Abstract
Pluripotency and proliferative capacity of human embryonic stem cells (hESCs) make them a promising source for basic and applied research as well as in therapeutic medicine. The introduction of human induced pluripotent cells (hiPSCs) holds great promise for patient-tailored regenerative medicine therapies. However, for hESCs and hiPSCs to be applied for therapeutic purposes, long-term genomic stability in culture must be maintained. Until recently, G-banding analysis was considered as the default approach for detecting chromosomal abnormalities in stem cells. Our goal in this study was to apply fluorescence in-situ hybridization (FISH) and comparative genomic hybridization (CGH) for the screening of pluripotent stem cells, which will enable us identifying chromosomal abnormalities in stem cells genome with a better resolution. We studied three hESC lines and two hiPSC lines over long-term culture. Aneuploidy rates were evaluated at different passages, using FISH probes (12,13,16,17,18,21,X,Y). Genomic integrity was shown to be maintained at early passages of hESCs and hiPSCs but, at late passages, we observed low rates mosaiciam in hESCs, which implies a direct correlation between number of passages and increased aneuploidy rate. In addition, CGH analysis revealed a recurrent genomic instability, involving the gain of chromosome 1q. This finding was detected in two unrelated cell lines of different origin and implies that gains of chromosome 1q may endow a clonal advantage in culture. These findings, which could only partially be detected by conventional cytogenetic methods, emphasize the importance of using molecular cytogenetic methods for tracking genomic instability in stem cells.
Similar content being viewed by others
Introduction
Human embryonic stem cells (hESCs), derived from the inner cell mass of a human blastocyst, are pluripotent and self-renewable. They present a potential valuable tool for regenerative medicine and serve as models of embryonic development in vitro.1, 2 The first ESC lines were isolated from mouse embryos in the early 1980s,3 but the first report on the derivation of hESCs was published nearly 20 years later in 1998.4 Since then, hundreds of hESC lines have been derived and characterized and a vast number of laboratories are trying to differentiate these cells for future therapeutic use.
Recently, a new type of human stem cells, human-induced pluripotent stem cells (hiPSCs), has become available to the scientific community. Human iPSCs are derived from somatic cells, such as adult fibroblasts,5 which have been reprogrammed to mimic ESCs by forcing the transgenic expression of defined transcription factors. A cocktail of four transcription factors (OCT4, SOX2, C-MYC and KLF4) was successfully used to fully reprogram the somatic cells into pluripotent stem cells. And so, hiPSCs exhibit the same phenotypical characteristics as the hESCs. Patient-specific iPSCs have the advantage of avoiding many of the ethical concerns associated with the use of embryonic material, and have no risk of immune rejection.6
Human ESCs and iPSCs offer the opportunity to recapitulate human cell ontogenesis in vitro, and to investigate the efficacy of drug therapies. Moreover, they represent a promising source for substitutive and regenerative allogenic (hESCs) or autologous (hiPSCs) cell therapies. Unlimited self-renewal property bears the risk of presence of genomic abnormalities; therefore, one of the issues that must be addressed before ESCs and iPSC technology can be applied to regenerative medicine regards their genomic integrity during culture. Concerns are already growing about the clinical application of iPSC after recently published data have identified disease-related mutations, epigenetic modifications and copy number variations in reprogrammed cells.7 The duration of culture and the culture conditions have also been pointed at as possible contributing factors to chromosomal changes in hESCs.8 A classic cytogenetic protocol (G banding) is considered as the default approach for routine karyotypic assessment,9, 10 and is the method widely used to value chromosome integrity.11 Karyotypic abnormalities of hESCs in long-term cultures have been reported before.12, 13, 14, 15 In hESCs, most of the alteration have been attributed to chromosomes 12 and 17, but chromosomes X and 20 were also repeatedly described.12, 16 G-banding technique is extremely laborious, requires dividing cells in culture and metaphases of sufficient quality for analysis, which have already proven difficulties to obtain. Moreover, conventional karyotype is not sensitive enough and may not be effective in evaluating genome integrity, as many of the intrachromosomal rearrangements and submicroscopic alterations in the genome can be missed due to the low resolution of the technique. Therefore, the use of advanced techniques is of crucial importance.
