Abstract
Background/Objectives: This study investigates determinants of sleep duration and its impact on nutritional status, resting energy expenditure (REE), cardiometabolic risk factors and hormones in children/adolescents.
Subjects/Methods: In 207 girls and 207 boys (13.0±3.4 (6.1–19.9) years) body mass index standard deviation score (BMI SDS), waist circumference (WC) z-score, body composition (air-displacement plethysmography), REE (ventilated hood system; n=312) and cardiometabolic risk factors/hormones (n=250) were assessed. Greater than 90th percentile of BMI/WC references was defined as overweight/overwaist. Sleep duration, media consumption (TV watching/computer use), physical activity, dietary habits, parental BMI, socio-economic status and early infancy were assessed by questionnaire. Short sleep was defined as <10 h per day for children <10 years and otherwise <9 h per day.
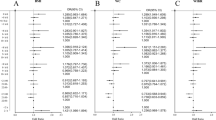
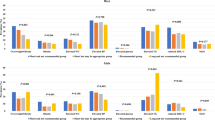
Results: Total 15.9% participants were overweight, mean sleep duration was 8.9±1.3 h per day. Age explained most variance in sleep (girls: 57.0%; boys: 41.2%) besides a high nutrition quality score (girls: 0.9%) and a low media consumption (boys: 1.3%). Sleep was inversely associated with BMI SDS/WC z-score (girls: r=−0.17/−0.19, P<0.05; boys: r=−0.21/−0.20, P<0.01), which was strengthened after adjusting for confounders. Short vs long sleep was associated with 5.5-/2.3-fold higher risks for obesity/overwaist (girls). After adjusting for age, REE (adjusted for fat-free mass) was positively associated with sleep in boys (r=0.16, P<0.05). Independently of age and WC z-score, short sleep was associated with lower adiponectin levels in boys (11.7 vs 14.4 μg/ml, P<0.05); leptin levels were inversely related to sleep in girls (r=−0.23, P<0.05). Homoeostasis model assessment–insulin resistance (r=−0.20, P<0.05) and insulin levels (r=−0.20, P<0.05) were associated with sleep (girls), which depended on WC z-score.
Conclusions: Age mostly determined sleep. Short sleep was related to a higher BMI SDS/WC z-score (girls/boys), a lower REE (boys), higher leptin (girls) and lower adiponectin levels (boys).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bader N, Bosy-Westphal A, Dilba B, Müller MJ (2005). Intra- and interindividual variability of resting energy expenditure in healthy male subjects—biological and methodological variability of resting energy expenditure. Br J Nutr 94, 843–849.
Benefice E, Garnier D, Ndiaye G (2004). Nutritional status, growth and sleep habits among Senegalese adolescent girls. Eur J Clin Nutr 58, 292–301.
Bosy-Westphal A, Danielzik S, Becker C, Geisler C, Onur S, Korth O et al. (2005). Need for optimal body composition data analysis using air-displacement plethysmography in children and adolescents. J Nutr 135, 2257–2262.
Bosy-Westphal A, Geisler C, Onur S, Korth O, Selberg O, Schrezenmeir J et al. (2006). Value of body fat mass vs. anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes 30, 475–483.
Chaput JP, Brunet M, Tremblay A (2006). Relationship between short sleeping hours and childhood overweight/obesity: results from the ‘Québec en Forme’ Project. Int J Obes 30, 1080–1085.
Chaput JP, Després JP, Bouchard C, Tremblay A (2007). Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Québec Family Study. Obesity 15, 253–261.
Chaput JP, Tremblay A (2007). Does short sleep duration favor abdominal adiposity in children? Int J Pediatr Obes 2, 188–191.
Chen X, Beydoun MA, Wang Y (2008). Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity 16, 265–274.
Danielzik S, Czerwinski-Mast M, Langnäse K, Dilba B, Müller MJ (2004). Parental overweight, socioeconomic status and high birth weight are the major determinants of overweight and obesity in 5–7y-old children: baseline data of the Kiel Obesity Prevention Study. Int J Obes Relat Disord 28, 1494–1502.
Dollman J, Ridley K, Olds T, Lowe E (2007). Trend in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Pediatr 96, 1011–1014.
Eisenmann JC, Ekkekakis P, Holmes M (2006). Sleep duration and overweight among Australian children and adolescents. Acta Paediatr 95, 956–963.
Flint J, Kothare SV, Zihlif M, Suarez E, Adams R, Legido A et al. (2007). Association between inadequate sleep and insulin resistance in obese children. J Pediatr 150, 364–369.
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE et al. (2006). Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 29, 1009–1014.
Hannon TS, Janosky J, Arslanian SA (2006). Longitudinal study of physiologic insulin resistance and metabolic changes of puberty. Pediatr Res 60, 759–763.
Hassink SG, Sheslow DV, De Lancey E, Opentanova I, Considine RV, Caro JF (1996). Serum leptin concentrations in children with obesity: relationship to gender and development. Pediatrics 98, 201–203.
Iglowstein I, Jenni OG, Molinari L, Largo RH (2003). Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 111, 302–307.
Knutson KL (2005a). Sex differences in the association between sleep and body mass index in adolescents. J Pediatr 147, 830–834.
