Abstract
There is evidence to suggest that follicle-stimulating hormone (FSH) can facilitate the neovascularization of ovarian cancers by increasing vascular endothelial growth factor (VEGF) expression in cancer cells, although the underlying molecular mechanism of this process is not well known. Therefore, we investigated the effect of FSH on VEGF expression in the ovarian cancer cell lines SKOV-3 and ES-2. Treatment with FSH significantly increased VEGF expression in a dose- and time-dependent manner. In addition, FSH treatment enhanced the expression of survivin and hypoxia-inducible factor-1 (HIF-1α). Knockdown of survivin or HIF-1α suppressed VEGF expression, but only knockdown of survivin inhibited FSH-stimulated VEGF expression. Pretreatment with LY294002, a phosphoinositide 3-kinase (PI3K)/AKT inhibitor, neutralized the enhanced expression of survivin induced by FSH, but treatment with U0126, a mitogen-activated protein kinase/extracellular signal-regulated kinase inhibitor, had no such effect. We further showed that ovarian serous cystadenocarcinoma samples had much higher incidence of positive AKT and phosphorylated AKT (pAKT) protein staining than did benign ovarian cystadenoma samples (p < 0.01). The 5-year survival rate was only about 15% in patients with ovarian serous cystadenocarcinoma who had AKT and pAKT expression, whereas it was about 80% in those who did not have AKT or pAKT expression. Taken together, these results indicate that FSH increases the expression of VEGF by upregulating the expression of survivin, which is activated by the PI3K/AKT signaling pathway. Understanding the role of the PI3K/AKT pathway in FSH-stimulated expression of survivin and VEGF will be beneficial for evaluating the prognosis for patients with ovarian serous cystadenocarcinoma and for pursuing effective treatment against this disease.
Similar content being viewed by others
Introduction
At present, ovarian epithelial cancer is the leading killer among all gynecological malignancies 1. Ovarian serous cystadenocarcinoma, accounting for 56% of all ovarian epithelial cancers 2, is one of the histopathological types with a particularly poor prognosis. Most deaths due to ovarian epithelial cancer are associated with its dissemination, where the development of disseminated malignancy is known to be related to neovascularization. However, the factors that regulate the angiogenic process of ovarian cancer are poorly understood. Vascular endothelial growth factor (VEGF) is identified as a major mediator of angiogenesis. It can induce endothelial cells to undergo angiogenesis, which facilitates the development of some diseases 3, 4, and also plays an important role in the regulation of tumor angiogenesis 5, 6.
Previous studies have proven that hypoxia-inducible factor-1α (HIF-1α) stimulates VEGF expression, further improving blood and oxygen supplies, which promote carcinogenesis and oncogenesis 7, 8, 9, 10. HIF-1 is a heterodimeric transcription factor composed of two subunits: HIF-1α and HIF-1β. The former is the oxygen regulatory subunit for HIF-1, which is induced by hypoxia and determines the activity of HIF-1, whereas the latter determines its stability. Under hypoxic conditions, HIF-1α degradation is impeded. HIF-1α then enters the nucleus from the cytoplasm of cells, where it binds with HIF-1β and produces stable HIF-1, representing a series of adaptive reactions to hypoxia. Other investigators have found that, in addition to the HIF-1α pathway, there are non-HIF-1α-dependent regulation pathways that regulate VEGF expression 11, 12. Survivin is a newly discovered apoptotic inhibitor belonging to the inhibitor of apoptosis protein (IAP) family, and has been shown to both inhibit tumor cell apoptosis and promote tumor proliferation. Survivin is overexpressed in 60 cancer cell lines and in most human tumor types, including lung, breast, stomach, liver, bladder, and ovarian cancer 12. Some studies found that survivin promoted angiogenesis of endothelial cells and decreased patient survival 13, 14, 15, 16.
Ovarian epithelial cancer is more common in conditions with elevated follicle-stimulating hormone (FSH) and luteinizing hormone (LH), such as in postmenopausal women or in women who have received treatment for induction of ovulation 17, 18. Additionally, reduced risk for ovarian cancer is associated with multiple pregnancies, breast-feeding, oral contraceptives, and estrogen replacement therapy, which are related to lower levels of and reduced exposure to FSH and LH 19, 20. The FSH receptor (FSHR) and LH receptor (LHR) have been shown in normal and neoplastic ovarian surface epithelium (OSE) cells 21, 22. Moreover, levels of ovarian and peritoneal FSH and LH seem to be elevated in ovarian cancer patients 23, 24. Although the mutagenic effect of FSH is still controversial, the proliferative effect has been shown in OSE and in ovarian cancer in vitro 15, 25, 26, 27. It has been reported that FSH promotes the metastasis of ovarian epithelial cancer through the protein kinase A/phosphoinositide 3-kinase (PI3K) pathway 28. However, little is known about the exact mechanism of FSH stimulation in other aspects of ovarian cancer, like VEGF expression. In light of this, we hypothesized that FSH may modulate VEGF expression, and we performed a study to examine the effect of FSH stimulation of VEGF expression in ovarian cancer cell lines, as well as its relationship to HIF-1α and survivin. We also examined whether this effect functioned via PI3K/AKT or another signal transduction pathway. In addition, to evaluate the clinical significance of AKT, we analyzed the expression of AKT and phosphorylated AKT (pAKT) in ovarian cancer specimens and the relationship between AKT/pAKT expression and the prognosis for ovarian cancer.