Fluorescence in-situ hybridization (FISH) is the hallmark of molecular cytogenetics and can be used to evaluate aneuploidy rate and to detect mosaicism. In addition, FISH can detect chromosome abnormalities such as submicroscopic deletions or amplifications, which are beyond the resolution of conventional karyotyping.17 However, detecting these abnormalities require a prior knowledge of the genomic region of interest. Another molecular-cytogenetic method is comparative genomic hybridization – CGH (conventional and array), for the analysis of copy number changes (gains/losses) in the DNA content in a single experiment, without requiring fresh samples (dividing cells).18 High-resolution array CGH is a growing used method to assess genetic integrity of hPSC cultures and allows identifying small regions, while chromosomal CGH is in sufficient resolution when the goal is to detect ≥5 Mb changes. As human pluripotent stem cells can and are often propagated for extended periods of time, monitoring and controlling the integrity of the genome of these cells is extremely important. The genomic stability question should be at the forefront when considering whether hESCs and hiPSCs will serve in clinical applications. In this research, we have studied hESC lines and hiPSC lines during long-term culture, in order to study their genomic integrity. We integrated several techniques that allowed us to get a better comprehensive data.
Materials and methods
Culturing hESC and hiPSC lines
HESC lines I3, I419 and H14 were cultured with inactivated MEF (mouse embryonic fibroblasts) as was previously described11 for 19–102 passages.
HiPSCs lines C2 and C3 derived from foreskin fibroblast using four constitutively expressed reprogramming constructs (AddGene, http://www.addgene.org): including pMXs-hOCT4 (17217, Shinya Yamanaka), pMXs-hSOX2 (17218, Shinya Yamanaka), pMXs-hKLF4 (17219, Shinya Yamanaka), pMXS-hc-MYC (17220, Shinya Yamanaka). The cells were cultured with inactivated MEF as previously described.20
HESCs and hiPSCs were passaged every 4–6 days using 1.5 mg/ml type IV collagenase (Worthington Biochemical Corporation, Lakewood, NJ, USA). We used previously defined criteria for characterization of hES and hiPS cells by examining their morphology, surface markers, growth rates, karyotype and pluripotency.21
Stem cells harvesting
The cells were harvested on day 3 after passaging. Cells were treated with 15 μg/ml CRA (Zotal, Tel Aviv, Israel) for 60 min followed by 0.75 μg/ml colcemid for 30 min (Biological Industries, Beit Haemek, Israel), during incubation at 37 °C. Next, cells were collected using trypsin (Beit Haemek, Israel), incubated for 5 min at 37 °C in 0.075 M KCl+Na citrate solution and fixed three times in fixative solution (3:1 methanol/acetic acid). Cells remained in −20 °C until use and spread on slides before analysis.
Karyotype analysis
Cells were stained for G banding with a trypsin-Giemsa solution. Karyotype analysis (G banding) was performed on at least 20 metaphases per sample, as previously described.22 Karyotypes were analyzed and reported according to the ‘International System for Human Cytogenetic Nomenclature’ (ISCN 2010).
DNA extraction
High molecular weight DNA was isolated from the SC samples at different passages using the Promega Genomic DNA Purification Kit (Madison, WI, USA). DNA from healthy male donors (served as reference for CGH experiments, single sample for each test) was extracted from leukocytes using the 5Prime kit (Zotal), following manufacturer's recommended protocol. DNA concentration and purity was evaluated by UV spectrophotometeric measurements and agarose gel eletrophoresis. All DNA samples had an A260/A280 ratio of 1.8–2.0, an A260/A230 ratio of >1.5 and run on agarose gel as a high molecular band.
Amniotic cells harvest and fixation
Amniotic fluid cells cultured on coverglass (serves as control group I): 20 ml amniotic fluid was obtained from five women in 17–20 weeks of pregnancy; The women ranged in age from 25 to 38 years (mean±SD of 32±5 years). Samples were cultured on coverglass for ∼3 weeks and harvested according to standard techniques.23
Uncultured amniotic fluid cells (serves as control group II): 10 ml amniotic fluid was obtained from 10 women in 17–20 weeks of pregnancy; The women ranged in age from 25 to 39 years (32.2±4.6 years). All samples were treated as previously described.17
Fluorescent in-situ hybridization
FISH analysis took place using three sequential hybridizations. Cycle 1: Chromosomes 12, 16, 17 labeled with three different fluorochromes; Cycle 2: Chromosomes 18, X, Y labeled with three different fluorochromes; Cycle 3: Chromosomes 13, 21 labeled with two different fluorochromes; these regions were examined along with any other chromosomes that had given an abnormal CGH result. All probes used during this study came from Abbott (Abbott Molecular, Abbot Park, IL, USA) and summarized in Table 1. The protocol used was described previously.17 Signal scoring was performed according to stringent criteria: cells were scored as ‘normal’ if FISH clearly indicated two separate signals for each probe, while ‘abnormal’ cell showed derivation from the normal signal pattern.24 Two signals represent two homolog chromosomes when their distance apart was at least two domain diameters.25 Two signals that are less than two domains apart are considered as one duplicated signal and represent single homolog chromosome.