Knutson KL (2005b). The association between pubertal status and sleep duration and quality among a nationally representative sample of U.S. adolescents. Am J Hum Biol 17, 418–424.
Koban M, Swinson KL (2005). Chronic REM-sleep deprivation of rats elevates metabolic rate and increases UCP1 gene expression in brown adipose tissue. Am J Physiol Endocrinol Metab 289, 68–74.
Kotani K, Sakane N, Saiga K, Kato M, Ishida K, Kato Y et al. (2007). Serum adiponectin levels and lifestyle factors in Japanese men. Heart Vessels 22, 291–296.
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V et al. (2001). Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschrift Kinderheilkunde 149, 807–818.
Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH (2007). Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 120, 1020–1029.
Locard E, Mamelle N, Billete A, Miginiac M, Munoz F, Rey S (1992). Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord 16, 721–729.
Mast M, Kortzinger I, Müller MJ (1998). Ernährungsverhalten und Ernährungszustand 5-7-jähriger Kinder in Kiel. Aktuelle Ernährungsmedizin 23, 282–288.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985). Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419.
McAdams MA, Van Dam RM, Hu FB (2007). Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity 15, 188–196.
McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM (2006). Body fat reference curves for children. Int J Obes 30, 598–602.
McCarthy HD, Jarrett KV, Crawley HF (2001). The development of waist circumference percentiles in British children aged 5.0–16.9y. Eur J Clin Nutr 55, 902–907.
Mercer PW, Merritt SL, Cowell JM (1998). Differences in reported sleep need among adolescents. J Adolesc Health 23, 259–263.
Patel SR, Hu FB (2008). Short sleep duration and weight gain: a systematic review. Obesity 16, 643–653.
Ravussin E, Bogardus C (1989). Relationship of genetics, age and physical fitness to daily energy expenditure and fuel utilization. Am J Nutr 49, 968–975.
Redline S, Storfer-Isser A, Rosen CL, Johnson NL, Kirchner HL, Emancipator J et al. (2007). Association between metabolic syndrome and sleep-disordered breathing in adolescents. Am J Respir Crit Care Med 176, 401–408.
Savoye M, Dziura J, Castle J, DiPietro L, Tamborlane WV, Caprio S (2002). Importance of plasma leptin in predicting future weight gain in obese children: a two-and-a-half-year longitudinal study. Int J Obes 26, 942–946.
Sekine M, Yamagami T, Handa K, Saito T, Nanri S, Kawaminami K et al. (2002). A dose–response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Dev 28, 163–170.
Sivak M (2006). Sleeping more as a way to lose weight. Obesity Rev 7, 295–296.
Spiegel K, Knutson K, Leprould R, Tasali E, Van Cauter E (2005). Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol 99, 2008–2019.
Spiegel K, Leproult R, L'hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E (2004a). Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab 89, 5762–5771.
Spiegel K, Leproult R, Van Cauter E (1999). Impact of sleep dept on metabolic and endocrine function. Lancet 354, 1435–1439.
Spiegel K, Tasali E, Penev P, van Cauter E (2004b). Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141, 846–850.
Taheri S, Lin L, Austin D, Young T, Mignot E (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1, e62.
Verhulst SL, Schrauwen N, Haentjens D, Rooman RP, Van Gaal L, De Backer WA et al. (2008). Sleep duration and metabolic dysregulation in overweight children and adolescents. Arch Dis Child 93, 89–90.
von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B (2002). Reduced risk for overweight and obesity in 5-and 6-y-old children by duration of sleep—a cross-sectional study. Int J Obes 26, 710–716.
WHO (1995). Physical Status: The Use and Interpretation of Anthropometry Technical Report Series WHO: Geneva.
Acknowledgements
This work was supported by Bundesministerium für Bildung und Forschung (project 6.1.2 Network Kiel: Dietary Fat and Metabolism).
Author information
Authors and Affiliations
Corresponding author
Additional information
Contributors: Writing of the manuscript, BH and MJM; study design, AB-W and MJM; data collection, BH, AB-W and FB; data analysis, BH, AB-W, US, MP, JS, HM; discussion of data, BH, AB-W, SP-D and MJM. All contributors helped with the revision of the paper.
Rights and permissions
About this article
Cite this article
Hitze, B., Bosy-Westphal, A., Bielfeldt, F. et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr 63, 739–746 (2009). https://doi.org/10.1038/ejcn.2008.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2008.41
Keywords
This article is cited by
-
Shorter sleep among adolescents is associated with lower fruit and vegetable consumption the following day
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
Association between overweight, obesity and sleep duration and related lifestyle behaviors is gender and educational stages dependent among children and adolescents aged 6-17 years: a cross-sectional study in Henan
BMC Public Health (2022)
-
Association between free-living sleep and memory and attention in healthy adolescents
Scientific Reports (2020)
-
Screen viewing behavior and sleep duration among children aged 2 and below
BMC Public Health (2019)
-
Childhood sleep duration modifies the polygenic risk for obesity in youth through leptin pathway: the Beijing Child and Adolescent Metabolic Syndrome cohort study
International Journal of Obesity (2019)