Results
FSH stimulation of VEGF expression in SKOV-3 and ES-2 cells
We stimulated SKOV-3 and ES-2 cells with FSH at different concentrations and for different time courses. Western blot analysis showed that VEGF expression levels increased gradually along with the FSH concentration in SKOV-3 cells, peaked at an FSH concentration of 40 mIU/mL, and then began to decline slightly, indicating a dose-dependent correlation (Figure 1A). When we stimulated SKOV-3 cells with 40 mIU/mL of FSH for 0, 12, 24, 48, 72, or 96 h, VEGF expression in the 24-, 48-, and 72-h groups of cells increased in comparison to the control group, indicating a time-dependent correlation. VEGF expression peaked at 48 h after stimulation with 40 mIU/mL FSH (Figure 1B).
FSH stimulation of VEGF expression in SKOV-3 and ES-2 cells. The level of VEGF protein expression in both cell types was determined using western blot analysis with an anti-VEGF antibody after FSH stimulation at different doses and time points. (A) Dose response: VEGF protein expression in SKOV-3 cells after stimulation with 0 to 160 mIU/mL FSH. (B) Time response: VEGF protein expression in SKOV-3 cells after stimulation with 40 mIU/mL FSH for 0-96 h. (C) Dose response: VEGF protein expression in ES-2 cells after stimulation with 0-160 mIU/mL FSH. (D) Time response: VEGF protein expression in ES-2 cells after stimulation with 40 mIU/mL FSH for 0-96 h.
Measurement of VEGF expression in ES-2 cells showed similar patterns (Figure 1C and 1D), but the stimulating effect of FSH was more apparent in SKOV-3 cells. We used the stimulation conditions of 48 h and 40 mIU/mL FSH, which produced the most obvious effects, to conduct further experiments for evaluating FSH-stimulated VEGF expression in SKOV-3 cells. We also found that FSH stimulated VEGF secretion in the supernatants and mRNA, indicating a time- and dose-dependent correlation in ELISA and RT-PCR analysis, respectively (data not shown).
FSH stimulation of survivin and HIF-1α expression in SKOV-3 cells
To investigate the correlation between FSH, survivin, and HIF-1α, we stimulated SKOV-3 cells with 40 mIU/mL FSH for 0, 8, 16, 24, 48, or 72 h. Western blot analysis showed that the survivin and HIF-1α expression levels increased gradually over time in SKOV-3 cells, peaked at 24 h, and then declined slightly, indicating a time-dependent correlation (Figure 2A and 2B).
Elevated (A) survivin and (B) HIF-1α expression in SKOV-3 cells after stimulation with FSH treatment. The level of survivin and HIF-1α protein expression in these cells was determined using western blot analysis with anti-survivin and anti-HIF-1α antibodies after stimulation with 40 mIU/mL FSH at different time points. GAPDH was used as a loading control.
Knockdown of survivin and HIF-1α expression in SKOV-3 cells by RNA interference (RNAi)
Three recombinant plasmids of survivin RNAi (pRNAT-suv1, pRNAT-suv2, and pRNAT-suv3) and one negative control plasmid (pRNAT-neg) were constructed and tested for their ability to knock down survivin expression in SKOV-3 cells. Transfection of SKOV-3 cells with pRNAT-suv2 resulted in a reproducible 70-80% decrease in the level of expression of survivin at both the mRNA and protein levels (verified by RT-PCR analysis and western blot analysis, respectively), whereas transfection with pRNAT-neg, pRNAT-suv1, or pRNAT-suv3 failed to produce such effects. We also found that transfection of SKOV-3 cells with pRNAT-hif1 knocked down HIF-1α mRNA and protein expression, whereas transfection with pRNAT-neg, pRNAT-hif2, or pRNAT-hif3 did not do so. As a control, transfection with the two effective plasmids (pRNAT-suv2 and pRNAT-hif1) failed to knock down the expression of the unrelated protein GAPDH (data not shown).
Inhibition of VEGF expression in SKOV-3 cells by survivin and HIF-1α RNAi
Based on the experimental results described above, we used RNAi to determine the influence of survivin RNAi and HIF-1α RNAi on the expression of VEGF and to examine the FSH-VEGF correlation. We observed that transfection of SKOV-3 cells with pRNAT-hif1 specifically downregulated HIF-1α mRNA and protein expression, but that transfection with pRNAT-suv2 downregulated both survivin and HIF-1α mRNA and protein expression (Figure 3A and 3B). Expression of VEGF mRNA and protein in the SKOV-3 cells decreased when survivin or HIF-1α was downregulated (Figure 3A and 3B).
Inhibition of VEGF expression in SKOV-3 cells by survivin RNAi and HIF-1α RNAi. (A) HIF-1α, survivin, and VEGF protein expression detected using western blot analysis with anti-survivin, anti-HIF-1α, and anti-VEGF antibodies without FSH stimulation. GAPDH was used as a loading control. The signal was semiquantitatively measured using the Odyssey infrared fluorescence scanning system. The number under each blot is the ratio of each signal to GAPDH. (B) HIF-1α, survivin, and VEGF mRNA expression detected using real-time PCR without FSH stimulation. (C) HIF-1α, survivin, and VEGF protein expression detected using western blot analysis with anti-survivin, anti-HIF-1α, and anti-VEGF antibodies with FSH stimulation. GAPDH was used as a loading control. The signal was semiquantitatively measured using the Odyssey infrared fluorescence scanning system. The number under each blot is the ratio of each signal to GAPDH. (D) HIF-1α, survivin, and VEGF mRNA expression detected using real-time PCR analysis with FSH stimulation. Control: transfection with reagents only; RNAi-neg: transfection with pRNAT-neg. **p < 0.01 compared with control or RNAi-neg; #p < 0.01: no FSH compared with stimulation with FSH; *p < 0.01 compared with control + FSH or RNAi-neg + FSH.