Comparative genomic hybridization
At the time of DNA extraction, colonies were allowed to grow for 4–5 days on MEFs before they were mechanically isolated. DNA samples were labeled via nick translation, according to manufacturer's instructions (Abbott), with the SC DNA labeled green (Green-dUTP; Abbott) and the reference DNA labeled red (Red-dUTP; Abbott). Co-precipitation of test and reference DNAs, their denaturation, along with that of the slides, and the post-hybridization washes all were conducted as described previously.26 Digital images were used to facilitate the identification of chromosomal regions with abnormal fluorescence ratios. Images of the hybridized metaphases were evaluated as previously published,27 with a detection resolution ≥5 Mb.28
Statistical analysis
The frequency of loss or gain of individual chromosomes was examined. Statistical significance between groups was determined by using a two-tailed, unpaired, Student's t-test. The frequency of aneuploidy per case (the number of abnormal cells divided by the total number of cells examined) was tested for correlation with passage number by Pearson's correlation analysis. The monosomy/trisomy ratio for individual chromosomes was determined by using a one-tailed paired Student's t-test.
We considered P-values<0.05 as statistically significant.
Results
Three hESC lines and two hiPSC lines were analyzed at different passages using three cytogenetic methods: G banding, FISH and CGH. Table 2 summarizes all chromosomal analyses preformed for each line. All three hESC lines analyzed (I3, I4, H1) had shown to meet the criteria of a defined hESC.
Aneuploidy rates of hESCs and hiPSCs
A total of 5940 hESCs and hiPSCs were scored for aneuploidy using three sets of FISH probes (see Materials and methods – FISH). For hESC lines (I3, I4, H1), an average of 154 (±66) cells was scored per probe in each passage examined. For hiPSC lines (C2, C3), an average of 148 (±45) cells was scored per probe in each passage examined. Table 3 summarizes aneuploidy rates of hESCs and hiPSCs at the passages examined.
Two sets of control groups were used in this study: Control group I consists of 10 different uncultured amniotic fluid cell samples, serves as baseline for aneuploidy rate in uncultured cells. These cells were selected for control since they are not cultured in vitro and therefore characterize, most accurately, the cells in the fetus' body. Overall, 1500 cells were scored in this group and results are summarized in Table 3. From each sample, an average of 100(±20) cells for each probe was scored. Average aneuploidy rate was found to be 0.7% (±0.1). Control group II consists of five different cultured amniotic fluid cell samples that were cultured for several cell divisions in vitro (average of 17 days in culture). This type of control allowed us to compare between cultured samples. Overall, total of 1200 culture amniotic fluid cells were scored in this group and results are summarized in Table 3. From each sample, an average of 145 cells (±15) for each probe was scored and average aneuploidy rate was 1.6% (±0.4).
All samples used as controls were analyzed and found to be karyotypically normal.
Mosaic aneuploidy in hESCs
Comparison between average aneuploidy rate of hESCs and controls is displayed in Figure 1a; mean aneuploidy rate in hESC lines was significantly higher (4.2±1.6%) and revealed pervasive mosaicism comparing with aneuploidy rates in non-cultured amniotic fluid samples (P<0.05) and in cultured amniotic fluid samples (P<0.05). This difference remains significant when restricting the analysis of hESCs to passages lower then 70 (P<0.05).
(a) Average aneuploidy rate in hESCs comparing with controls, significant difference was found between groups and is marked with *(P<0.05). (b) Average aneuploidy rate in hiPSCs comparing with controls. No statistical difference was found between groups. Student's t-test was used to determine significance of difference in aneuploidy levels between each two groups. Aneuploidy rates and standard error bars are presented for each cell source.
HiPSCs aneuploidy screening
Comparison between average aneuploidy rate of hiPSCs and controls is displayed in Figure 1b; average aneuploidy levels ranged between 0.6 and 5.5% (Table 3) with mean rate of 2.1% (±1.3). No statistical difference was found between hiPSCs and control cells (both uncultured and cultured cells, P>0.1).
Aneuploidy rate for individual chromosomes
Chromosome gain and loss were found in all tested chromosomes and appear to be stochastic. However, an increase in aneuploidy rate of chromosomes 18 was observed in hESC lines and of chromosomes 17 and 18 in hiPSC lines (Figure 2).
