AKT pathway has been shown to have positive effects: AKT phosphorylation is known to be elevated in PTPN11-induced JMML, and also mTOR inhibitors have been shown to be effective in in vitro studies.21, 22, 23, 24 This intriguing observation has been confirmed by animal studies. In line with the in vitro data, there is evidence that hypertrophic cardiomyopathy caused by specific Ptpn11 variants in cell lines and mouse models of LEOPARD syndrome can be successfully treated by mTOR inhibition (rather than MEK inhibition).25, 26, 27, 28
Thus, it can be concluded that alteration of both the MAP-kinase cascade and the PI3K-AKT effector pathway are involved in the pathophysiology of rasopathies. Certain organ manifestations may be mediated not only by one of these two pathways, but by a specific interaction of the two. It should be noted that this interaction might be tissue specific and time dependent.
This hypothesis is further supported by the following observations: during the last years, oncogenomics revealed that PIK3CA variants frequently coexist with RAS and BRAF variants in patients with advanced cancer.29 A very recent publication even showed that in 4 out of 50 advanced gastric cancers, PIK3CA and PTPN11 were both mutated, leading to activation of the AKT pathway.30
This seems to be more than just coincidence. It is known that in most cancers, there is not only one gene that is mutated, but a distinct set of genes. Not all of these variants seem to be relevant: most of the alterations are described to be ‘passenger mutations’, indicating their rather passive role in tumorigenesis. However, some are known to be ‘driver mutations’ and are essential for tumor progression.
MCAP being an overgrowth syndrome is pathogenically closely related to tumor disorders, as the same pathways are affected. Therefore, it is possible and biologically plausible that in our patient, the PTPN11 variant is not just coincidental, but preceding (or even causing) the PIK3CA variant.
Further studies, for example, systematic screening of MCAP patients for alterations in the RAS-MAPK pathway, are needed to confirm this hypothesis. Especially in the context of tumor risk, the knowledge of a second alteration in another pathway might not just be academically interesting, but very valuable for planning individual risk assessment strategies.
Our ‘second hit’ hypothesis is further supported by the first patient reported in the literature carrying the same PTPN11 variant (c.1529A>G; p.(Gln510Arg)).9 Apart from the PTPN11 variant, the female index patient in this publication also showed an NF1 variant. She exhibited symptoms of both phenotypes, whereas her father who only had the PTPN11 variant was described to have a Noonan phenotype.9
In conclusion, there is a lot of evidence that activation of both the RAS-MAPK pathway, as well as the PI3K-AKT pathway has a major role in the pathogenesis of rasopathies. In tumors, both of these effector pathways seem to be associated not only in a functional way, but on DNA level, as variants in effectors of both pathways co-occur frequently in some advanced tumors. The same mechanism might be responsible for the phenotype presented in this report.
Further patient and animal studies are needed to address the link between overgrowth syndromes and rasopathies. Clinicians are encouraged to search for somatic variants in patients with unusual clinical features by using next-generation sequencing approaches. It should be noticed that somatic variants might not be detectable from blood, so analysis of a second tissue such as saliva or skin should be considered.
References
Moore CA, Toriello HV, Abuelo DN et al: Macrocephaly-cutis marmorata telangiectatica congenita: a distinct disorder with developmental delay and connective tissue abnormalities. Am J Med Genet 1997; 70: 67–73.
Clayton-Smith J, Kerr B, Brunner H et al: Macrocephaly with cutis marmorata, haemangioma and syndactyly—a distinctive overgrowth syndrome. Clin Dysmorphol 1997; 6: 291–302.
Toriello HV, Mulliken JB : Accurately renaming macrocephaly-cutis marmorata telangiectatica congenita (M-CMTC) as macrocephaly-capillary malformation (M-CM). Am J Med Genet A 2007; 143A: 3009.
Mirzaa GM, Conway RL, Gripp KW et al: Megalencephaly-capillary malformation (MCAP) and megalencephaly-polydactyly-polymicrogyria-hydrocephalus (MPPH) syndromes: two closely related disorders of brain overgrowth and abnormal brain and body morphogenesis. Am J Med Genet A 2012; 158A: 269–291.
Mirzaa G, Conway R, Graham JM, Dobyns WB : PIK3CA-related segmental overgrowth 1993 http://www.ncbi.nlm.nih.gov/books/NBK153722/ Last update 2013.
Mirzaa GM, Riviere JB, Dobyns WB : Megalencephaly syndromes and activating mutations in the PI3K-AKT pathway: MPPH and MCAP. Am J Med Genet C Semin Med Genet 2013; 163C: 122–130.
Riviere JB, Mirzaa GM, O'Roak BJ et al: De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet 2012; 44: 934–940.
Döcker D, Schubach M, Menzel M et al: Further delineation of the SATB2 phenotype. Eur J Hum Genet 2013, e-pub ahead of print 4 December 2013; doi:10.1038/ejhg.2013.280.
Bertola DR, Pereira AC, Passetti F et al: Neurofibromatosis-Noonan syndrome: molecular evidence of the concurrence of both disorders in a patient. Am J Med Genet A 2005; 136: 242–245.
Carcavilla A, Santome JL, Pinto I et al: LEOPARD Syndrome: a variant of Noonan syndrome strongly associated with hypertrophic cardiomyopathy. Rev Esp Cardiol 2013; 66: 350–356.