Under the FSH-stimulation conditions (40 mIU/mL for 48 h), both VEGF mRNA and protein expression were upregulated (Figure 3C and 3D). Survivin RNAi blocked this increase, whereas HIF-1α RNAi had no effect on it, suggesting that interference with survivin expression leads to antagonism of FSH-stimulated VEGF expression, whereas interference with HIF-1α expression has no such effect (Figure 3C and 3D). In addition, expression of HIF-1α mRNA and protein in SKOV-3 cells decreased when survivin was downregulated under the FSH-stimulation conditions, while inhibition of HIF-1α by RNAi could not reduce the expression of survivin mRNA and protein (Figure 3C and 3D)
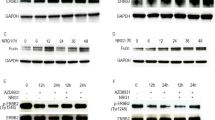
FSH may stimulate survivin expression through the PI3K/AKT signal transduction pathway
We found that FSH stimulation of SKOV-3 and ES-2 cells significantly increased the expression of pAKT in these cells, whereas it had no obvious effect on extracellular signal-regulated kinase (ERK) phosphorylation (pERK) (Figure 4A and 4B). We also found that transfection of SKOV-3 and ES-2 with pRNAT-akt2 downregulated AKT mRNA and protein expression, whereas transfection with pRNAT-neg, pRNAT-akt1 or pRNAT-akt3 had no such effects (data not shown). Treatment with the specific PI3K inhibitor LY294002 or transfection with pRNAT-akt2 antagonized the enhancement effects of FSH on pAKT and survivin expression in SKOV-3 and ES-2 cells, but treatment with the specific ERK inhibitor U0126 only decreased the pERK expression and did not affect survivin expression (Figure 4C–4F).
Expression of pAKT/AKT, pERK/ERK, and survivin. FSH stimulated pAKT but not pERK expression in (A) SKOV-3 cells and (B) ES-2 cells over time. AKT RNAi and the PI3K/AKT inhibitor LY294002 eliminated the enhancement effects of FSH on survivin expression in (C) SKOV-3 cells and (D) ES-2 cells. The MAPK/ERK inhibitor U0126 did not alter the enhancement effects of FSH on survivin expression in (E) SKOV-3 cells or (F) ES-2 cells. Control: transfection with reagents only; RNAi-neg: transfection with pRNAT-neg.
Expression of AKT and pAKT correlates with poor prognosis in patients with ovarian serous cystadenocarcinoma
To investigate the clinical significance of AKT and pAKT expression in ovarian cancer, we examined their expression in ovarian serous cystadenoma, ovarian borderline serous cystadenoma, ovarian clear cell carcinoma, and ovarian serous cystadenocarcinoma samples using immunohistochemistry. Our results showed that 81% (21 of 26) of ovarian serous cystadenocarcinoma samples, 28% (5 of 18) of ovarian borderline serous cystadenomas and 5% (1 of 21) of ovarian serous cystadenoma samples were positive for AKT, and that 77% (20 of 26) of ovarian serous cystadenocarcinoma samples, 22% (4 of 18) of ovarian borderline serous cystadenomas and 19% (4 of 21) of ovarian serous cystadenomas were positive for pAKT. When compared with ovarian serous cystadenoma samples, ovarian serous cystadenocarcinoma samples had much higher rates of AKT and pAKT protein expression (p < 0.01) (Tables 1 and 2). Also, we detected much higher levels of AKT and pAKT protein expression in ovarian serous cystadenocarcinoma samples than in the other samples (Figure 5). We examined whether the expression of AKT or pAKT correlated with the upregulation of VEGF and survivin expression in the ovarian serous cystadenocarcinoma specimens. We observed that the expression of both AKT and pAKT was significantly correlated with the expression of survivin (Pearson correlation coefficient R > 0.9; p < 0.05), but not with the expression of VEGF.
AKT and pAKT expression in ovarian serous tumor tissue samples. Shown are representative cases of (A) ovarian benign serous cystadenoma, (B) ovarian borderline serous cystadenoma, (C) ovarian serous cystadenocarcinoma (negative for AKT and pAKT), and (D) ovarian serous cystadenocarcinoma (positive for AKT and pAKT).
Furthermore, among the ovarian serous cystadenocarcinoma specimens, AKT expression levels were higher in grade 2 and 3 tumors than in grade 1 tumors (p < 0.01). However, AKT expression in the ovarian serous cystadenocarcinoma specimens was not found to be correlated with other clinical pathological parameters, such as age, disease stage, or presence of lymph node metastasis (Table 1). We found almost the same pattern of pAKT correlation with clinical pathological parameters in the ovarian serous cystadenocarcinoma specimens (Table 2).
The prognostic significance of AKT and pAKT expression was evaluated in the 26 samples of ovarian serous cystadenocarcinoma. We observed strong correlations between AKT/pAKT expression and the 2-year and 5-year survival rates (p < 0.01) in the ovarian serous cystadenocarcinoma cases (Tables 1 and 2). The 5-year survival rate was only about 14% in the 21 patients with ovarian serous cystadenocarcinoma who showed positive AKT expression, whereas it was 80% in the 5 patients who did not have AKT expression. Also, the 5-year survival rate was only 15% in the 20 patients with ovarian serous cystadenocarcinoma who showed positive pAKT expression, but was 67% in the 6 patients who did not have pAKT expression (Figure 6, Tables 1 and 2).
In the ovarian clear cell carcinoma samples, AKT positive rates were not high, with only 12% of the samples positive for AKT, whereas pAKT-positive rates were much higher, with 94% of the samples positive for pAKT. We found that expression of both AKT and pAKT in these specimens was not correlated with clinical pathological parameters such as age, disease stage, presence of lymph node metastasis, or the 2-year and 5-year survival rates (data not shown).