Aneuploidy rate for individual chromosomes, presented as monosomy/trisomy ratio variations for individual chromosomes. An increase in the frequency of autosomal trisomy/monosomy for chromosome 18 was observed in hESC lines, and for chromosomes 17 and 18 in hiPSC lines. Monosomy rate was significantly higher than trisomy rate (P<0.05) when combining all chromosomes results.
Monosomy and trisomy rates
Variations for individual chromosomes are presented in Figure 2. Aneuploidy rate per chromosome ranged between 0.3 and 2.6%, with an average rate of 1.3% (±0.6) per chromosome. We found that monosomy rate was significantly higher than trisomy rate (P<0.05) when combining all chromosomes results.
Aneuploidy rate increases over time
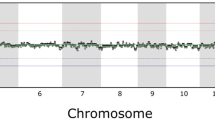
Aneuploidy rate in all cell lines increased in direct correlation to number of passages (r=0.83, Pearson's correlation) and is presented by the different stem cells' types in Figures 3a and b.
Chromosome analysis of line I4 in culture
G-banding analysis of line I4 at passage 83 has raised the possibility of chromosome aberration. At passage 98, we identified, by G banding, an unexplained additional segment on the short arm of chromosome 2 in 20 metaphases analyzed; 46,XX,ins(2;?)(p16;?)[2]/46,XX[18] (Figure 4a, G banding).
(a) G banding of line I4, p.98 showing an additional segment in the short arm of chromosome 2. (b) CGH analysis to a DNA extract from line I4, p.98 identified a fragment amplification of the short arm of chromosome 1 [ish cgh amp(1)(p32p34.1)]. (c) FISH analysis of line I4, p.98 with whole chromosome 1 paint located this interstitial amplified region to the short arm of chromosome 2. (d) CGH analysis of line I4 at passage 59 showing rev ish amp(1)(q21q32). (e) Line I4, passage 90 – ish cgh amp(1)(p32p34.1) and ish cgh amp(1)(q21q32). (f) CGH analysis of line C3, passage 55 showed a fragment amplification of the long arm of chromosome 1, ish cgh amp(1)(q21qter). (g) FISH analysis of line C3-passage 55, with specific probes for chromosome 1, (D1Z5 and Tel1q) demonstrated the amplification.
CGH analysis, which was performed on DNA extract from this passage, identified a fragment amplification of the short arm of chromosome 1; ish cgh amp(1)(p32p34.1) (Figure 4b). FISH analysis with a painting probe of chromosome 1 verified these findings, and also located this interstitial amplified region to the short arm of chromosome 2 (Figure 4c, FISH). Further CGH analysis of this cell line, at earlier passages, revealed: at passage 59: ish cgh amp(1)(q21q32) (Figure 4d) and at passage 90: ish cgh amp(1)(p32p34.1) and ish cgh amp (1)(q21q32) (Figure 4e).
Lines I3 and H1 maintained normal karyotype, determined at different passages (Table 2) by G banding and by CGH (Supplementary data 1), even after freeze-thaw procedures and continuous in-vitro culture for over 100 passages.
Chromosome analysis of lines C2 and C3 in culture
The hiPSC lines C2 and C3 have previously been examined and were found to have a normal 46,XY karyotype, using G-banding method (Table 2). Line C3, examined by CGH at passage 55, showed a fragment amplification of the long arm of chromosome 1: ish cgh amp(1)(q21qter) (Figure 4f). Karyotype analysis of line C3 growing in suspension detected the same aberration. FISH performed on cell nuclei using specific probes for chromosome 1 detected high rate mosaicism: nuc ish (3XD1Z5),(3xTel1q)[44/150] (Figure 4g).
Simultaneously, C3 cells exhibited an aberrant growth and the culture had altered from colony growth to monolayer cell growth on MEF (Supplementary data 2).
Discussion
Human ESCs and hiPSCs hold great promises for biomedical applications such as cell replacement therapy, developmental biology, drug discovery and disease modeling. Clearly, therapeutic applications require maintaining of pluripotency and genomic integrity.1, 2 Our observations of low rate mosaic aneuploidy and chromosomal changes occurring both in hESC lines and in hiPSCs, not only suggest caution but should encourage researchers to perform regular high-resolution molecular and cytogenetic studies to verify the chromosome integrity in hESCs and hiPSCs, with the combination of several cytogenetic techniques.
Molecular cytogenetic analysis
The most commonly used technology today for genome integrity investigation of stem cells is G banding.29 Karyotyping using G banding requires extended analysis time as obtaining high quality metaphases is difficult, the number of cells amenable to analysis is sometimes limited, and clones of cells with chromosomal changes can easily be missed.30 Moreover, detecting low rate mosaicism (under ∼20%) in cell cultures using G banding is almost impossible. In this study, we used other possible strategies to investigate the chromosomal constitution within stem cell lines.