Tartaglia M, Gelb BD, Zenker M : Noonan syndrome and clinically related disorders. Best Pract Res Clin Endocrinol Metab 2011; 25: 161–179.
Zenker M : Genetic and pathogenetic aspects of Noonan syndrome and related disorders. Horm Res 2009; 72 (Suppl 2): 57–63.
Kurek KC, Luks VL, Ayturk UM et al: Somatic mosaic activating mutations in PIK3CA cause CLOVES syndrome. Am J Hum Genet 2012; 90: 1108–1115.
Lindhurst MJ, Parker VE, Payne F et al: Mosaic overgrowth with fibroadipose hyperplasia is caused by somatic activating mutations in PIK3CA. Nat Genet 2012; 44: 928–933.
Lee JH, Huynh M, Silhavy JL et al: De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nat Genet 2012; 44: 941–945.
Rios JJ, Paria N, Burns DK et al: Somatic gain-of-function mutations in PIK3CA in patients with macrodactyly. Hum Mol Genet 2013; 22: 444–451.
Steelman LS, Chappell WH, Abrams SL et al: Roles of the Raf/MEK/ERK and PI3K/PTEN/Akt/mTOR pathways in controlling growth and sensitivity to therapy-implications for cancer and aging. Aging (Albany NY) 2011; 3: 192–222.
Conway RL, Pressman BD, Dobyns WB et al: Neuroimaging findings in macrocephaly-capillary malformation: a longitudinal study of 17 patients. Am J Med Genet A 2007; 143A: 2981–3008.
Lapunzina P, Gairi A, Delicado A et al: Macrocephaly-cutis marmorata telangiectatica congenita: report of six new patients and a review. Am J Med Genet A 2004; 130A: 45–51.
Wright DR, Frieden IJ, Orlow SJ et al: The misnomer "macrocephaly-cutis marmorata telangiectatica congenita syndrome": report of 12 new cases and support for revising the name to macrocephaly-capillary malformations. Arch Dermatol 2009; 145: 287–293.
Mohi MG, Williams IR, Dearolf CR et al: Prognostic, therapeutic, and mechanistic implications of a mouse model of leukemia evoked by Shp2 (PTPN11) mutations. Cancer Cell 2005; 7: 179–191.
Goodwin CB, Yang Z, Yin F, Yu M, Chan RJ : Genetic disruption of the PI3K regulatory subunits, p85alpha, p55alpha, and p50alpha, normalizes mutant PTPN11-induced hypersensitivity to GM-CSF. Haematologica 2012; 97: 1042–1047.
Goodwin CB, Li XJ, Mali RS et al: PI3K p110delta uniquely promotes gain-of-function Shp2-induced GM-CSF hypersensitivity in a model of JMML. Blood 2014; 123: 2838–2842.
Polivka J Jr., Janku F : Molecular targets for cancer therapy in the PI3K/AKT/mTOR pathway. Pharmacol Ther 2013; 142: 164–175.
Marin TM, Clemente CF, Santos AM et al: Shp2 negatively regulates growth in cardiomyocytes by controlling focal adhesion kinase/Src and mTOR pathways. Circ Res 2008; 103: 813–824.
Marin TM, Keith K, Davies B et al: Rapamycin reverses hypertrophic cardiomyopathy in a mouse model of LEOPARD syndrome-associated PTPN11 mutation. J Clin Invest 2011; 121: 1026–1043.
Schramm C, Fine DM, Edwards MA, Reeb AN, Krenz M : The PTPN11 loss-of-function mutation Q510E-Shp2 causes hypertrophic cardiomyopathy by dysregulating mTOR signaling. Am J Physiol Heart Circ Physiol 2012; 302: H231–H243.
Ishida H, Kogaki S, Narita J et al: LEOPARD-type SHP2 mutant Gln510Glu attenuates cardiomyocyte differentiation and promotes cardiac hypertrophy via dysregulation of Akt/GSK-3beta/beta-catenin signaling. Am J Physiol Heart Circ Physiol 2011; 301: H1531–H1539.
Janku F, Lee JJ, Tsimberidou AM et al: PIK3CA mutations frequently coexist with RAS and BRAF mutations in patients with advanced cancers. PLoS One 2011; 6: e22769.
Yoda Y, Takeshima H, Niwa T et al: Integrated analysis of cancer-related pathways affected by genetic and epigenetic alterations in gastric cancer. Gastric Cancer 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Döcker, D., Schubach, M., Menzel, M. et al. Germline PTPN11 and somatic PIK3CA variant in a boy with megalencephaly-capillary malformation syndrome (MCAP) - pure coincidence?. Eur J Hum Genet 23, 409–412 (2015). https://doi.org/10.1038/ejhg.2014.118
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2014.118
This article is cited by
-
The Orthopaedic Management of Hip Dysplasia with Underlying Megalencephaly-Capillary Malformation Syndrome: a Case Report
SN Comprehensive Clinical Medicine (2022)
-
Megalencephaly-capillary malformation syndrome and associated hydrocephalus: treatment options and revision of the literature
Child's Nervous System (2021)
-
Clinical pitfalls in the diagnosis of segmental overgrowth syndromes: a child with the c.2740G > A mutation in PIK3CA gene
Italian Journal of Pediatrics (2018)