Discussion
Because it has been hypothesized that FSH increases the risk of ovarian malignancy and that pregnancies and oral contraceptives protect the ovary by suppressing secretion of such hormones 29, numerous studies have examined the roles of FSH and/or LH in tumorigenesis. These hormones have been shown to stimulate the growth of normal and immortalized OSE (IOSE) and several ovarian cancer cell lines in a dose- and time-dependent manner in vitro 30, 31, 32, 33. Although these observations have shown the role of FSH in initiation and proliferation of ovarian cancer, the contribution of FSH to other aspects of cancer progression, such as neovascularization, is poorly understood. FSH has been reported to enhance tumor invasion and adhesion by regulating the expression of matrix metalloproteinases (MMP), as well as integrin subunit α (v) and CD44 in ovarian cancer cells 28, 34. VEGF can induce angiogenesis and promote tumor neovascularization. Thus, we hypothesized that FSH may affect ovarian cancer angiogenesis by regulating VEGF expression.
The effect of FSH stimulation on VEGF expression was examined primarily using ELISA, western blot and RT-PCR analysis. Treatment with FSH significantly enhanced the expression of VEGF. The elevated FSH may be effective in promoting tumor neovascularization in vivo and VEGF expression in human ovarian cancer cells in vitro 35, 36. However, little was known about the mechanism of FSH stimulation on VEGF expression. Other studies showed HIF-1α and survivin may play a role in VEGF expression 7, 8, 9, 10, 13, 14, 15, 16, and it had also been shown that FSH induces HIF-1α and survivin expression 37, 38, 39. In this study, we showed that treatment with FSH also increased survivin and HIF-1α expression (Figure 2A and 2B). In this regard, the possibility exists that survivin and/or HIF-1α are somehow involved in FSH-stimulated VEGF expression.
The results of the present study show that survivin regulates VEGF and HIF-1α expression and that HIF-1α only regulates VEGF expression. Our investigation further revealed that survivin RNAi was able to antagonize the effect of FSH upregulation of VEGF expression, whereas HIF-1α RNAi did not affect this stimulation. These data suggest that the effect of FSH upregulation of VEGF expression depends on the survivin pathway. Thus, survivin may serve as a major contributing factor in these pathways.
FSH stimulated PI3K/AKT signal transduction in many cells, including granular cells, Sertoli cells, and oocytes 39, 40, 41. FSH has also been shown to activate ERK and p38 mitogen-activated protein kinase (MAPK) in granulose cells 42, 43. Choi et al. 44 found that FSH and LH activated MAPK and PI3K in human OSE cell. Additionally, FSH significantly upregulates the level of protein kinase Cα (PKCα) mRNA and protein, and the PKC pathway has been proposed to play a role in FSH-induced cell proliferation in ovarian cancer cells 27. FSH also stimulates the growth of human OSE and ovarian cancer cells through the PKA and inerleukin-6/signal transducers and activators of transcription 3 (STAT3) signaling pathway 45. The present study shows that FSH stimulated survivin expression through activation of the PI3K/AKT signal transduction pathway in SKOV-3 and ES-2 cells. Our analysis reveals that the expression of AKT or pAKT significantly correlates with the expression of survivin in the ovarian serous cystadenocarcinoma specimens. Moreover, pAKT/AKT expression was found to be correlated with the 2-year and 5-year survival rates. Aberrant activity of the PI3K signaling pathway in human cancer is of great interest. In ovarian cancer, the PI3K signaling pathway plays an important role in proliferation, antiapoptosis, and tumorigenesis 46. Increasing evidence suggests the involvement of PI3K/AKT in cell migration, invasion, and metastasis in normal and neoplastic tissues, including ovarian cancer 28, 47, 48.
Taken together, our results indicate that FSH stimulation of VEGF expression may be mediated through the PI3K/AKT pathway (Figure 7). Further studies to understand the role of FSH in neovascularization on cellular and molecular levels are necessary, as they may help to elucidate the etiology of ovarian cancer development.
Materials and Methods
Ovarian cancer cell lines and human tissue samples
The ovarian serous cancer cell line SKOV-3 and ovarian clear cell cancer cell line ES-2 were obtained from the American Type Culture Collection (Manassas, VA, USA). Both cell lines were cultured in RPMI 1640 culture solution (GIBCO BRL, Gaithersburg, MD, USA) containing 10% calf serum (Sijiqing Co., Shanghai, China) in 5% CO2 at 37 °C.
Eighty-two samples of paraffin-embedded ovarian tumor tissue, consisting of 21 ovarian benign serous cystadenomas, 18 borderline ovarian serous cystadenomas, 26 ovarian serous cystadenocarcinomas, and 17 ovarian clear cell carcinomas, were collected from patients who had undergone surgery from January 2001 to December 2002 in the Obstetrics and Gynecology Hospital of Fudan University in Shanghai, China. None of the patients had a history of other neoplasms or had undergone radiotherapy, chemotherapy, hormone replacement therapy, immunotherapy, or any other therapy before surgery. In addition, clinical characteristics such as age, disease stage, and tumor grade were considered for enrollment (Supplementary information, Table S1). The histological diagnosis and tumor grade were based on the 1986 International Federation of Gynecology and Obstetrics classification system. All of the tissue samples were obtained with the patients' informed consent using protocols and procedures approved by the Institutional Review Board at the Obstetrics and Gynecology Hospital of Fudan University.