CGH enables an overview of the whole genome and proved to be a feasible technique to characterize the chromosomal constitution of pluripotent stem cells. However, CGH measures the genomic DNA content and therefore low rate mosaicism and balanced rearrangements are not detected with this method.30 Interphase FISH allows screening of a large number of cells for chromosomal aberrations, balanced rearrangement and mosaicism in a relatively short time. FISH data of this assay revealed low rate mosaic aneuploidy that was not detected by G banding. But, with FISH, only a limited part of the genome – which is homologs to the probes regions – can be analyzed. This fact raises difficulties since by now, there are many chromosomal regions that have been identified as recurrently mutated in cultured pluripotent stem cells31 and our findings in the current study indicate that chromosome gains and losses seems to be stochastic. Consequently, since each technique has its advantages and disadvantages, only integration of several molecular cytogenetic techniques for continuous analysis of hESC and hiPSC lines during culture can give reassurance of their chromosomal stability/constitution.
Aneuploidy screening
In this study, we examined the aneuploidy rates in hESCs and hiPSCs; FISH data indicate that hESC lines exhibit significant and pervasive mosaic aneuploidy, in comparison with controls. Aneuploidy rate detected in control group represents cells with abnormal number of chromosomes and might include background noise of FISH technique, known as false positive.
Aneuploidy rate differences remained significant between hESCs and controls, even when restricting the analysis to passages lower than 70 (<70), suggesting that accumulating changes occur relative early in culture conditions.
Recent study, published by Peterson et al, reported of significant levels of mosaic aneuploidy in all human pluripotent stem cells they examined. In similar to our findings of an average rate of 1.3% (±0.6) per chromosome, Peterson's group reported of 1.5–2% aneuploidy for each of the two FISH probes they used. If extrapolated for the remaining paired chromosomes, then the resultant level of mosaic aneuploidy revealed by FISH is consistent with their finding using G banding and SKY analysis, showing that the percentage of aneuploid cells ranged from 18% to as much as 35%.32 De-novo aberrations in hESC lines have been previously reported, some of them shows very fast culture take over.33 Here, we report high prevalence of aneuploidy in chromosomes 17 and 18, and although it is not statistically significant higher than other chromosomes, trisomy 17 aneuploidy is highly interesting as it was rarely reported in iPSCs. Significant difference was found in our research between monosomy and trisomy rate, suggesting that chromosome loss is more common. Prior studies highlighted chromosomes 12, 17, 20 and X as involved in most of the genomic aberrations12, 13 and both chromosomal gains and losses were frequently reported in cells from different sources. It is notable that, trisomy 12 is known to take over the culture in a few passages15, 34 but in our study, aneuploid cells carrying additional copy of chromosome 12 do not seem to be enriched in culture over time. Taken together, since chromosome gain and loss appears to be stochastic, with no significantly recurrent aneuploidy of specific chromosome, genome-wide analyses using CGH array or SNP array (and at a later stage – whole-genome sequencing and single-nucleotide polymorphism genotyping)7 may have some advantages over multi-FISH hybridizations as an improved standardized genetic screening of human ESCs and hiPSCs.
In this study, we also detected tetraploid cells that probably arise during in-vitro culture. Continuous cell lines are usually show a wide deviation range in chromosome number among individual cells in the population (ie, heteroploid) and a common feature of many continuous cell lines is the development of a subtetraploid chromosome number.35
The most likely possibility for the origin of those aneuploidies is that aneuploid cells arise during culture as a result of the alteration of one or more cells. Our observation of aneuploidy rate that increases over time supports this possibility. Lavon et al36 demonstrated the possibility that mosaicism may lead to one cell population, by the derivation of euploid hESCs from monosomy 21 embryos, which were in fact mosaic. They detected high rate of monosomy 21 mosaicism in early passages of hESCs and concluded that in higher passages the euploid cells took over the culture. Therefore, the mosaicism phenomenon should be monitored regularly to locate as early as possible any change in the cells.
Accumulating genomic changes over time, as presented in this study, means that the cells might loose their therapeutic value. This is crucial when considering transplantation of these cells. In this study, we found that aneuploidy rate in all cell lines (both hESCs and hiPSCs) increased over time, in direct correlation with the number of passages. A recent study compared early and late passages of hESC lines and reported about high rate of copy number variations and loss of heterozygocity changes.37 Taken together, these findings emphasize the need of tight surveillance of genomic integrity during long-term culture and the preference of low passages for clinical applications.