Reagents and preparations
FSH, the ERK inhibitor U0126, and the PI3K/AKT inhibitor LY294002 were purchased from Sigma Chemical Co. (St. Louis, MO, USA). Opti-MEM was purchased from GIBCO BRL. A GAPDH monoclonal antibody was purchased from Kangchen Bioengineering Corporation (Shanghai, China); an anti-HIF-1α polyclonal antibody, an ERK antibody, and a phosphorylated ERK (pERK) antibody were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA); an anti-VEGF polyclonal antibody was purchased from Caliches (Darmstadt, Germany), and anti-AKT and anti-pAKT (Thr308) antibodies were purchased from Cell Signaling Technology (Danvers, MA, USA). An anti-survivin monoclonal antibody and human VEGF ELISA kit were purchased from R&D Systems (Minneapolis, MN, USA); infrared fluorescence secondary antibodies were purchased from Rockland Immunochemicals (Gilbertsville, PA, USA). Lipofectamine 2000 transfection reagent and TRIzol reagent were purchased from Invitrogen (Carlsbad, CA, USA); and probes for GAPDH, survivin, HIF-1α, and VEGF and a MIX solution for real-time PCR were purchased from Applied Biosystems (Foster City, CA, USA).
Design and preparation of constructs
Nineteen-nucleotide DNA sequences targeting survivin, HIF-1α, and AKT were obtained from Kangchen Bioengineering Corporation (Shanghai, China), with three sequences targeting survivin (5′-GCA TCT CTA CAT TCA AGA A-3′, 5′-GAA GCA GTT TGA AGA ATT A-3′, and 5′-AGG AAA CCA ACA ATA AGA A-3′), three sequences targeting HIF-1α (5′-CAG TTG CCA CTT CCA CAT A-3′, 5′-AGT TCA CCT GAG CCT AAT A-3′, and 5′-TGC CAC CAC TGA TGA ATT A-3′), and three sequences targeting AKT (5′-GGT GAT CCT GGT GAA GGA G-3′, 5′-GAA GGA AGT CAT CGT GGC C-3′, and 5′-GGA CGG GCA CAT TAA GAT C-3′). The 19-nucleotide oligonucleotide sequence 5′-TTC TCC GAA CGT GTC ACG T-3′, which had no significant homology with any known human mRNA in the GeneBank databases, was used as a negative control. A template was created using synthetic sense and antisense oligonucleotides (Shanghai Sangon Biological, Shanghai, China) for generating RNA composed of two identical 19-nt sequence motifs in an inverted orientation separated by a 19-bp spacer to form a double-stranded hairpin of small interfering RNA. Two micrograms of each oligonucleotide were annealed for 10 min at 95 °C and for 1 h at 37 °C and then ligated into 2 μg of pRNAT-U6.1/Neo plasmid containing the ampicillin resistance gene and the U6 promoter (GenScript, Piscataway, NJ, USA) and linearized with BamHI and HindIII. The 10 shRNA constructs were named pRNAT-suv1, pRNAT-suv2, pRNAT-suv3, pRNAT-hif1, pRNAT-hif2, pRNAT-hif3, pRNAT-akt1, pRNAT-akt2, pRNAT-akt3, and pRNAT-neg and were cloned in TOP10 chemically competent Escherichia coli cells according to the manufacturer's instructions (Invitrogen). The sequence of insert in each shRNA was confirmed by automated sequencing.
Transfection assay for RNAi
Transfection of plasmids was performed with Lipofectamine 2000 (Invitrogen) following the manufacturer's instructions. Briefly, the day before transfection, 5 × 105 SKOV-3 cells per well were plated onto six-well plates and grown for 1 day when the cells had reached 80-85% confluence. The plasmids and Lipofectamine 2000 were each diluted in 250 μL of serum-free Opti-MEM and incubated for 5 min at room temperature. The diluted plasmid and diluted Lipofectamine 2000 were then combined at a ratio of 1:2 (4 μg of plasmid and 8 μL of Lipofectamine 2000). This combination was mixed gently and incubated for 20 min at room temperature. A total of 500 μL of the combination was added to each well in a final volume of 2 mL/well. The cells were incubated for another 48-72 h before the experiments were conducted.
FSH stimulation
Monoplast suspensions of SKOV-3 or ES-2 cells were inoculated into six-well plates at a concentration of 5 × 105 cells/mL and a total volume of 2 mL. At 24 hours after culture, RPMI1640 culture solution without serum was replaced, and the cells were starved for 18 h. Then, the cells were stimulated with FSH at different concentrations (for the VEGF protein assay) or 40 mIU/mL (for the HIF-1α or survivin or pERK/ERK or pAKT/AKT protein assay), and for different time courses; PBS was used as a control. The transfected cells were also starved for 18 h and then stimulated with FSH at 40 mIU/mL for another 24 h on HIF-1α or survivin and 48 h on VEGF. The cells were then harvested and the proteins or mRNA were extracted for western blot, RT-PCR, or real-time PCR analysis.
ELISA for VEGF detection in cell culture supernatants
Monoplast suspensions of SKOV-3 and ES-2 cells were inoculated into 96-well plates at a concentration of 1 × 105 cells/mL and a total volume of 0.2 mL. At 24 h after culture, RPMI 1640 culture solution without serum was replaced, and the cells were starved for 18 h. FSH was added to the wells at 0, 10, 20, 40, 80, or 160 mIU/mL; PBS was used as a control. The monoplast suspensions were cultured for 0, 12, 24, 48, 72, or 96 h, and four parallel reactions were performed in each group. The resulting supernatants were collected, and the VEGF concentration in each sample was measured using ELISA according to the ELISA kit manufacturer's instructions.