Although in all hESC and hiPSC lines aneuploidy cells were observed, in our research, statistical difference was found only between hESCs and control. HiPSCs and control showed no statistical difference. One of the explanations for the high aneuploidy rate in hESCs cells, compared with hiPSCs and controls, might lies in the possibility that ESCs guarantee rapid cell division by bypassing certain mechanisms of cell-cycle control and by that, enabling the survival of chromosomally aberrant cells. As it turns out, in early development, the strict requirements for cell growth are suspended to allow rapid cell proliferation38, 39 and is activated again when ESCs are induced to differentiate into embryoid bodies.40, 41 A recent study, conducted by Mayshar et al34, identified a substantial number of hiPS cell lines carrying full and partial chromosomal aberrations. To conclude, both hESCs and hiPSCs should be tightly monitored regarding their genomic stability.
Chromosome 1 aberration
A recurrent genomic aberration, involving an amplification of similar segment in chromosome 1 was found, independently, in one hESC (I4) line – ish cgh amp(1)(q21q32) and in one hiPSC (C3) line – ish cgh amp(1)(q21qter). While line I4 aberration was detected after identification of unexplained chromosome aberration using G banding (46,XX,ins(2;?)(p16;?)[2]/46,XX[18]) but with normal culture growth, line C3 aberration was detected simultaneity to alteration of the cells from colony growth to monolayer cell growth. The fact that hESC line and hiPSC line share a similar aberration might implies that gains of chromosome 1q may endow a clonal advantage in culture. Trisomy of entire chromosome 1 has been reported in human pluripotent stem cells as well as gains of small region of chromosome 1.12, 34, 37 A recent study reported about a recurrent chromosomal duplication of chromosome 1q in neural pluripotent stem cells,42 but duplication of almost the entire 1q arm had not been observed in pluripotent stem cells. Duplication of the chromosome segment of 1q11-1q32 is associated with advantages in proliferation and metastasis formation43 and data from several reports suggest that alterations in chromosome 1, and especially in the 1q region may have a significant role in disease evolution by providing a growth and/or survival advantage.44, 45 Until now, number of genes located on 1q region have been described to be associated with cell-cycle control and proliferation.46 It is possible that one or more of them are responsible for clonal advantage in culture. As we witnessed in the present study, the chromosomal aberration in line C3 was accompanied by change of growth from colonies to monolayer. As the characteristics of a cell line do not always remain stable and phenotype alterations might occur, regularly monitoring of morphologic features is also essential.35
Another finding in our study was a partial trisomy of the short arm of chromosome 1. The need to integrate several techniques is demonstrated here again, as CGH did not detect this aberration at passage 59 but we witness the change in passage 90 and passage 98 – ish cgh amp(1)(p32p34.1). One of the possibilities is that this change was present in a small mosaicism at an early passage, therefore CGH and G banding could not detect it, but FISH would probably have.
Conclusion
To conclude, the importance of complete validation of any stem cells destined for therapy cannot be underestimated.47 The low-grade mosaic aneuploidy and the recurrent genomic instability of chromosome 1 that were found in this manuscript illustrate the need for careful monitoring of the cells. Our findings demonstrate the phenomenon of genomic instability in stem cell lines, which increases over time. Without specific measures being taken to ensure genomic integrity and identity, their use as a cellular source for cell therapy may be compromised for safety reasons. The present study emphasizes the significance of the use of several molecular cytogenetic methods when studying genomic stability of hESC and hiPSC lines. It is important and of a great value to integrate these methods into a plan for routine cell line quality control.
References
Keller G : Embryonic stem cells differentiation: emergence of a new era in biology and medicine. Genes Dev 2005; 19: 1129–1155.
Gokhale PJ, Andrews PW : A prospective on stem cells research. Semin Reprod Med 2006; 24: 289–297.
Evans MJ, Kaufman MH : Establishment in culture of pluripotential cells from mouse embryos. Nature 1981; 292: 154–156.
Thomson JA, Itskovitz-Eldor J, Shapiro SS et al. Embryonic stem cell lines derived from human blastocysts. Science 1998; 282: 1145–1147.
Takahashi K, Tanabe K, Ohnuki M et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 2007; 131: 861–872.
Lian Q, Chow Y, Esteban MA, Pei D, Tse HF : Future perspective of induced pluripotent stem cells for diagnosis, drug screening and treatment of human diseases. Thromb Haemost 2010; 104: 39–44.
Gore A, Li Z, Fung HL et al. Somatic coding mutations in human induced pluripotent stem cells. Nature 2011; 471: 63–67.