Western blot analysis
Cell lysates from culture were collected and quantified using the BCA method. Following 8%, 12%, and 15% denaturation sodium dodecyl sulfate-polyacrylamide gel electrophoresis, 30 μg of protein lysates was separated from the gel and transferred to a nitrocellulose filter. The membranes were sealed with PBS containing 5% non-fat milk for 1 h at room temperature, sealed with a primary antibody overnight at 4 °C, and mixed with an infrared fluorescence secondary antibody for 1 h the next day at 37 °C; GAPDH was used as a loading control. The signal was detected, and the protein was analyzed semiquantitatively using the Odyssey infrared fluorescence scanning system (LI-COR. Inc., Lincoln, NE, USA).
RNA extraction and RT-PCR
Total cellular RNA was extracted from cells using the TRIzol reagent according to the manufacturer's instructions. cDNA was synthesized from 2 μg of RNA using a reverse transcription kit (Promega, Madison, WI, USA) and PCR primers by Yingjun Biotechnology Corporation (Shanghai, China). The VEGF upstream primer 5′-CCT TGC TGC TCT ACC TCC AC-3′ and downstream primer 5′-ATC TGC ATG GTG ATG TTG GA-3′ (288 bp) and the GAPDH upstream primer 5′-ACC ACA GTC CAT GCC ATC AC-3′ and downstream primer 5′-CCA CCA CCC TGT TGC TGT AG-3′ (450 bp) were used in the PCRs. The PCR conditions were as follows: 94 °C for 5 min; 94 °C for 45 s, 60 °C for 45 s, and 72 °C for 45 s for 30 cycles; and 72 °C for 10 min. In all, 20 μL of the PCR product was used for agarose electrophoresis.
Real-time PCR
The probes (Applied Biosystems) were all assay-on-demand products and specific for VEGF, HIF-1α, survivin, and GAPDH. Their product numbers were as follows: VEGF, Hs00173626_m1; HIF-1α, Hs00153153_m1; survivin, Hs00153353_m1; and GAPDH, Hs99999905_m1. Real-time PCR analysis was conducted using the Applied Biosystems 7000 Sequence Detection System equipped with a 96-well optical reaction plate. The reactions were set up using 10 μL of TaqMan Universal PCR Master Mix (Applied Biosystems), 2 μL of TaqMan probes (Applied Biosystems), 3 μL of a cDNA template, and 5 μL of ddH2O. The real-time PCR conditions were as follows: 50 °C for 2 min followed by 95 °C for 10 min, 40 cycles at 95 °C for 15 s, and 60 °C for 1 min. All real-time experiments were carried out in triplicate, and a mean value was employed for determination of mRNA expression levels. A negative control containing water instead of sample cDNA was applied to each real-time plate. At the end of the PCR, the threshold value (CT) for each of these genes was set using the ABI PRISM 7000 software program (Foster City, CA), and the calculated CT values were exported to the SPSS software program (version 11.0; SPSS Inc., Chicago, IL, USA) for analysis. The relative expression of mRNA was calculated using the comparative CT method according to the manufacturer's instructions (Applied Biosystems).
Detection of signals in the PI3K/AKT pathway
For inhibitory assays, SKOV-3 or ES-2 cells were grown as described above, and LY294002 and U0126 (both at a concentration of 10 μmol/L) were added to the culture supernatants. After 30 min, 40 mIU/mL FSH was added to the cells; PBS was used as a control. The cells were then harvested. The proteins were extracted from the cells 30 min later for PI3K/AKT or MAPK/ERK phosphorylation assay, or 24 h later for survivin protein assay.
Immunohistochemical analysis
The expression of AKT, pAKT, survivin, and VEGF in paraffin-embedded clinical tissue samples was examined using the avidin-biotin complex immunoperoxidase method. Deparaffinized sections of the tissue were treated with 3% hydrogen peroxide to block endogenous peroxidase activity. Next, the sections were blocked with 5% normal serum for 20 min, and an anti-AKT antibody (1:500 dilution) or anti-pAKT antibody (1:200 dilution) was applied to them for incubation overnight at 4 °C. After being rinsed three times with PBS, the sections were treated with biotinylated secondary antibody avidin-biotin complex/horseradish peroxidase (Dako A/S, Glostrup, Denmark). The peroxidase activity in the tissue samples was visualized by applying diaminobenzidine chromogen to them. The sections were then counterstained with hematoxylin. A rabbit or mouse IgG alone was used as a negative control for immunostaining, and slides containing colon tumor tissue were used as positive controls based on the manufacturer's (Dako) instructions. Two independent investigators evaluated the immunohistochemical staining. The staining intensity was examined in a semiquantitative assessment of the immunohistochemical results, and the percentage of stained tumor cells was graded as negative (≤5%) or positive (>6%).
Statistical analysis
The results of all of the experiments were analyzed using the χ2 test for positive rate comparison and one-way analysis of variance for the other comparisons. Differences were considered to be significant at p < 0.05. The 5-year survival curve was analyzed using the Kaplan-Meier product-limit method. The SPSS software program (version 11.0) was used for all statistical analysis.
(Supplementary information is linked to the online version of the paper on the Cell Research website.)
References
Ozols RF, Bookman MA, Connolly DC, et al. Focus on epithelial ovarian cancer. Cancer Cell 2004; 5:19–24.
Risch HA, Marrett LD, Jain M, Howe GR . Differences in risk factors for epithelial ovarian cancer by histologic type. Results of a case-control study. Am J Epidemiol 1996; 144:363–372.
Ferrara N . Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am J Physiol Cell Physiol 2001; 280:C1358–C1366.
Carmeliet P . Angiogenesis in health and disease. Nat Med 2003; 9:653–660.
Anonynous . Translational research: the role of VEGF in tumor angiogenesis. Proceedings of a symposium. Oncologist 2000; 5:1–57.
Xia C, Meng Q, Cao Z, et al. Regulation of angiogenesis and tumor growth by p110 alpha and AKT1 via VEGF expression. J Cell Physiol 2006; 209:56–66.
Skinner HD, Zheng JZ, Fang J, Agani F, Jiang BH . Vascular endothelial growth factor transcriptional activation is mediated by hypoxia-inducible factor 1alpha, HDM2, and p70S6K1 in response to phosphatidylinositol 3-kinase/AKT signaling. J Biol Chem 2004; 279:45643–45651.
Choi KS, Bae MK, Jeong JW, Moon HE, Kim KW . Hypoxia-induced angiogenesis during carcinogenesis. J Biochem Mol Biol 2003; 36:120–127.
Jung YJ, Isaacs JS, Lee S, Trepel J, Neckers L . IL-1beta-mediated up-regulation of HIF-1alpha via an NFkappaB/COX-2 pathway identifies HIF-1 as a critical link between inflammation and oncogenesis. FASEB J 2003; 17:2115–2117.
Pore N, Jiang Z, Gupta A, Cerniglia G, Kao GD, Maity A . EGFR tyrosine kinase inhibitors decrease VEGF expression by both hypoxia-inducible factor (HIF)-1-independent and HIF-1-dependent mechanisms. Cancer Res 2006; 66:3197–3204.
Ding J, Li J, Chen J, et al. Effects of polycyclic aromatic hydrocarbons (PAHs) on vascular endothelial growth factor induction through phosphatidylinositol 3-kinase/AP-1-dependent, HIF-1alpha-independent pathway. J Biol Chem 2006; 281:9093–9100.
Altieri DC . Survivin, versatile modulation of cell division and apoptosis in cancer. Oncogene 2003; 22:8581–8589.
Conway EM, Zwerts F, Van Eygen V, et al. Survivin-dependent angiogenesis in ischemic brain: molecular mechanisms of hypoxia-induced up-regulation. Am J Pathol 2003; 163:935–946.
Mesri M, Morales-Ruiz M, Ackermann EJ, et al. Suppression of vascular endothelial growth factor-mediated endothelial cell protection by survivin targeting. Am J Pathol 2001; 158:1757–1765.
O'Connor DS, Schechner JS, Adida C, et al. Control of apoptosis during angiogenesis by survivin expression in endothelial cells. Am J Pathol 2000; 156:393–398.
Tanaka K, Iwamoto S, Gon G, et al. Expression of survivin and its relationship to loss of apoptosis in breast carcinomas. Clin Cancer Res 2000; 6:127–134.
Venn A, Watson L, Bruinsma F, et al. Risk of cancer after use of fertility drugs with in vitro fertilization. Lancet 1999; 354:1586–1590.
Brekelmans CT . Risk factors and risk reduction of breast and ovarian cancer, Curr Obstet Gynecol 2003; 15:63–68.
Daly M, Obrams GI . Epidemiology and risk assessment for ovarian cancer. Semin Oncol 1998; 25:255–264.
Gnagy S, Ming EE, Devesa SS, et al. Declining ovarian cancer rates in U.S. women in relation to parity and oral contraceptive use. Epidemiology 2000; 11:102–105.
Zheng W, Lu JJ, Luo F, et al. Ovarian epithelial tumor growth promotion by follicle-stimulating hormone and inhibition of the effect by luteinizing hormone. Gynecol Oncol 2000; 76:80–88.
Parrott JA, Doraiswamy V, Kim G, et al. Expression and actions of both the follicle stimulating hormone receptor and the luteinizing hormone receptor in normal ovarian surface epithelium and ovarian cancer. Mol Cell Endocrinol 2001; 172:213–222.
Halperin R, Pansky M, Vaknin Z, et al. Luteinizing hormone in peritoneal and ovarian cyst fluids: a predictor of ovarian carcinoma. Eur J Obstet Gynecol Reprod Biol 2003; 110:207–210.
Rzepka-Górska I, Chudecka-G³az A, Kosmowska B . FSH and LH serum/tumor fluid ratios and malignant tumors of the ovary. Endocr Relat Cancer 2004; 11:315–321.
Syed V, Ulinski G, Mok SC, et al. Expression of gonadotropin receptor and growth responses to key reproductive hormones in normal and malignant human ovarian surface epithelial cells. Cancer Res 2001; 61:6768–6776.
Choi KC, Kang SK, Tai CJ, et al. Follicle stimulating hormone activates mitrogen-activated protein kinase in preneoplastic and neoplastic ovarian surface epithelial cells. J Clin Endocrinol Metab 2002; 87:2245–2253.
Ohtani K, Sakamoto H, Kikuchi A, et al. Follicle-stimulating hormone promotes the growth of human epithelial ovarian cancer cells through the protein kinase C-mediated system. Cancer Lett 2001; 166:207–213.
Choi JH, Choi KC, Auersperg N, Leung PC . Gonadotropins activate proteolysis and increase invasion through protein kinase A and phosphatidylinositol 3-kinase pathways in human epithelial ovarian cancer cells. Cancer Res 2006; 66:3912–3920.
Stadel BV . Letter: the etiology and prevention of ovarian carcinoma cells. Cancer Res 2001; 61:8340–8346.
Feng YJ, Zhang XY, Ge BQ . Gonadotropins stimulate the proliferation of human epithelial ovarian cancer cell. Zhonghua Fu Chan Ke Za Zhi 1996; 31:166–168.
Zhu MW, Wu QY, Ge BQ, et al. The dose response of cell proliferation and secretion of CA125 II antigen to follicle stimulation hormone in ovarian cancer cell lines. Zhonghua Fu Chan Ke Za Zhi 1998; 33:225–226.