Grandela C, Wolvetang E : HESC adaptation, selection and stability. Stem Cell Rev 2007; 3: 183–191.
Meisner LF, Johnson JA : Protocols for cytogenetic studies of human embryonic stem cells. Methods 2008; 45: 133–141.
Hoffman LM, Carpenter MK : Human embryonic stem cell stability. Stem Cell Rev 2005; 1: 139–144.
Amit M, Chebath J, Margulets V et al. Suspension culture of undifferentiated human embryonic and induced pluripotent stem cells. Stem Cell Rev 2010; 6: 248–259.
Baker DE, Harrison NJ, Maltby E et al. Adaptation to culture of human embryonic stem cells and oncogenesis in vivo. Nat Biotechnol 2007; 25: 207–215.
Draper JS, Smith K, Gokhale P et al. Recurrent gain of chromosomes 17q and 12 in cultured human embryonic stem cells. Nat Biotechnol 2004; 22: 53–54.
Maitra A, Arking DE, Shivapurkar N et al. Genomic alterations in cultured human embryonic stem cells. Nat Genet 2005; 37: 1099–1103.
Mitalipova MM, Rao RR, Hoyer DM et al. Preserving the genetic integrity of human embryonic stem cells. Nat Biotechnol 2005; 23: 19–20.
Lefort N, Feyeux M, Bas C et al. Human embryonic stem cells reveal recurrent genomic instability at 20q11.21. Nat Biotechnol 2008; 26: 1364–1366.
Aviram-Goldring A, Daniely M, Dorf H, Chaki R, Goldman B, Barkai G : Use of interphase fluorescence in situ hybridization in third trimester fetuses with anomalies and growth retardation. Am J Med Genet 1999; 87: 203–206.
Pinkel D, Albertson DG : Comparative genomic hybridization. Annu Rev Genomics Hum Genet 2005; 6: 331–354.
Amit M, Itskovitz-Eldor J : Derivation and spontaneous differentiation of human embryonic stem cells. J Anat 2002; 200 (Part 3): 225–232.
Germanguz I, Sedan O, Zeevi-Levin N et al. Molecular characterization and functional properties of cardiomyocytes derived from human inducible pluripotent stem cells. J Cell Mol Med 2011; 15: 38–51.
Amit M, Carpenter MK, Inokuma MS et al. Clonally derived human embryonic stem cell lines maintain pluripotency and proliferative potential for prolonged periods of culture. Dev Biol 2000; 227: 271–278.
Bates SE : Classical cytogenetics: karyotyping techniques. Methods Mol Biol 2011; 767: 177–190.
Verma RS, Babu A : Human Chromosomes: Manual of Basic Techniques. Pergamon Press, 1989, pp 16–18.
Munne S, Márquez C, Magli C, Morton P, Morrison L : Scoring criteria for preimplantation genetic diagnosis of numerical abnormalities for chromosomes X, Y, 13, 16, 18 and 21. Mol Hum Reprod 1998; 4: 863–870.
Munne S, Weier HU : Simultaneous enumeration of chromosomes 13, 18, 21, X, and Y in interphase cells for preimplantation genetic diagnosis of aneuploidy. Cytogenet Cell Genet 1996; 75: 263–270.
Fragouli E, Wells D, Doshi A et al. Cytogenetic investigation of oocytes from a young cancer patient with the use of comparative genomic hybridisation reveals meiotic errors. Prenat Diagn 2006; 26: 71–76.
Israeli O, Gotlieb WH, Friedman E et al. Familial vs sporadic ovarian tumors: characteristic genomic alterations analyzed by CGH. Gynecol Oncol 2003; 90: 629–636.
Kirchhoff M, Gerdes T, Maahr J et al. Deletions below 10 megabasepairs are detected in comparative genomic hybridization by standard reference intervals. Genes Chromosomes Cancer 1999; 25: 410–413.
Catalina P, Cobo F, Cortés JL et al. Conventional and molecular cytogenetic diagnostic methods in stem cell research: a concise review. Cell Biol Int 2007; 31: 861–869.
Inzunza J, Sahlén S, Holmberg K et al. CGH and karyotyping of human embryonic stem cells reveals the occurrence of an isodicentric X chromosome after long-term cultivation. Mol Hum Reprod 2004; 10: 461–466.
Amps K, Andrews PW, Anyfantis G et al. Screening ethnically diverse human embryonic stem cells identifies a chromosome 20 minimal amplicon conferring growth advantage. Nat Biotechnol 2011; 29: 1132–1144.
Peterson SE, Westra JW, Rehen SK et al. Normal human pluripotent stem cell lines exhibit pervasive mosaic aneuploidy. PLoS One 2011; 6: e23018.