Ji Q, Liu PI, Chen PK, et al. Follicle stimulating hormone-induced growth promotion and gene expression profiles on ovarian surface epithelial cells. Int J Cancer 2004; 112:803–814.
Choi JH, Choi KC, Auersperg N, et al. Overexpression of follicle-stimulating hormone receptor activates oncogenic pathways in preneoplastic ovarian surface epithelial cells. J Clin Endocrinol Metab 2004; 89:5508–5516.
Schiffenbauer YS, Meir G, Maoz M, et al. Gonadotropin stimulation of MLS human epithelial ovarian carcinoma cells augments cell adhesion mediated by CD44 and by alpha(v)-integrin. Gynecol Oncol 2002; 84:296–302.
Schiffenbauer YS, Abramovitch R, Meir G, et al. Loss of ovarian function promotes angiogenesis in human ovarian carcinoma. Proc Natl Acad Sci USA 1997; 94:13203–13208.
Wang J, Luo F, Lu JJ, Chen PK, Liu P, Zheng W . VEGF expression and enhanced production by gonadotropins in ovarian epithelial tumors. Int J Cancer 2002; 97:163–167.
Huang CF, Liu DY, Shen K . Follicle stimulating hormone inhibits cisplatin induced apoptosis in ovarian cancer cells. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2003; 25:447–450.
Huang CF, Liu DY, Xu WH, et al. Protective effect of follicle stimulating hormone on apoptosis of human epithelial ovarian cancer cell induced by cisplatin. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2003; 25:443–446.
Alam H, Maizels ET, Park Y, et al. Follicle-stimulating hormone activation of hypoxia-inducible factor-1 by the phosphatidylinositol 3-kinase/AKT/Ras homolog enriched in brain (Rheb)/mammalian target of rapamycin (mTOR) pathway is necessary for induction of select protein markers of follicular differentiation. J Biol Chem 2004; 279:19431–19440.
Carvalho CR, Carvalheira JB, Lima MH, et al. Novel signal transduction pathway for luteinizing hormone and its interaction with insulin: activation of Janus kinase/signal transducer and activator of transcription and phosphoinositol 3-kinase/Akt pathways. Endocrinology 2003; 144:638–647.
Meroni SB, Riera MF, Pellizzari EH, Galardo MN, Cigorraga SB . FSH activates phosphatidylinositol 3-kinase/protein kinase B signaling pathway in 20-day-old Sertoli cells independently of IGF-I. J Endocrinol 2004; 180:257–265.
Gebauer G, Peter AT, Onesime D, et al. Apoptosis of ovarian granulosa cells: correlation with the reduced activity of ERK-signaling module. J Cell Biochem 1999; 75:547–554.
Maizels ET, Cottom J, Jones JC, et al. Follicle stimulating hormone (FSH) activates the p38 mitogen-activated protein kinase pathway, including small heat shock protein phosphorylation and cell rounding in immature rat ovarian granulose cells. Endocrinology 1998; 139:3353–3356.
Choi JH, Choi KC, Auersperg N, et al. Gonadotropins upregulate the epidermal growth factor receptor through activation of mitogen-activated protein kinases and phosphatidyl-inositol-3-kinase in human ovarian surface epithelial cells. Endocr Relat Cancer 2005; 12:407–421.
Syed V, Ulinski G, Mok SC, et al. Reproductive hormone-induced, STAT3-mediated interleukin 6 action in normal and malignant human ovarian surface epithelial cell. J Natl Cancer Inst 2002; 94:617–629.
Vara JAF, Casado E, de Castro J, et al. PI3K/Akt signaling pathway and cancer. Cancer Treat Rev 2004; 30:193–204.
Park BK, Zeng X, Glazer RI . Akt1 induces extracellular matrix invasion and matrix metalloproteinase-2 activity in mouse mammary epithelial cell. Cancer Res 2001; 61:7647–7653.
Liu LZ, Hu XW, Xia C, et al. Reactive oxygen species regulate epidermal growth factor-induced vascular endothelial growth factor and hypoxia-inducible factor-1alpha expression through activation of AKT and P70S6K1 in human ovarian cancer cells. Free Radic Biol Med 2006; 41:1521–1533.
Acknowledgements
We thank Zhen Liu Liang for editing this manuscript. This work was supported by Shanghai Key Subject Construction Project 05-III-016, Shanghai Health Bureau Key Project 05-ZD-001, and Shanghai Leading Academic Discipline Project B117.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary information, Table S1
Patient characteristics (PDF 30 kb)
Rights and permissions
About this article
Cite this article
Huang, Y., Hua, K., Zhou, X. et al. Activation of the PI3K/AKT pathway mediates FSH-stimulated VEGF expression in ovarian serous cystadenocarcinoma. Cell Res 18, 780–791 (2008). https://doi.org/10.1038/cr.2008.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.2008.70
Keywords
This article is cited by
-
Circular RNAs in the tumour microenvironment
Molecular Cancer (2020)
-
Progranulin expression induced by follicle-stimulating hormone in ovarian cancer cell lines depends on the histological subtype
Medical Oncology (2020)
-
Follicle-stimulating hormone promoted pyruvate kinase isozyme type M2-induced glycolysis and proliferation of ovarian cancer cells
Archives of Gynecology and Obstetrics (2019)
-
Optimal FSH usage in revascularization of allotransplanted ovarian tissue in mice
Journal of Ovarian Research (2017)
-
Administration of follicle-stimulating hormone induces autophagy via upregulation of HIF-1α in mouse granulosa cells
Cell Death & Disease (2017)