Spits C, Mateizel I, Geens M et al. Recurrent chromosomal abnormalities in human embryonic stem cells. Nat Biotechnol 2008; 26: 1361–1363.
Mayshar Y, Ben-David U, Lavon N et al. Identification and classification of chromosomal aberrations in hiPSCs. Cell Stem Cell 2010; 7: 521–531.
Ian Freshney R : Culture of Animal Cells: A Manual of Basic Technique and Specialized Applications, Chapter 17 - Transformation and Immortalization. 6th edn, Wiley-Blackwell: Hoboken, NJ, USA, 2005.
Lavon N, Narwani K, Golan-Lev T et al. Derivation of euploid human embryonic stem cells from aneuploid embryos. Stem Cells 2008; 26: 1874–1882.
Närvä E, Autio R, Rahkonen N et al. High-resolution DNA analysis of human embryonic stem cell lines reveals culture-induced copy number changes and loss of heterozygosity. Nat Biotechnol 2010; 28: 371–377.
Stead E, White J, Faast R et al. Pluripotent cell division cycles are driven by ectopic Cdk2, cyclin A/E and E2F activities. Oncogene 2002; 21: 8320–8333.
Fluckiger AC, Marcy G, Marchand M et al. Cell Cycle features of primate embryonic stem cells. Stem Cells 2006; 24: 547–556.
White J, Stead E, Faast R et al. Pathway and establishment of cell cycle-regulated cyclin-dependent kinase activity during embryonic stem cell differentiation. Mol Biol Cell 2005; 16: 2018–2027.
Henning Ulrich Perspectives of Stem Cells, Chapter 6 - Aneuploidy in Embryonic Stem Cells. Springer Publishing Company: New York, NY, USA, 2010, pp 73–87.
Varela C, Denis JA, Polentes J et al. Recurrent genomic instability of chromosome 1q in neural derivatives of hESCs. J Clin Invest 2012; 122: 569–574.
Ghose T, Lee CL, Fernandez LA et al. Role of 1q trisomy in tumorigenicity, growth, and metastasis of human leukemic B-cell clones in nude mice. Cancer Res 1990; 50: 3737–3742.
Shaughnessy JD, Zhan F, Burington BE et al. A validated gene expression model of high-risk multiple myeloma is defined by deregulated expression of genes mapping to chromosome 1. Blood 2007; 109: 2276–2284.
Hanamura I, Stewart JP, Huang Y et al. Frequent gain of chromosome band 1q21 in plasma-cell dyscrasias detected by FISH: incidence increases from MGUS to relapsed myeloma and is related to prognosis and disease progression following tandem stem-cell transplantation. Blood 2006; 108: 1724–1732.
Carpten JD, Robbins CM, Villablanca A et al. Encoding parafibromin, is mutated in yperparathyroidism-jaw tumor syndrome. Nat Genet 2002; 32: 676–680.
Stephenson E, Ogilvie CM, Patel H et al. Safety paradigm: genetic evaluation of therapeutic grade human embryonic stem cells. J R Soc Interface 2010; 7 (Suppl 6): S677–S688.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work was performed in partial fulfillment of the requirements for a PhD degree of Michal Dekel, Sackler Faculty of medicine, Tel Aviv University, Ramat Aviv, Israel.
Supplementary Information accompanies the paper on European Journal of Human Genetics website
Rights and permissions
About this article
Cite this article
Dekel-Naftali, M., Aviram-Goldring, A., Litmanovitch, T. et al. Screening of human pluripotent stem cells using CGH and FISH reveals low-grade mosaic aneuploidy and a recurrent amplification of chromosome 1q. Eur J Hum Genet 20, 1248–1255 (2012). https://doi.org/10.1038/ejhg.2012.128
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2012.128
Keywords
This article is cited by
-
Towards physiologically relevant human pluripotent stem cell (hPSC) models of Parkinson’s disease
Stem Cell Research & Therapy (2021)
-
Induced Pluripotent Stem Cells (iPSCs) Provide a Potentially Unlimited T Cell Source for CAR-T Cell Development and Off-the-Shelf Products
Pharmaceutical Research (2021)
-
CRISPR System: A High-throughput Toolbox for Research and Treatment of Parkinson’s Disease
Cellular and Molecular Neurobiology (2020)
-
Cytogenetic Analysis of the Results of Genome Editing on the Cell Model of Parkinson’s Disease
Bulletin of Experimental Biology and Medicine (2018)
-
Low-grade chromosomal mosaicism in human somatic and embryonic stem cell populations
Nature Communications (2014)